1. Background
Mask ventilation is one of the most important aspects of managing and maintaining a patient's airway. It is the most fundamental technique that can maintain sufficient oxygenation and be lifesaving in an apneic patient by preventing brain injury and cardiovascular failure, especially when intubation is difficult and unsuccessful (1, 2).
Most suggested definitions for difficult mask ventilation are binary (difficult or not difficult), while patients mostly fall on a spectrum between these two ends. Thus, a graded definition is more useful clinically. Although a standard and widely accepted definition for difficult mask ventilation does not exist, such classification systems have been proposed (1). The American Society of Anesthesiology defined difficult mask ventilation as the inability of a trained anesthetist to maintain the oxygen saturation level above 90% by using facemask ventilation (while the patient's initial saturation level is in the normal range) (3). Han et al. developed and defined a classification and scale with grades 0-4 for difficult mask ventilation in 2004 (4).
Patient-related and non-patient-related factors can cause difficult mask ventilation. Considering etiology, difficult mask ventilation is caused by one or more of the three following categories: Inadequate mask seal, increased airway resistance, and decreased respiratory compliance. Several factors can lead to a poor mask seal, including improper mask size or positioning, inappropriate mask shape/design, facial hair, edentulism, maxillomandibular deformities such as micrognathia, and foreign objects (e.g., nasogastric tubes). Increased airway resistance can occur in the upper airway caused by tonsillar and adenoidal hypertrophy, redundant soft tissue, large tongue or epiglottis, airway edema, oropharyngeal tumors, external compression (e.g., large neck mass or hematoma) and laryngospasm. It can also occur in the lower airway as a result of airway secretions, excessively applied cricoid pressure, foreign body, tracheomalacia, tracheal stenosis, airway or mediastinal mass, and bronchospasm. Decreased respiratory compliance causes difficult mask ventilation by increasing distal pressure. Contributing factors include inadequate depth of anesthesia or inadequate paralysis (i.e., ventilation asynchrony), restrictive lung disease (such as pulmonary fibrosis or ARDS), chest wall deformity (e.g., severe kyphoscoliosis), obesity, abdominal compartment syndrome, pregnancy, external compression (e.g., orthotics), and tension pneumothorax (1, 5).
