1. Background
Spontaneous pneumomediastinum (SPM) refers to the presence of free air in the mediastinum that occurs without an identifiable cause, such as trauma or surgical intervention. It was initially described by Louis Hamman in 1939. By 1944, Macklin had identified the mechanism behind the formation of pneumomediastinum through experiments with cats. He found that the release of free air from tears was due to a sudden increase in alveolar pressure, which then moved through the perivascular sheaths into the mediastinum (1). The diffusion of free air from the visceral pleura could account for the frequently associated pneumothorax. Yet, the underlying cause of alveolar wall fragility remains unclear. Despite its spontaneous nature, it is often observed that patients experience a precipitating action that activates the Valsalva maneuver, typically preceding chest pain. Such actions may include coughing (often linked to asthma or a history of smoking), (2) childbirth, (3) severe vomiting, (4) engaging in vigorous sports, diving, and heavy lifting, which might be noted in the patient's history (5). However, cases of SPM can also arise without any apparent triggering event or predisposing factor (6).
Spontaneous pneumomediastinum typically resolves spontaneously, sometimes with signs and symptoms healing unnoticed if small leaks are missed on X-rays. Conversely, the detection of larger leaks and mediastinal air prompts the need for differential diagnosis due to similar symptoms with esophageal perforation. Boerhaave syndrome, characterized by spontaneous esophageal perforation usually stemming from severe vomiting, presents with chest or abdominal pain. A longitudinal transmural tear occurs distally due to a sudden esophageal pressure increase. Late diagnosis, especially, can lead to severe complications like mediastinitis, (7) posing fatal risks. Hence, identifying mediastinal air in a young patient with the classic triad of chest pain, dyspnea, and subcutaneous emphysema in the emergency department initiates a challenging and resource-intensive process involving transfer to a specialized center, differential diagnosis, and prolonged hospitalization.
Boerhaave syndrome is typically observed in men aged 50 - 70 years, often with a history of alcohol consumption and severe postprandial vomiting. Common symptoms include vomiting and epigastric pain, with patients often exhibiting a toxic appearance and experiencing clinical and radiological deterioration, particularly the development of pleural effusion, within 24 hours. In contrast, SPM primarily affects young and healthy individuals, with vomiting being rare and epigastric pain uncommon. Symptoms of SPM tend to resolve, and radiological findings improve during follow-up.
2. Objectives
Our study aimed to explore the clinical presentation of SPM in pediatric patients, where the actual incidence may be underestimated due to nonspecific symptoms and easily overlooked radiological findings. Additionally, we discussed the diagnostic examinations necessary to rule out esophageal perforation and the consequent extended hospital stays.
3. Methods
Twenty-four pediatric patients diagnosed with SPM between 2014 and 2022 were included in our study. Ethical approval was obtained from the hospital ethics committee, and data were collected from the hospital institutional database and national information databases of the Ministry of Health using diagnosis codes for emphysema, pneumomediastinum, and pneumothorax. Patients with a follow-up period of less than 18 months and those with secondary pneumomediastinum were excluded. Demographic characteristics, clinical features, diagnostic procedures, treatment modalities, and follow-up outcomes were retrospectively analyzed. Data were presented using averages and percentages.
4. Results
During the study period, 24 patients were followed up with a diagnosis of SPM. The mean age of these patients was 14 years, with 20 males and 4 females included. The youngest patient was four years old, while the oldest was 18 years old.
Among the patients, 30% were smokers. Chest pain was reported by all patients, while 50% experienced dyspnea, 30% had neck pain, and 12% had symptoms of dysphagia. On average, patients sought medical attention one day after the onset of symptoms. The duration of symptoms varied, with some patients presenting within an hour of symptom onset while others waited up to two days before seeking medical care. Notably, all symptoms, including chest pain, resolved by the second day of hospitalization. In addition, the complaints regressed almost totally after the transfer from the emergency department to the service in 55% of the patients and completely resolved in 2 patients.
