1. Background
According to the World Health Organization (WHO) definition, pre-term labor is characterized by pregnancy termination before reaching 37 weeks of gestational age, resulting in live birth (1). Approximately 15 million pre-term infants are born worldwide each year, and there is a global trend of increasing pre-term labor incidence. Complications arising from pre-term labor stand as the leading causes of mortality among children under the age of 5, accounting for nearly 1 million deaths in 2015 (1).
The mechanisms underlying the initiation of labor at term are complex and not fully understood. The sequence and timing of events leading to pre-term initiation of labor, whether through induction of contractions or premature rupture of membranes (PROM), are unknown to us (2). Pre-term labor is primarily attributed to spontaneous pre-term labor (40% - 50%) and PROM (20% - 30%), with maternal and fetal factors complicating pregnancy and necessitating medical induction of labor accounting for the remaining 20% - 30% of pre-term labor cases (3).
In developed countries, pre-term labor is the primary cause of both morbidity and mortality in infants (3). It has been associated with a range of health issues from infancy to adulthood. With advancements in the management of pre-term newborns, we now encounter a population with varying comorbidities directly linked to the degree of prematurity (4).
Complications stemming from pre-term labor include a wide array of issues, including respiratory distress, apnea, hypothermia, feeding difficulties, hypoglycemia, hyperbilirubinemia, jaundice, sepsis, and even death (5). At present, pre-term complications stand as the leading causes of early-life mortality, constituting 35% of infant mortality and 18% of under-5 mortality worldwide (6). Furthermore, pre-term labor imposes substantial economic burdens on families and societies, including both the costs associated with initial newborn care and those stemming from subsequent complications that arise during childhood. Additionally, families are faced with the challenge of handling non-medical costs that arise as a result of changes in their daily lives (7).
It is challenging to estimate the exact prevalence of pre-term labor, primarily due to incomplete reporting of data, particularly in low-income countries (6). In a study involving 184 countries, pre-term labor accounted for 5% - 18% of live birth cases (1). The estimated prevalence of pre-term labor in Iran in 2017 was 10% (8).
An increasing trend in the incidence of pre-term labor has been observed globally (9). A study examining the trend of pre-term labor reported an increase in the rate of pre-term labor from 9.8 in the year 2000 to 10.6 in 2014 (10). The incidence of pre-term labor is influenced by various factors, including the social environment, economic conditions, and race, leading to variations in incidence rates between countries (11). To the best of our knowledge, no prior studies have explored the trend of pre-term labor in Iran. Moreover, due to racial and environmental differences, the findings from studies on the trend of pre-term labor may not be applicable to the Iranian population.
2. Objectives
The objective of this study was to examine the trend of pre-term labor and its contributing factors in Arak city, Iran, from 2005 to 2019.
3. Methods
This study used a retrospective-descriptive design based on routinely recorded data from pregnant women who sought care at Taleghani Hospital, the referral obstetrics and gynecology hospital affiliated with Arak University of Medical Sciences. Data collected from pregnant women over a 15-year period (2005 - 2019) were reviewed, and a researcher-developed checklist was used for data recording.
The inclusion criterion was all women who gave birth at Taleghani Hospital, Arak, Iran. The exclusion criterion was incomplete or insufficient data for calculating gestational age.
Out of a total of 89 415 recorded live birth cases, 108 were excluded due to inadequate data for gestational age calculation, resulting in 89 307 cases eligible for the study.
The collected data included the following variables: Date of delivery, infant gender, birth weight, type of delivery, number of infants in cases of multiple pregnancies, maternal age, maternal history of hypertension and diabetes, history of intrauterine fetal death, anencephaly, and fetal anomaly, polyhydramnios, oligohydramnios, PROM, placenta previa, placental abruption, cervical ripening, maternal history of smoking, and maternal history of urinary tract infection (UTI). The study specifically focused on data related to live births occurring before 37 weeks of gestation.