Different studies have offered distinct techniques to optimize mask ventilation. Choosing the appropriate mask size that fits the patient's face is always recommended. Optimizing the mask-holding technique is one of the factors that can reduce difficulty in mask ventilation (1). Several methods have been described for holding a face mask to achieve an adequate seal, including the commonly employed C-E clamp, the double C-E technique, the two-handed V-E technique, the EO technique, and many others (1, 6). Some studies have introduced different techniques for holding the face mask in children as well, such as the three-finger grip, the spider hold (7), and the glass holding technique (8). However, not enough evidence exists to show the superiority of one of these techniques over the others in infants.
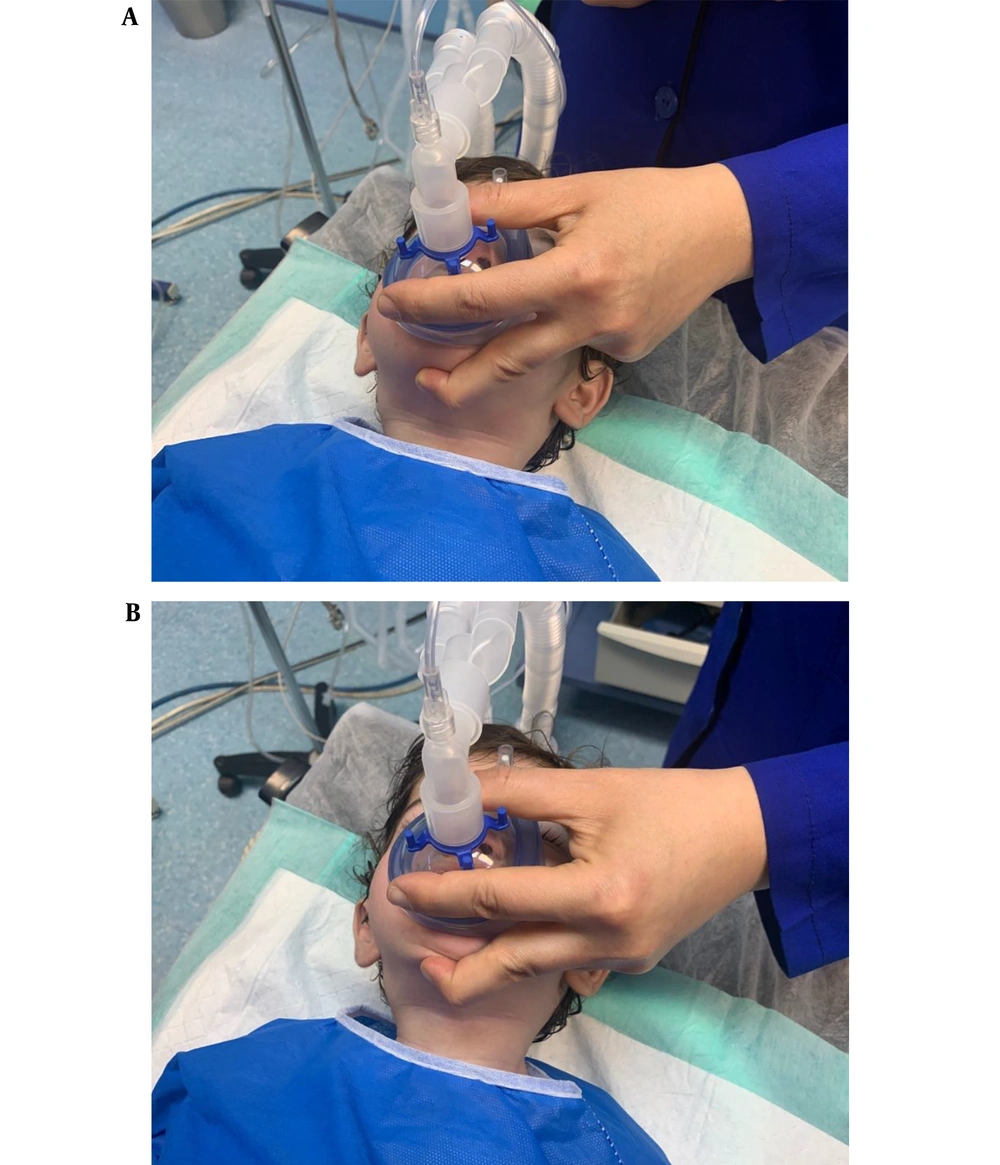
Considering the smaller size and different anatomy of the infants' faces, developing and applying techniques different from the ones used in adults seems to be necessary for children to find the best mask-holding method in this group of patients. In spite of being the most commonly used technique in infants, the three-finger grip technique fails to provide optimal ventilation in some instances. In this study, we compared the quality of ventilation between two different mask-holding techniques in infants: The three-finger grip that has been described before and is used commonly and the three-finger grip with the application of a new maneuver we devised ourselves called the submental maneuver. None of the previous studies comparing expired tidal volume (VTE) between different mask-holding techniques have compared these two techniques so far. The three-finger grip is very much like the C-E clamp technique. The thumb and index finger are placed on the rim of the mask, forming a C shape, and the middle finger is placed on the chin protuberance to lift the chin. The ring and the little fingers are flexed onto the palm and are non-functional in this technique (Figure 1A). The submental maneuver is performed by holding and pulling the submental soft tissue upward with the middle finger while maintaining pressure on the chin protuberance (Figure 1B). We hypothesized that this maneuver can enhance ventilation by pulling the hyoid bone anteriorly and thus can open and maintain the airway more effectively.
Face mask-holding techniques. A, three-finger grip; B, three-finger grip plus the submental maneuver. With the three-finger grip, the thumb and index finger are placed on the rim of the mask, forming a C shape, and the middle finger is placed on the chin protuberance to lift the chin, while the ring and little fingers are flexed onto the palm and are non-functional in this technique. The submental maneuver is performed by holding and pulling the submental soft tissue upward with the middle finger while maintaining pressure on the chin protuberance.
2. Objectives
The purpose of this study was to compare these two different mask-holding techniques in infants, with the primary outcome being VTE.