Various triggering factors were identified, including coughing in 11 patients (45%), severe sneezing in 1 patient, increased physical exertion (such as sports, weight lifting, or diving) in 8 patients (33%), and retching or vomiting in 2 patients (8%). Additionally, six patients (25%) were diagnosed with asthma. Two patients primarily admitted due to vomiting were found to have consumed drugs.
Subcutaneous emphysema was palpable in 16 patients (66%) upon physical examination. Half of the patients (50%) exhibited asthenia. Leukocytosis was observed in 9 patients (37.5%), while C-reactive protein (CRP) elevation was noted in the same number of patients. Cardiac markers were assessed in 14 patients in the emergency department, with two patients admitted after intense sports activities showing minimal elevation. Additionally, four patients (17%) had pneumothorax (PX), with one experiencing bilateral involvement and associated tachycardia and tachypnea.
Most patients had normal vital signs, as detailed in Table 1. Seven patients (29.1%) showed no abnormal findings on posteroanterior chest X-rays. Prior to transfer to our hospital, all patients underwent computed tomography (CT) scans, with one CT performed using oral and IV contrast and the remainder with only IV contrast.
| Parameter | Values a |
|---|---|
| Gender | |
| Male | 20 |
| Female | 4 |
| Age, y | 14 (4 - 18) |
| Additional disease/condition | |
| Asthma | 6 (25) |
| Drug intoxication | 2 (8) |
| Pneumothorax | 4 (16) |
| Single | 3 (12) |
| Bilateral | 1 (4) |
| Smoking | 7 (30) |
| Complaints | |
| Chest pain | 24 (100) |
| Dyspnea | 12 (50) |
| Neck pain | 7 (30) |
| Dysphagia | 3 (12) |
| Triggers | |
| Cough | 11 (45) |
| Vomiting | 2 (8) |
| Ball sports | 1 (4) |
| Weight lifting | 1 (4) |
| Diving | 1 (4) |
| Screaming | 1 (4) |
| Blowing up a balloon | 1 (4) |
| Sneezing | 1 (4) |
| Physical examination/laboratory findings | |
| Subcutaneous emphysema | 16 (66) |
| Asthenia | 12 (50) |
| Tachycardia | 1 (4) |
| Leukocytosis | 9 (37.5) |
| C-reactive protein (+) | 9 (37.5) |
| Cardiac Marker (+) | 2 (8) |
a Values are expressed as No. (%).
All patients in our series were transferred to our hospital from another health center. The reasons for requesting transfer to an upper center are provided in Table 2. A fluoroscopic esophagogram was conducted within 22 hours of the patient's admission to the pediatric surgery clinical stay for all patients except those who had undergone oral contrast-enhanced CT scans. The results of all esophagograms were normal. Endoscopy and bronchoscopy were not performed on any of the patients.
| First Diagnosis/the Reason for Transfer to Upper Center | Number of Patients |
|---|---|
| Pneumothorax/tube thoracostomy | 10 |
| Cardiac tamponade due to spontaneous pneumomediastinum/aspirating air with a needle | 2 |
| Spontaneous pneumomediastinum/tube thoracostomy | 6 |
During their stay in our ward, all patients received intermittent mask oxygen inhalation at a rate of 2 - 4 liters per minute under broad-spectrum mediastinitis prophylaxis, and oral intake was prohibited. Oral feeding commenced after a fluoroscopic esophagogram, and antibiotic prophylaxis was discontinued. The average fasting duration was 28 hours. The mean duration of symptom-free and untreated clinical hospital stay was 32 hours. None of the patients experienced worsening symptoms during follow-up. Patients were discharged once linear air images on direct radiographs disappeared or significantly decreased. The average hospital stay was 4.4 days. Key milestones during patient follow-up are summarized in Table 3.
| Event | Time, h |
|---|---|
| The onset of complaints-first hospital a | 6 |
| First hospital-our hospital's emergency department a | 10 |
| Emergency department- pediatric surgery clinic a | 1 |
| First admission to our hospital-fluoroscopic esophagogram a | 22 |
| Fasting duration | 28 |
| Symptom-free and untreated b -hospital stay duration | 32 |
| Linear air images disappeared or decreased evidently on the direct radiographs c | 106 |
a Time between two states.
b Without oxygen and medication.
c The time between the first diagnosis and the x-ray for the discharge decision.