Gestational age was determined using 2 methods: (1) reported gestational age obtained through ultrasound scans during the first trimester (before the sixth day of the 13th gestational week); and (2) the date of the last normal menstrual period (LNMP) in cases where first-trimester ultrasound results were unavailable.
This study was approved by the Ethics Committee of Arak University of Medical Sciences (code: IR.ARAKMU.REC.1394.170), and all data related to the study participants were anonymized to protect their privacy.
3.1. Statistical Analysis
Continuous variables were summarized using mean and SD, while nominal variables were presented as percentages. The trend of pre-term labor over the study period was assessed using the linear-by-linear test. The impact of various study parameters on pre-term labor was examined through both univariate and multivariate logistic regression analyses. Data analysis was performed using SPSS version 25.
4. Results
Demographic characteristics of the study population are presented in Table 1. Among the 89 307 cases of live births, 80 037 (89.6%) were term, 9210 (10.3%) were pre-term, and 60 (0.1%) were post-term deliveries. Significant differences were observed in sex (P = 0.002), neonatal weight (P < 0.001), maternal age (P = 0.001), maternal diabetes (P < 0.001), type of delivery (P < 0.001), maternal blood pressure (P < 0.001), and gravida (P = 0.020) categories between term, pre-term, and post-term deliveries.
| Variables | Total | Term | Pre-term | Post-term | P |
|---|---|---|---|---|---|
| Sex | 0.002 b, d | ||||
| Male | 46175 (51.7) | 41222 (89.3) | 4920 (10.7) | 33 (0.1) | |
| Female | 43132 (48.3) | 38815 (90.0) | 4290 (9.9) | 27 (0.1) | |
| Neonatal weight | < 0.001 b, d | ||||
| ELBW | 2429 (2.7) | 1191 (49.0) | 1238 (51.0) | 0 (0.0) | |
| VLBW | 2719 (3.0) | 1814 (66.7) | 905 (33.3) | 0 (0.0) | |
| LBW | 10488 (11.7) | 6064 (57.8) | 4424 (42.2) | 0 (0.0) | |
| Normal | 68460 (76.7) | 65808 (96.1) | 2640 (3.9) | 12 (0.0) | |
| Macrosomia | 5211 (5.8) | 5160 (99.0) | 3 (0.1) | 48 (0.9) | |