3. Methods
3.1. Patient Enrollment and Exclusion Criteria
Infants under 1 year of age in the ASA classification 1 and 2 who were candidates for elective surgery (pediatrics' general surgeries, specifically hernia and hydrocele surgeries) under general anesthesia at Tehran Children's Medical Center between December 19, 2021, and February 6, 2022, were recruited for this study (ASA class 1: A normal healthy patient, ASA class 2: A patient with mild systemic disease). Patients who had any of the following were excluded from the study: The presence of maxillofacial anomalies, chest wall deformity, past medical history of any respiratory disease, and any foreign object interfering with mask ventilation. Ethical approval was obtained from the Ethics Committee of Tehran Children's Medical Center (reference number: IR.TUMS.CHMC.REC.1400.024). Also, this clinical trial was approved by and registered on the Iranian Registry of Clinical Trials (IRCT) website (IRCT Id: IRCT20221114056498N1).
3.2. Sample Size and Randomization
The required sample size for this study was calculated as 90, using the mean VTE and standard deviations measured by Gerstein et al. (m1 = 269, SD1 = 197, m2 = 379, SD2 = 172) (9). Subjects were randomized into two blocks using the website www.randomization.com before beginning the investigation. Forty-five numbers out of numbers 1 - 90 were allocated randomly to each intervention group (group 1: Three-finger grip technique, group 2: Three-finger grip with the submental maneuver). The number and its assigned technique were inserted in the data collection form for each patient. For example, it was specified that for patient number 4, the three-finger grip technique would be performed.
3.3. Blinding
Parents or guardians of the infants were unaware of the group assignment. Only the researcher performing mask ventilation was aware of the groups. The monitor displayed the parameters to be studied, and the hyperinflation bag was positioned in a way that the researcher could not see them. Thus, the researcher was unaware of these parameters while holding the mask. The person in charge of collecting the data was not only unaware of the mask-holding technique for each patient but also positioned in a place that could not see the technique used by the researcher performing mask ventilation.
3.4. Study Design
In this interventional double-blind randomized controlled trial (RCT), written informed consent was obtained from the infants' parents or guardians. The face mask was connected to a circle breathing system (Altech® pediatric breathing circuit corrugated with water trap reference No. Al-1411.v002, Izmir, Turkey). After connecting the standard monitoring devices, general anesthesia was induced with 8% sevoflurane and 100% oxygen (flow = 2 - 3 lit/min) by the Dräger Fabius® Plus anesthesia machine (Drägerwerk AG & Co. KGaA, Lübeck, Germany) using one of the mask-holding techniques (three-finger grip technique or three-finger grip plus submental maneuver) in the neutral position. After the patient was anesthetized and fell asleep within the first few seconds to one minute, the concentration of sevoflurane was reduced from 8% to 3.5% and maintained at this level. When the appropriate depth of anesthesia was reached, the anesthetist inserted an intravenous line, and the patient was intubated following administration of intravenous anesthetic drugs (sodium thiopental 5 mg/kg and fentanyl 1 mcg/kg). Spontaneous breathing was maintained for patients during the induction phase, and assisted ventilation was not performed. The duration of this process differed for each patient but fell in the range of 6 to 8 minutes. Demographic data (age, sex, weight, and height) for each patient was collected from their medical records. Quantitative hemodynamic parameters [systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse rate (PR), O2 saturation (SpO2), and end-tidal CO2 pressure (Et CO2)] were measured. Also, VTE was assessed quantitatively by the Drager machine and then classified into three groups of patient's quality of breath flow as either good, fair, or bad for VTE in the range of 5 - 7 mL/kg, 3 - 5 mL/kg, and < 3 mL/kg, respectively (10). Abnormal respiratory sounds and respiratory distress were evaluated by a single experienced anesthesiologist during mask ventilation. If any of the following situations occurred for a patient, the study was terminated, and necessary measures were taken: O2 saturation drop below 95%, failure to manage the patient's airway, and the need to intubate the patient immediately.
3.5. Data Analysis
The data were analyzed using the IBM SPSS Statistics software version 26. Descriptive data for continuous variables are presented as mean ± standard deviation (SD). Categorical variables are presented as absolute numbers and frequencies. Continuous variables were compared by independent sample t-test. Categorical data were analyzed using the chi-square test. P-values < 0.05 were considered statistically significant.
