1. Background
Helicobacter pylori infection affects more than 50% of the world's population and is the primary cause of duodenal and gastric ulcers, as well as gastric cancer (1). Children are particularly susceptible to H. pylori infection (2), with approximately one-third of children worldwide being infected (3). Moreover, about two-thirds of adult patients acquired their H. pylori infection before the age of 10 (4, 5), underscoring the importance of controlling H. pylori infection during childhood. Currently, "triple therapy" is commonly used clinically to eradicate H. pylori infection (6). However, some patients may experience a recurrence of the infection after receiving treatment, which represents a significant challenge in the management of H. pylori infection (7). Recurrence rates are notably higher among younger patients.
2. Objectives
Given the context, our research team aims to understand the recurrence of H. pylori infection in children in the local region and the risk factors associated with its recurrence. We utilized a standardized survey questionnaire to gather data on personal history (e.g., prior infections, history of treatment, history of drug allergy, etc.), family history (e.g., family history of H. pylori infection, gastric and duodenal ulcers, gastrointestinal malignancies, etc.), health status, and family socioeconomic status (e.g., family economic income, education level and occupation of the parents, etc.). This was followed by a 1-year follow-up of children in the local region who had successfully undergone eradication therapy. The findings are reported below.
3. Methods
3.1. General Information
This study is a retrospective clinical investigation. The sample size was calculated based on the eradication rate of H. pylori in China, which ranges from 70% to 85%. The sample size formula used for counting data (rate) is n = z2 × p × (1 - p) / d2, employing a 95% confidence interval where z = 1.96, p = 77.5%, and the acceptable margin of error (d) = 0.05. The minimum sample size calculated was 268 individuals. Due to potential data incompleteness and other factors, the final sample comprised 328 participants.
The study subjects were 328 children aged 4 - 16 years, diagnosed with H. pylori infection and successfully treated in a hospital from January 2020 to June 2021. Among the enrolled children, there were 177 boys and 151 girls, with an average age of 8.9 ± 2.8 years. The children were assessed through a questionnaire survey covering personal history, family history, health status, and family socioeconomic status, followed by a 1-year follow-up. The study received approval from the Institutional Ethics Committee of the Hospital, and written informed consent was obtained from all participants.
Diagnostic criteria for H. pylori infection included children exhibiting positive results from any of the following tests: rapid urease test, endoscopic pathological staining, or the 13C-urea breath test, conducted due to digestive system symptoms or a strong demand for an H. pylori test (8).
3.2. Inclusion Criteria
(1) Children aged 4 - 16 years;
(2) Positive 13C-urea breath test, gastric mucosal rapid urease test, or tissue section staining, followed by a negative 13C-urea breath test after 4 weeks of eradication treatment;
(3) Children capable of completing a 1-year follow-up and returning to the hospital every 6 months for a repeat 13C-urea breath test.
3.3. Exclusion Criteria
(1) Children with major organ or mental diseases;
(2) Children with poor compliance who cannot complete follow-up on time;
(3) Children who had an acute infectious disease in the past month.
3.4. Research and Investigation Methods
Our unified survey questionnaire was based on the national H. pylori infection research questionnaire, adapted to reflect local economic levels and dietary habits. The questionnaire covered various topics, including sociodemographic characteristics (gender, age, parental education level, income status, etc.), dietary habits (shared meals, meal structure, etc.), lifestyle (living in rural or urban areas, cohabitation with parents, campus residency, etc.), and H. pylori-related diseases (treatment history, treatment plans, frequency, and presence of digestive tract diseases). All enrolled children were surveyed on personal history, family history, health status, and family socioeconomic status by medical staff with intermediate or higher professional titles and systematic training. The authenticity and reliability of the questionnaire were maintained during the survey, with care taken to avoid leading questions. Additionally, the 13C-urea breath test was re-administered at 6 and 12 months post-enrollment. Children testing positive on these subsequent tests were considered to have a recurrence of H. pylori infection. The study process flowchart is shown in Figure 1.
3.5. Statistical Analysis
Statistical analysis was conducted using SPSS 25.0 software. Enumerated data were expressed as n(%), and measurement data were presented as means (± standard deviation). The chi-square test was used for inter-group comparisons of categorical data, such as gender and recurrence rate, while the t-test was used for inter-group comparisons of continuous data, such as age. The results of the questionnaire survey were statistically analyzed using a binary logistic regression equation, with the recurrence rate as the dependent variable. A P-value of < 0.05 was considered statistically significant.