| Maternal age (y) | 0.001 b, d | ||||
| < 18 | 1508 (2.1) | 1311 (86.9) | 197 (13.1) | 0 (0.0) | |
| 18 - 25 | 28368 (38.9) | 24963 (88.0) | 3384 (11.9) | 21 (0.1) | |
| 26 - 30 | 19880 (22.3) | 17313 (87.1) | 2551 (12.8) | 16 (0.1) | |
| 31 - 35 | 15645 (17.5) | 13603 (86.9) | 2028 (13.0) | 14 (0.1) | |
| 36 - 40 | 6241 (7.0) | 5358 (85.9) | 875 (14.0) | 8 (0.1) | |
| > 40 | 1347 (1.5) | 1171 (86.9) | 175 (13.0) | 1 (0.1) | |
| Maternal diabetes | 1582 (6.0%) | 1267 (80.1) | 312 (19.7) | 3 (0.2) | < 0.001 b, d |
| Delivery type | < 0.001 b, d | ||||
| NVD | 54568 (61.1) | 49449 (90.6) | 5085 (9.3) | 34 (0.1) | |
| C/S | 34739 (38.9) | 30588 (88.1) | 4125 (11.9) | 26 (0.1) | |
| Maternal blood pressure | < 0.001 b, d | ||||
| Normal | 24311 (92.3) | 15932 (65.5) | 8355 (34.4) | 24 (0.1) | |
| Hypertension | 865 (3.3) | 521 (60.2) | 343 (39.7) | 1 (0.1) | |
| Mild preeclampsia | 20 (0.5) | 63 (52.5) | 57 (47.5) | 0 (0.0) | |
| Severe preeclampsia | 1007 (3.8) | 558 (55.4) | 444 (44.1) | 5 (0.5) | |
| Eclampsia | 32 (0.1) | 21 (65.6) | 11 (34.4) | 0 (0.0) | |
| Gestational age (weeks) | 38.59 ± 2.40 | 39.00 (38.00 - 40.00) | 35.00 (31.00 - 36.00) | 43.00 (43.00 - 43.00) | < 0.00 c, d |
| Number of previous abortions | 0.20 ± 0.54 | 0.00 (0.00 - 0.00) | 0.00 (0.00 - 0.00) | 0.00 (0.00 - 0.00) | 0.142 c |
| Gravida | 2.00 (1.00 - 3.00) | 1.00 (1.00 - 2.00) | 2.00 (1.00 - 3.00) | 2.00 (1.00 - 3.00) | 0.020 c, d |
| Parity | 0.00 (0.00 - 1.00) | 0.00 (0.00 - 1.00) | 0.00 (0.00 - 1.00) | 1.00 (0.00 - 1.00) | 0.085 c |
Demographic Characteristics and Their Comparison Between Term, Pre-term, and Post-term Cases a
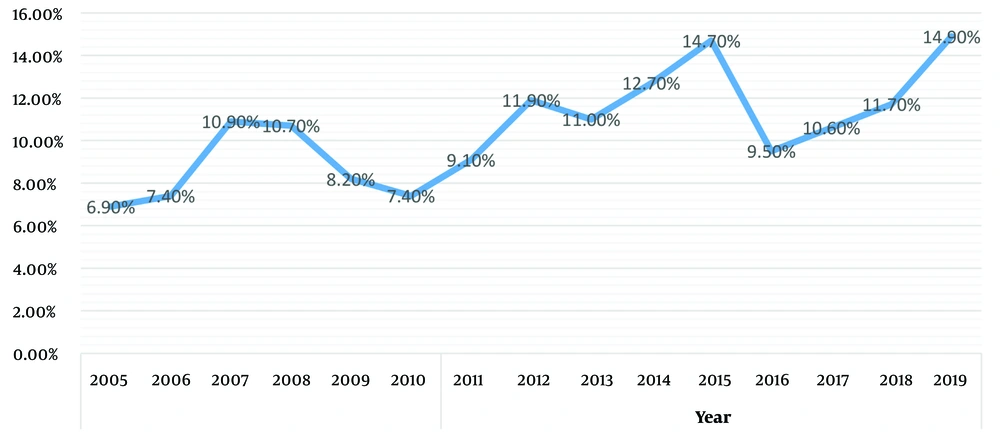
The overall percentage of pre-term labor was 6.9% in 2005, increasing to 14.9% in 2019 (Figure 1). The number of recorded live births and the percentage of pre-term labor in 2005, 2010, 2015, and 2019 were 5675 (6.9%), 7005 (7.4%), 6408 (14.7%), 3051 (14.9%), respectively (Table 2). The trend of pre-term labor over the study period showed a significant increase (P < 0.001).