4. Results
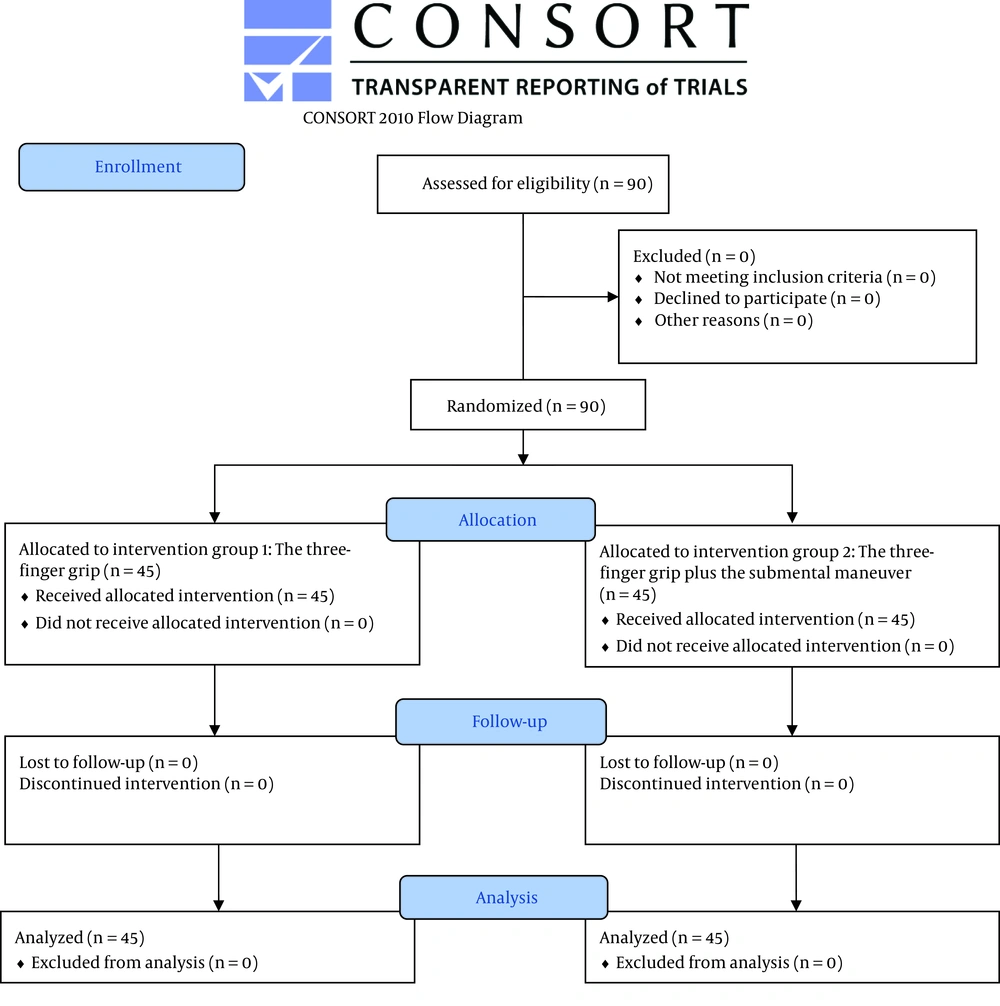
Ninety patients were enrolled in this study (Figure 2, Table 1). Regarding sex, age, weight, and height, no significant difference existed between the two study groups. The primary outcome of this study (VTE), assessed as the quality of the patient's breath flow, was compared between the two techniques. Good, fair, and bad qualities were recorded for 30 (66.67%), 15 (33.33%), and 0 patients in the three-finger grip technique and 39 (86.67%), 6 (13.33%), and 0 patients in the submental maneuver group, respectively. A chi-square test was performed to analyze the relationship between the mask-holding technique and VTE (P-value = 0.025).
| Variables | Overall (N = 90) | Three-Finger Grip (N = 45) | Submental Maneuver b (N = 45) |
|---|---|---|---|
| Sex | |||
| Male | 74 (82.22) | 36 (80) | 38 (84.44) |
| Female | 16 (17.78) | 9 (20) | 7 (15.56) |
| Age (month) | 7.361 ± 4.1218 | 7.611 ± 4.2798 | 7.111 ± 3.9899 |
| Weight (kg) | 8.074 ± 2.6877 | 8.042 ± 2.6359 | 8.107 ± 2.768 |
| Height (cm) | 66.43 ± 10.138 | 66.93 ± 10.049 | 65.93 ± 10.316 |
| BMI (kg/m2) | 17.844 ± 3.31333 | 17.5103 ± 3.18902 | 18.1778 ± 3.4363 |
Abbreviations: BMI, body mass index; SD, standard deviation.
a Values are expressed as No. (%) or mean ± SD.
b Three-finger grip plus the submental maneuver.