4. Results
Out of the 328 children enrolled with H. pylori infection, 295 (89.9%) were successfully followed up, while 33 cases were lost to follow-up, resulting in a loss rate of 10.1%. Among the children who were successfully followed up, 55 (18.6%) tested positive on the 13C-urea breath test and were considered as having a recurrence (the recurrence group), while 240 (81.4%) tested negative and were considered as not having a recurrence (non-recurrence group). The recurrence group comprised 31 boys and 24 girls, while the non-recurrence group included 132 boys and 108 girls, with average ages of 8.3 ± 2.1 years and 9.0 ± 2.8 years, respectively. No statistically significant differences were found in the comparison of gender and age between the two groups (P > 0.05), as presented in Table 1.
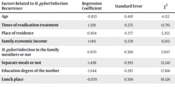
A questionnaire survey was conducted on the personal history, family history, health status, and family socioeconomic status of the enrolled children. Univariate chi-square analysis of the questionnaire results indicated that age (χ2 = 4.122, P = 0.042), number of eradication treatments (χ2 = 12.761, P < 0.001), the mother's education level (χ2 = 17.166, P < 0.001), place of residence (χ2 = 5.252, P = 0.022), family income (χ2 = 9.103, P = 0.003), and whether meals were separate (χ2 = 13.241, P < 0.001) were significant factors influencing H. pylori infection recurrence (Table 2).
| Factors Related to H. pylori Infection Recurrence | Regression Coefficient | Standard Error | χ2 | P-Value | OR | 95%CI |
|---|---|---|---|---|---|---|
| Age | -0.833 | 0.410 | 4.122 | 0.042 | 0.435 | 0.195 - 0.972 |
| Times of eradication treatment | 1.339 | 0.375 | 12.761 | < 0.001 | 3.816 | 1.830 - 7.956 |
| Place of residence | 0.864 | 0.377 | 5.252 | 0.022 | 2.372 | 1.133 - 4.967 |
| Family economic income | 1.140 | 0.378 | 9.103 | 0.003 | 3.128 | 1.491 - 6.562 |
| H. pylori infection in the family members or not | 0.670 | 0.386 | 3.007 | 0.083 | 1.953 | 0.916 - 4.163 |
| Separate meals or not | -1.436 | 0.395 | 13.241 | < 0.001 | 0.238 | 0.110 - 0.516 |
| Education degree of the mother | -1.644 | 0.397 | 17.166 | < 0.001 | 0.193 | 0.089 - 0.420 |
| Lunch place | -0.670 | 0.396 | 16.126 | 0.091 | 0.512 | 0.235 - 1.113 |
Further multivariate analysis included these significant factors from the univariate analysis in a logistic regression model. The results (Table 3) revealed that undergoing fewer than two eradication treatments, living in a city, and having a high family income were combined protective factors against H. pylori infection recurrence in children (OR < 1, P < 0.05). Conversely, being younger than 10 years old, not having separate meals, and having a mother with a lower education level were combined risk factors for H. pylori infection recurrence in children (OR > 1, P < 0.05).
| Factors Related to H. pylori Infection Recurrence | Regression Coefficient | Standard Error | χ2 | P-Value | OR | 95%CI |
|---|---|---|---|---|---|---|
| Age of < 10 years old | 0.888 | 0.405 | 4.810 | 0.028 | 2.431 | 1.099 - 5.377 |
| Times of eradication treatment, < 2 times | -1.304 | 0.367 | 12.590 | < 0.001 | 0.271 | 0.132 - 0.558 |
| Living in city | -0.817 | 0.366 | 4.995 | 0.025 | 0.442 | 0.216 - 0.904 |
| High economic income | -1.027 | 0.366 | 7.856 | 0.005 | 0.358 | 0.175 - 0.734 |
| Non-separate meals | 1.447 | 0.389 | 13.819 | < 0.001 | 4.252 | 1.982 - 9.121 |
| Lower education degree of the mother | 1.614 | 0.392 | 17.001 | < 0.001 | 5.025 | 2.333 - 10.823 |
5. Discussion
H. pylori infection is among the most common infections in humans, typically occurring during childhood. Although most infected individuals are asymptomatic, about 30% may develop mild to severe upper gastrointestinal diseases (9). With a growing understanding of H. pylori, considerable research has focused on its diagnosis and treatment. In recent decades, there has also been an increasing focus on studying the recurrence of H. pylori infection after eradication, especially in children, where relatively fewer studies have been conducted on the risk factors for recurrence after eradication. This study was performed to comprehensively discuss the risk factors of recurrence of H. pylori infection in children in the local region.