| Year | P | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | ||
| Pre-term | 392 (6.9) | 429 (7.4) | 694 (10.9) | 712 (10.7) | 546 (8.2) | 517 (7.4) | 633 (9.1) | 770 (11.9) | 650 (11.0) | 789 (12.7) | 939 (14.7) | 599 (9.5) | 555 (10.6) | 531 (11.7) | 454 (14.9) | < 0.001 b |
| Term | 5282 (93.1) | 5377 (92.6) | 5689 (89.1) | 5939 (89.2) | 6095 (91.7) | 6481 (92.5) | 6323 (90.9) | 5718 (88.1) | 5258 (89.0) | 5428 (87.1) | 5468 (85.3) | 5704 (90.5) | 4674 (89.4) | 4004 (88.0) | 2597 (85.1) | |
| Post-term | 1 (0.0) | 3 (0.1) | 2 (0.0) | 7 (0.1) | 4 (0.1) | 7 (0.1) | 3 (0.0) | 0 (0.0) | 0 (0.0) | 17 (0.3) | 1 (0.0) | 0 (0.0) | 0 (0.0) | 15 (0.3) | 0 (0.0) | |
Frequency and Percentage of Pre-term, Term, and Post-term Deliveries Recorded During the Study Period a
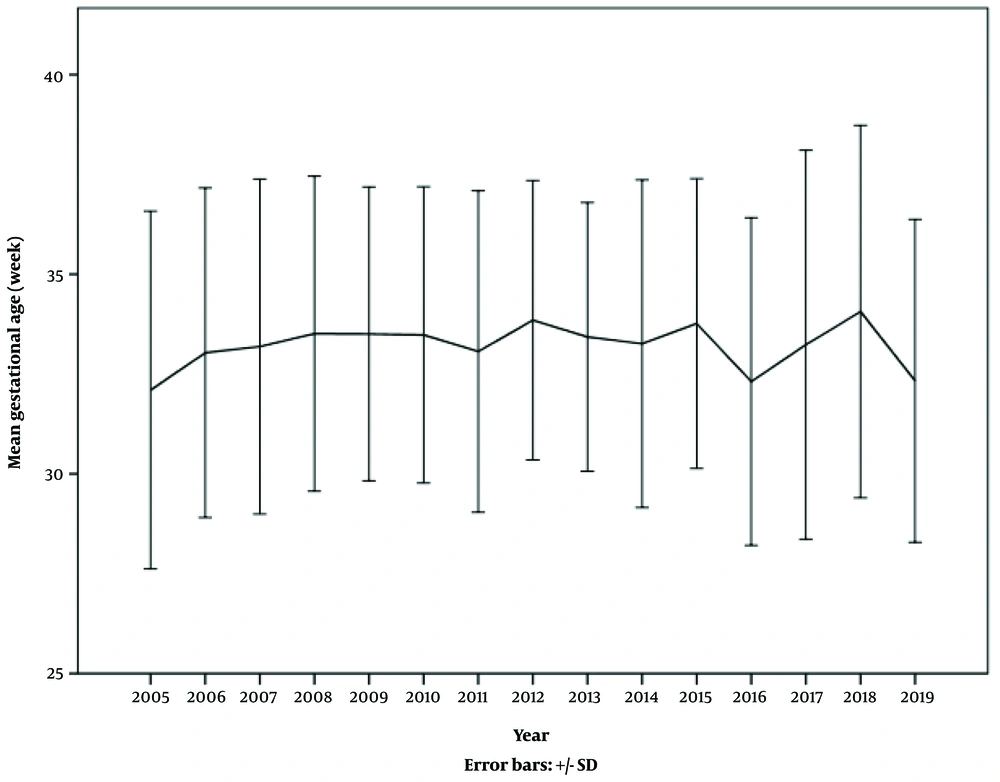
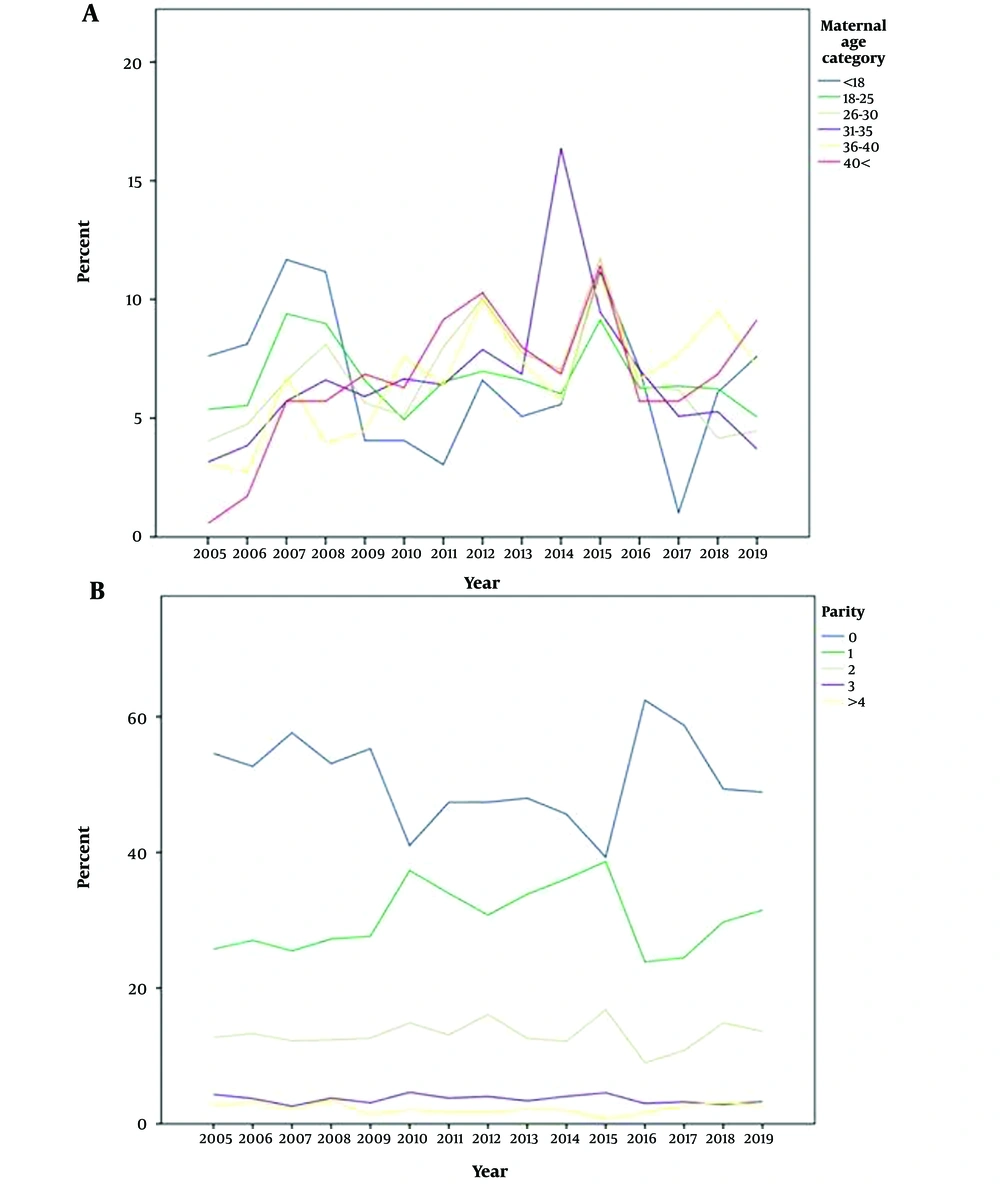
The overall trend in gestational age at birth among pre-term labor cases is presented in Figure 2. There was no significant trend change in gestational age at birth during the study period (P = 0.314). Trends in pre-term labor as per maternal age and parity are presented in Figure 3. Significant differences in trends of pre-term labor were observed among maternal age and parity categories (P < 0.001 for each), indicating a significant increase in the percentage of maternal age below 18 years old in 2014 and a significant decrease in the percentage of primiparity between 2010 and 2015 compared to the rest of the study duration.