Mean values of SpO2, Et CO2, PR, SBP, and DBP were calculated for each group and compared using the independent sample t-test. The results are represented in Table 2.
| Variables | Overall (N = 90) | Three-Finger Grip (N = 45) | Submental Maneuver b (N = 45) | P-Value | 95% CI |
|---|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 89.49 ± 14.566 | 89.69 ± 14.370 | 89.29 ± 14.919 | 0.897 c | -5.736, 6.536 |
| Diastolic blood pressure (mmHg) | 49.70 ± 13.001 | 50.24 ± 14.391 | 49.16 ± 11.584 | 0.694 c | -4.384, 6.562 |
| Pulse rate (bpm) | 135.59 ± 12.902 | 135.24 ± 12.112 | 135.93 ± 13.776 | 0.802 c | -6.123, 4.745 |
| SpO2 (%) | 99.34 ± 11.531 | 99.40 ± 0.809 | 99.29 ± 0.991 | 0.562 c | -0.268, 0.490 |
| Et CO2 (mmHg) | 34.26 ± 11.531 | 33.96 ± 12.040 | 34.56 ± 11.126 | 0.807 c | -5.457, 4.257 |
| Auscultation | 0.593 d | ||||
| No abnormal sound | 66 (73.33) | 33 (73.33) | 33 (73.33) | ||
| Wheeze | 23 (25.56) | 12 (26.67) | 11 (24.44) | ||
| Crackle | 1 (1.11) | 0 (0) | 1 (2.22) | ||
| Respiratory distress | 1.0 d | ||||
| None | 88 (97.78) | 44 (97.78) | 44 (97.78) | ||
| Usage of accessory muscles | 2 (2.22) | 1 (2.22) | 1 (2.22) |
Abbreviations: CI, confidence interval; SD, standard deviation; SpO2, O2 saturation; Et CO2, end-tidal CO2 pressure.
a Values are expressed as No. (%) or mean ± SD unless otherwise indicated.
b Three-finger grip plus the submental maneuver.
c P-value calculated using the independent sample t-test.
d P-value calculated using the chi-square test.
The presence of abnormal respiratory sounds and respiratory distress were evaluated for each patient and compared between the two techniques using the chi-square test (Table 2).