It is acknowledged that the recurrence rate of H. pylori infection is highest in the first year post-eradication and is significantly influenced by socioeconomic conditions (10). Recurrence rates may vary significantly between different countries or even within different regions of the same country. Our study found that the recurrence rate of H. pylori infection in children aged 4 - 16 in the region was 18.6% after one year of follow-up. Literature suggests that recurrence rates in developing countries are much higher than those in developed countries (11, 12). For example, the annual recurrence rate in Latin America is 11.2% (13), while it is 9.3% in Mexico (14). A study in South Korea reported a recurrence rate of 10.9% following eradication (15), and in Vietnam, the reinfection rate was 23.5% after 11 months of follow-up (16). Our study's recurrence rate falls within these reported ranges, indicating significant regional differences in the recurrence of H. pylori infection. The annual reinfection rate among 5,193 H. pylori-infected patients across 15 provinces in China after 6-84 months of follow-up is 1.5% (17), while the rate reported in Chongqing, China, is 4.75% (18). Our study has higher annual recurrence rates than those reported in China and Chongqing, which may be related to the underdeveloped local economy and the demographics of the children involved in this study. Age is another influencing factor for the recurrence of H. pylori infection, with a higher recurrence rate observed in children (19). Research indicates that the one-year recurrence rate of H. pylori infection in children under 10 years old is 20%, while it is 8% in children over 10 years old (20). Our research confirms that being under 10 years old is an independent risk factor for H. pylori infection recurrence, aligning with previous studies (21, 22).
The recurrence of H. pylori infection is a multifactorial process potentially related to personal medical history, family history, health status, and family socioeconomic status. Research has demonstrated that age and socioeconomic status are independently associated with the recurrence of H. pylori infection (23). Additionally, risk factors for the recurrence of H. pylori infection include low education levels, living in rural areas, family members not receiving simultaneous H. pylori eradication treatment, contact with H. pylori-infected patients, and low household income (15, 17, 24-26). Our research findings suggest that living in rural areas, having low economic income, not sharing meals, and having a low maternal education level are independent risk factors for the recurrence of H. pylori infection, consistent with previous reports. Particularly, families with low education levels, rural residence, and low incomes often lack sufficient health knowledge, pay less attention to children's illnesses, and maintain relatively poor hygiene standards. Most of these families share tableware during meals, which are major contributors to the recurrence of H. pylori infection (27, 28).
Given our findings, it can be concluded that younger children may exhibit a higher recurrence rate of H. pylori infection. For children under 10 years old with H. pylori infection, the high risk of recurrence should be considered before starting eradication treatment. Additionally, patients with multiple eradication attempts may face a higher likelihood of recurrence. Therefore, it is essential to adopt regular and systematic treatment strategies to minimize the need for repeated eradication and thus reduce the recurrence rate of H. pylori infection. Promoting good dietary and health habits, as well as reducing the frequency of dining out, can also decrease the recurrence rate of H. pylori infection. This underscores the importance of actively educating the public about H. pylori prevention and control, encouraging meal sharing, and enhancing awareness of H. pylori and health prevention to reduce the recurrence of H. pylori infection.
It should be noted that this study has limitations, including being a single-center study with a small sample size, potential recall bias in the questionnaire survey, and the lack of strain culture and identification. Further research with a larger sample size is planned in an expanded study area to determine whether the recurrence of H. pylori infection is due to the recurrence of the original strain or reinfection by a new strain.
5.1. Conclusions
From January 2020 to June 2021, the recurrence rate of H. pylori infection in children aged 4 - 16 in the Baoding area was relatively high. The combined effect of multiple factors can lead to the recurrence of H. pylori infection in children. The protective factors against the recurrence of Hp infection in children include fewer than two eradication treatments, living in cities, and higher family income. Being younger than 10 years old, not sharing meals, and low maternal education level are independent risk factors for the recurrence of H. pylori infection in children.