Univariate logistic regression showed that time points (P < 0.001), sex (P = 0.001), maternal age (P = 0.334), maternal diabetes (P < 0.001), maternal hypertension (P < 0.001), birth weight (P < 0.001), and type of delivery (P < 0.001) increased the risk of pre-term labor. Therefore, these variables were included in the multivariate logistic regression model (Table 3).
| Variables | P | OR | 95% CI for OR | |
|---|---|---|---|---|
| Lower | Upper | |||
| Time period | ||||
| 2005 - 2009 | < 0.001 a | Reference | ||
| 2010 - 2015 | 0.150 | 0.744 | 0.498 | 1.113 |
| 2015 - 2019 | < 0.001 a | 0.002 | 0.002 | 0.003 |
| Sex (male) | 0.523 | 1.033 | 0.935 | 1.141 |
| Maternal age category (y) | ||||
| < 18 | 0.120 | Reference | ||
| 18 - 25 | 0.062 | 0.703 | 0.486 | 1.018 |
| 26 - 30 | 0.156 | 0.763 | 0.526 | 1.108 |
| 31 - 35 | 0.328 | 0.828 | 0.568 | 1.208 |
| 36 - 40 | 0.282 | 0.808 | 0.548 | 1.191 |
| 40 < | 0.197 | 0.722 | 0.440 | 1.184 |
| Maternal diabetes | 0.447 | 1.081 | 0.885 | 1.321 |
| Birth weight category | ||||
| Normal | < 0.001 a | Reference | ||
| Low birth weight | < 0.001 a | 0.023 | 0.021 | 0.026 |
| Macrosomia | 0.142 | 0.726 | 0.512 | 1.202 |
| Type of delivery (Cesarean section) | 0.836 | 0.989 | 0.893 | 1.096 |
| Gestational blood pressure categories | ||||
| No | 0.006 a | Reference | ||
| Gestational hypertension | 0.837 | 1.031 | 0.774 | 1.373 |
| Mild preeclampsia | 0.008 a | 2.538 | 1.277 | 5.045 |
| Severe preeclampsia | 0.005 a | 1.422 | 1.109 | 1.823 |
| Eclampsia | 0.769 | 1.248 | 0.285 | 5.463 |
The Influencing Factors on Pre-term Labor Based on Multivariate Regression Analysis
Multivariate logistic regression showed that the risk of pre-term labor increased by 15% from the first time period (2005 - 2009) to the second 5-year period (2010 - 2014), which was not significant (P = 0.744). The risk of pre-term labor increased by 0.001% from the first time period to the third time period (2015 - 2019), which was statistically significant (P = 0.002; Table 2).
Our results also showed that mild and severe preeclampsia were among the influencing factors of pre-term labor. The risk of pre-term labor increased by 2.5-fold and 1.5-fold in pregnancies with mild (P = 0.008) and severe preeclampsia (P = 0.005), respectively. Furthermore, pre-term labor increased by 0.023% in low birth weight compared to normal birth weight pregnancies (P < 0.001). Overall, the most influencing factors on pre-term labor were mild preeclampsia (odds ratio [OR] = 2.538) followed by severe preeclampsia (OR = 1.422; Table 2).
5. Discussion
Addressing changes in the rate of pre-term labor over the past decade has posed a significant challenge. The current study showed an increasing trend in the rate of pre-term labor. Specifically, the percentage of pre-term labor (defined as pregnancy termination before 37 gestational weeks leading to live birth) increased from 8.9% in the first 5-year period to 12.1% in the third 5-year period. The rate of pre-term labor exhibited a 1.4% increase from the first to the second 5-year period, which was not statistically significant, and a significant 1.8% increase from the second to the third time period. This secular trend in the rate of pre-term labor over the 15-year period persisted as statistically significant even after adjusting for confounding variables, including gender, maternal age, maternal diabetes, maternal hypertension, birth weight, and type of delivery.