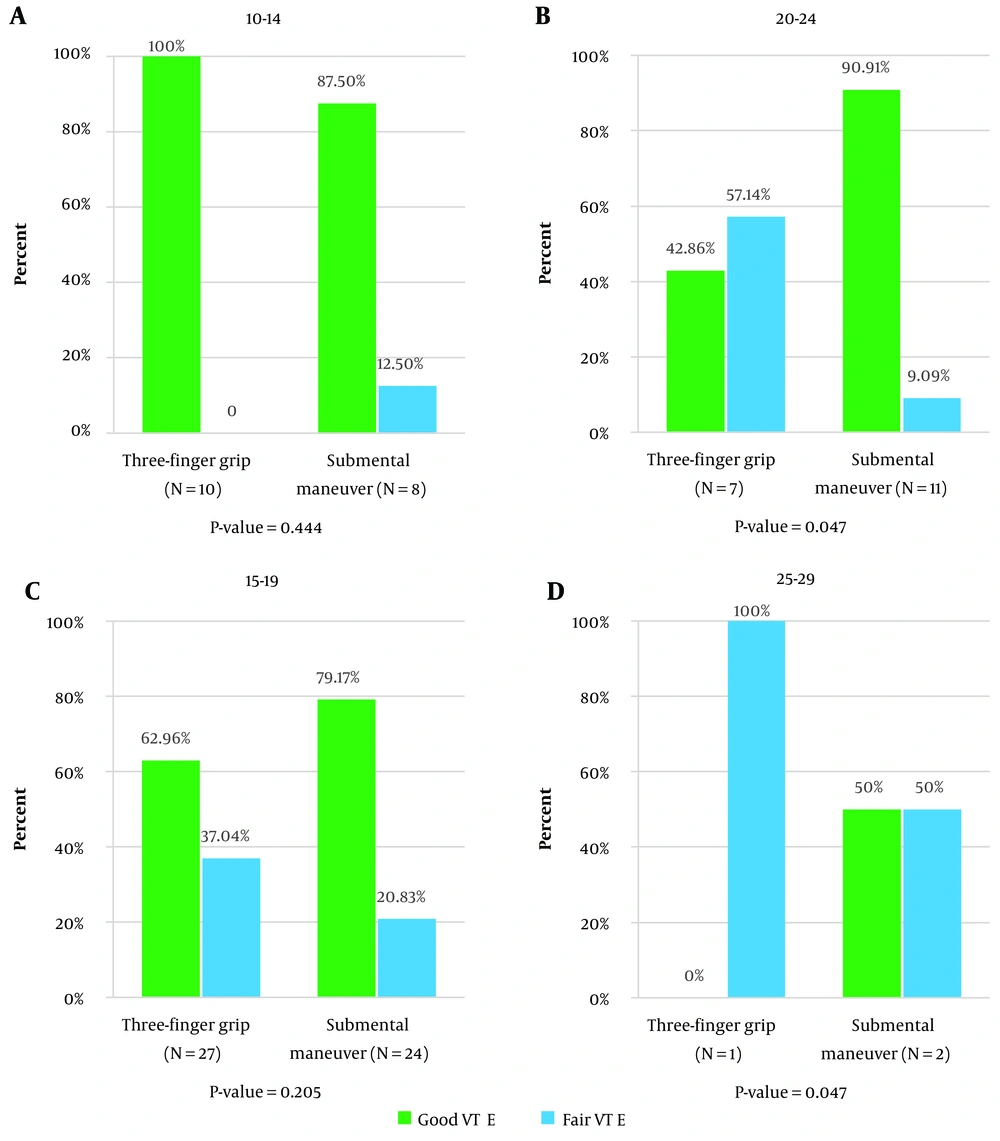
The relationship between VTE and sex, age, and BMI was also analyzed in the whole sample and each group separately (Table 3). Furthermore, in order to evaluate the correlation between VTE and increasing BMI, patients were categorized into four BMI groups. Then, VTE was compared between the two techniques within each group (Figure 3).
| Mask-Holding Technique | Good VTE (N = 69) | Fair VTE (N = 21) | P-Value | 95% CI |
|---|---|---|---|---|
| Three-finger grip | 30 (43.48) | 15 (71.43) | ||
| Sex | 0.02 b | |||
| Male | 21 (70) | 15 (100) | ||
| Female | 9 (30) | 0 (0) | ||
| Age (month) | 6.9 ± 4.442 | 9.033 ± 3.6668 | 0.116 c | -0.5485, 4.8152 |
| BMI (kg/m2) | 16.4501 ± 2.87687 | 19.6308 ± 2.75536 | 0.001 c | 1.37093, 4.99056 |
| Submental maneuver d | 39 (56.52) | 6 (28.57) | ||
| Sex | 0.23 b | |||
| Male | 34 (87.18) | 4 (66.67) | ||
| Female | 5 (12.82) | 2 (33.33) | ||
| Age (month) | 6.923 ± 4.0025 | 8.333 ± 4.0332 | 0.427 c | -2.1327, 4.9532 |
| BMI (kg/m2) | 18.0265 ± 3.34679 | 19.1612 ± 4.17669 | 0.458 c | -1.91948, 4.18901 |
| Overall | ||||
| Sex | 0.342 b | |||
| Male | 55 (79.71) | 19 (90.48) | ||
| Female | 14 (20.29) | 2 (9.52) | ||
| Age (month) | 6.913 ± 4.1674 | 8.833 ± 3.6856 | 0.61 c | -0.092, 3.9326 |
| BMI (kg/m2) | 17.3411 ± 3.22625 | 19.4967 ± 3.11815 | 0.008 c | -0.5697, 3.74145 |
Abbreviations: VTE, expired tidal volume; CI, confidence interval; SD, standard deviation; BMI, body mass index.
a Values are expressed as No. (%) or mean ± SD unless otherwise indicated.
b P-value calculated using the chi-square test.
c P-value calculated using the independent sample t-test.
d Three-finger grip plus the submental maneuver.