Notably, this trend is consistent with the findings of Rezaeean et al.; they compared pre-term labor rates across studies and reported a nearly 2-fold increase from 1996 to 2000 (from 6.7% to 12.1%), reaching 16.4% in 2003 (12). Similar increasing trends have been observed in neighboring countries of Iran. For example, Medani documented an increasing trend in pre-term labor from 2007 to 2016 in Saudi Arabia (13). Likewise, Taha et al. reported a slight but notable increasing trend in the rate of pre-term labor in the United Arab Emirates (14).
Our study findings are consistent with research conducted in other countries, showing an alarming increase in the incidence of pre-term labor. This is consistent with the study by Jing et al., reporting a steady 1.7% increase in pre-term labor incidence from 1990 to 2016 (15). Similarly, a study in South Australia revealed a 40% increase in pre-term labor rates in singleton pregnancies from 1986 to 2014 (16), while Chen et al. in Taiwan observed an 11.1% increase from 2001 to 2011 (17).
However, it is worth noting that some studies have reported contrasting findings. For instance, Richter et al. evaluated 188 044 singleton pregnancies in Canada from 2009 to 2019 and found a stable pre-term labor rate of 6.2% (18). Another study in Bangladesh in 2019 showed a decrease in the pre-term labor rate from 29% during 1990 - 1994 to 11% during 2010 - 2015 (19). Similarly, Ravelli et al. in the Netherlands showed a decrease in the pre-term labor rate from 6.1% in 2010 to 5.6% in 2015 (20). In the United States, a study on 41 206 315 pregnancies in 2018 reported a decline in the pre-term labor rate from 12.3% in 2003 to 11.5% in 2012 (21).
These varying trends in pre-term labor can be attributed to a range of social, environmental, economic, and racial factors that differ between countries (11). Changes in the rates of unintended pregnancies and medical abortions during specific time periods have also been suggested as contributing factors to observed shifts in pre-term labor rates.
In the context of our study in Arak, Iran, several unique factors may have influenced the trends in pre-term labor. Arak, being one of Iran's major industrial hubs, experienced a rising trend in air pollution. To address this issue, a comprehensive plan to reduce air pollution was initiated in 2007 (22). While the plan was effective, the changes in air pollution indices were mostly observed after 2016, leading to increased hospital admissions in the city (23). The decrease in the rate of pre-term labor observed in 2016 and 2017 may be partially attributed to improved air quality during this period.
However, it is essential to interpret reported data on pre-term labor rates cautiously. Advances in health care systems may have resulted in only high-risk pregnancies being referred to tertiary hospitals, potentially inflating the reported pre-term labor rate. This might explain the observed high incidence of pre-term labor.
Our study identified mild and severe preeclampsia as the primary risk factors for pre-term labor in the study population. Preeclampsia is a known risk factor associated with an increased likelihood of pre-term labor (24). Our findings are consistent with those of Guida et al. (25) and Bossung et al. (26), both showing a significant increase in pre-term labor in pregnancies with mild and severe preeclampsia (25, 26). The proposed mechanisms underlying pre-term labor in preeclampsia include reduced placental perfusion due to incomplete regeneration of spiral arteries in the early stages of pregnancy, systemic inflammation, and chorioamnionitis (27).
Furthermore, our study found that the rate of pre-term labor was higher in low-birth-weight deliveries compared to normal-weight deliveries. It is important to note that term babies can also have low birth weight due to intrauterine growth retardation (IUGR) or being small for gestational age (SGA). This might be the reason for the reported 67% overlap between pre-term labor and low birth weight (28).
Regarding gender differences, our findings did not show statistically significant differences in terms of pre-term labor. However, there was a slightly higher proportion of male gender among pre-term cases compared to term cases. Previous studies have shown conflicting results regarding the relationship between gender and pre-term labor. While some studies found no significant relationship between gender and pre-term labor (29, 30), Teoh et al. reported that male gender was a risk factor for both spontaneous pre-term labor and pre-term labor due to PROM in European women (31). These differences in findings could be attributed to differences in sample sizes across studies, as well as differences in the prevalence of underlying conditions that increase the risk of pre-term labor, some of which may be gender-dependent.
The current study showed that maternal age was not significantly associated with pre-term labor. Previous studies have shown inconsistent results regarding the relationship between maternal age and the risk of pre-term labor. Some studies have reported no significant relationship between maternal age and pre-term labor (32, 33), while others indicated a significant relationship between pre-term labor and older maternal age (34, 35).
The current study showed that the rate of pre-term labor was 1.08 times higher in mothers with diabetes compared to healthy mothers, although this finding was not statistically significant. This is consistent with the findings of Kong et al., showing a significant relationship between type 1 or type 2 diabetes and pre-term labor, while no significant relationship was found between gestational diabetes and pre-term labor (36). It is worth noting that the non-significant higher rate of pre-term labor in mothers with gestational diabetes in our study may be due to the lack of differentiation between gestational diabetes and diabetes in the medical records of the mothers. Finally, our study found no significant relationship between the type of delivery and pre-term labor.
The current study had several limitations. While our data source from a large referral hospital provided a substantial sample size of over 89 000 live births over 15 years, it is important to acknowledge that single-hospital data may not be readily generalizable to the general population. Additionally, like many retrospective studies, the presence of missing or incorrect data could lead to the exclusion of some cases. Furthermore, less obvious errors, such as incorrect recording of maternal age or maternal medical history and unreliable information, could potentially reduce the reliability of the recorded data. There is also the possibility that other confounding variables not considered in our study may exist due to unavailable data.
Another limitation to consider is the potential impact of in-hospital factors on pre-term labor, including differences in the management approach for pregnancies with chronic diseases in terms of indications for terminating pregnancy and variations in control and follow-up processes for high-risk pregnancies. Given that our hospital was a tertiary hospital, there was a high tendency for the admission of high-risk pregnancies, which could affect the study's outcomes. Unfortunately, medical records lacked data on the use of labor induction methods, specifically the presence or absence of cervical ripening. Although cervical ripening did not appear to be related to the outcomes in our study, this issue should still be noted as a potential limitation.
On a positive note, the study possessed several strengths. For the first time in Iran, our study evaluated the trend of pre-term labor and its influencing factors, providing valuable insights into this important issue. Being a population-based study, our findings could be generalized to the entire population. Additionally, identical forms were consistently used for recording data across the 15-year study period, ensuring data comparability and enhancing the quality of our findings.
Further studies are needed to explore trends in pre-term labor in different regions of Iran. These efforts can help inform health authorities and guide interventions aimed at reducing the risk of pre-term birth in Iran by addressing factors associated with pre-term labor.
5.1. Conclusions
The findings of the current study showed a clear secular trend in the rate of pre-term labor. Additionally, preeclampsia is a notable risk factor for pre-term labor. It is important to emphasize that pre-term labor is a significant contributor to under-5 mortality, responsible for 1 million deaths and representing the leading cause of under-5 mortality (18%) and neonatal mortality (35%). Given these substantial implications, it is crucial to prioritize pre-term labor as a key area of concern in achieving the third goal of the United Nations Sustainable Development, which aims to end preventable newborn and under-5 deaths by 2030 (6).
Recognizing the increasing trend of pre-term labor serves as a vital alarm for health care policymakers. This highlights the urgent need to develop a comprehensive program focused on the early diagnosis of high-risk pregnancies and the prevention of pre-term labor. For instance, it is necessary to identify the root causes of spontaneous pre-term labor, allowing for tailored management approaches. Concerning induced pre-term labor, thorough assessments should be conducted to understand maternal health conditions and evaluate policies and midwifery care practices.
Prenatal care plays a pivotal role in the prevention of pre-term labor. These crucial visits allow for the assessment of the pregnant mother's health and the condition of the fetus. Moreover, they offer an opportunity to provide recommendations for lifestyle modifications, particularly for high-risk behaviors that might lead to pre-term labor.