5. Discussion
Proper mask ventilation is the first and most important measure in managing the airway, especially in case of an emergency (1). The importance of effective mask ventilation becomes even more significant when it comes to infants, given their heightened vulnerability to hypoxia and their unique anatomical characteristics. Infants have relatively large tongues and epiglottises, larger heads, and a higher and more anterior position of the larynx (11). The incidence of difficult mask ventilation is estimated to be around 6.6% in infants (12). Healthcare professionals must be familiar with more than just one technique for holding the mask so that they can achieve efficient ventilation by trying out different techniques when needed, especially when facing an emergency. In spite of several novel techniques being introduced for holding the face mask in children, none of them has shown to be superior to others (7, 8). Thus, further effort is necessary to develop and find a new mask-holding technique that improves ventilation in infants.
In order to determine the efficacy of mask ventilation, we examined the primary outcome of VTE in our study. Studies performed by Gerstein et al. (9), Jain et al. (13), Fei et al. (14), and Rajappa et al. (15) also used VTE as their primary outcome. In the current study, we have shown that adding the submental maneuver to the three-finger grip technique provides statistically significantly better VTE compared to the three-finger grip alone. This is in line with the results of similar studies that have compared VTE between a conventionally used technique and one or two non-conventional techniques, with VTE being better significantly in the non-conventional ones (9, 13-15).
There are several reasons why the submental maneuver causes better ventilation in infants. For effective mask ventilation, lifting the pharyngeal structures anteriorly to relieve potential obstruction of the airway is important. With the three-finger grip alone, this is achieved by the middle finger placed on the chin protuberance, thereby performing the chin lift. Alternatively, the middle finger also pulls the submental soft tissue upward while maintaining pressure on the chin protuberance in the submental maneuver, which may cause the airway to open more effectively by pulling the hyoid bone anteriorly. Another possible explanation for this effect is that the face and the mask are drawn closer together in the submental maneuver, creating a better mask seal.
Interestingly, comparing VTE between the two techniques within each group of BMI showed that in the BMI group of 20 - 24, the quality of breath flow was significantly better statistically in the submental maneuver compared with the three-finger grip (Figure 3). Hence, our data support the idea that a larger submental soft tissue can be more beneficial in performing the submental maneuver. It effectively opens the airway and improves ventilation quality in infants with a higher BMI and larger submental soft tissue. The above data also collectively show that no meaningful relationship existed between VTE and sex and age (Table 3).
Two other variables that we did not measure, called peak inspiratory pressure (PIP) and failure rate for mask ventilation, were also investigated by Gerstein et al. (9) and Fei et al. (14), respectively. The PIP values did not differ between the C-E and T-E techniques in Gerstein et al.'s study (9). In Fei et al.'s study (14), the V-E technique was superior to the C-E technique, with failure rates for mask ventilation being 44% for the C-E technique and 0% for the V-E technique (P < 0.001).
Taken together, our results suggest that no statistically significant difference existed in the hemodynamic parameters (SBP, DBP, and PR) between the two techniques and that both techniques establish acceptable cardiovascular stability (Table 2). Regarding the quantitative respiratory parameters (SpO2 and Et CO2) and the presence of abnormal respiratory sounds and respiratory distress, no significant difference was shown between the two techniques (Table 2). Thus, these findings suggest that both of these techniques provide appropriate oxygenation and ventilation and are safe in this group of patients.
Our study has some limitations. First, the unpredictable nature of the operating room and possible uncontrolled factors may have influenced the results and outcome of our study. Second, this was a single-center study, which may limit the validity of our results.
5.1. Conclusions
Adding the submental maneuver to the three-finger grip technique seems to provide better expired tidal volume in infants. Also, it seems that in children with higher BMI and larger submental soft tissue, the submental maneuver provides better ventilation quality and can be of help, especially in cases of difficult mask ventilation in infants. So, it is of utmost importance to have different mask-holding techniques in mind and be prepared for the various airway conditions. None of the two techniques investigated in this study have a significant effect on hemodynamic variables, and both are safe for face mask ventilation in infants regardless of age and sex.
We recommend that future research study these two techniques in children of a different age range from a multi-center setting with a greater sample size.