All patients attended the outpatient clinic at least twice after discharge. Recommendations provided included restrictions on activities such as long flights, scuba diving, and high jumping, as well as staying within proximity to healthcare centers. Chest disease consultation was arranged for all patients. No further examinations or recommendations were deemed necessary as no parenchymal pathologies were observed on CT scans. Notably, no cases of recurrent SPM were identified during the follow-up period, which ranged from one to nine years in our series.
5. Discussion
Spontaneous pneumomediastinum primarily affects young, generally slender, and healthy individuals, with men comprising 72% of cases and a mean age of 23 years (8-10). In our pediatric SPM series, the mean age was 14 years, aligning with the literature, and there was a consistent male predominance (83%). Although the incidence of SPM in children is relatively low (0.003 - 0.0095%) (11, 12), some studies suggest it might be higher due to mild findings being missed on routine chest radiographs (13). Most of the studies mentioned that there may be a triggering or predisposing factor that leads to a sudden change in intrathoracic pressure, such as coughing (27.7%), physical exertion (21.1%), and recumbency/vomiting (13%) (8). In our series, the rates of these triggers were 45%, 33%, and 8%, respectively.
Despite the young age of the children in our series, the prevalence of smoking (30%) was noteworthy, along with asthma rates (25%) (8), which are in line with the literature findings. The overall condition and vital signs of SPM patients are typically stable (2), as observed in our series, where vital signs remained stable for all patients except one who had bilateral pneumothorax and was monitored in the intensive care unit for 24 hours (14). Symptoms of SPM are correlated with the volume of air leaked into the mediastinum. Common symptoms include chest pain (100%), dyspnea (50%), sore throat (30%), and dysphagia (12%), consistent with literature findings.
During the transfer from the emergency room to the pediatric surgery service, patients reported symptoms starting at least 2 hours and up to two days prior. Notably, chest pain improved or resolved significantly in 55% of patients, with subcutaneous emphysema being the most frequent examination finding (66%). Additionally, half of the cases involved asthenic children. Vital signs and laboratory findings of SPM patients are not extensively documented in the literature.
Leukocytosis was observed in 9 (37.5%) patients, and elevated CRP levels were found in 9 patients. Blood gas values were assessed for all patients upon arrival at the emergency department. Only the patient with bilateral pneumothorax exhibited low blood oxygen saturation. The peripheral oxygen saturation of all other patients breathing room air was above 97%, with no pathological features identified in their blood gas analyses. Cardiac markers were evaluated in 14 patients with a provisional diagnosis of myocardial infarction in the emergency department. Elevated markers were detected in two patients who presented with chest pain after intense physical activity, prompting a cardiology consultation. The diagnosis of SPM was confirmed based on mediastinal air observed in the echocardiograms of these two patients. Notably, no other cases diagnosed as SPM via echocardiograms were found in the literature.
During auscultation examinations, no special crackling sound known as Hamman's sign, produced by the friction of mediastinal air against the pleura, was noted. All patients in our series were transferred from other healthcare centers. The decisions leading to requests for transfer to tertiary centers are outlined in Table 2. All patients underwent CT scans, and the images were evaluated by emergency physicians. However, SPM diagnosis was missed in some cases, indicating a lack of proper recognition and treatment guidance in patients where the condition was identified.
Upon suspicion of SPM following a medical history and physical examination, a routine anterior-posterior chest radiograph is typically sufficient for diagnosis confirmation. Diagnosis is confirmed by the presence of linear air along the fascial planes between the mediastinum and muscles. Yellin et al. suggested that lateral X-rays would provide 100% confirmation since 30% of anterior-posterior X-rays may show normal findings or findings that could be overlooked without careful examination (15, 16). In our series, lateral radiographs were not initially taken, and anterior-posterior chest radiographs were deemed normal in 29.1% of cases, consistent with the literature. Radiographs were evaluated by pediatric surgery consultant doctors, and cross-sectional radiological assessments were performed by experienced radiologists, showing no discrepancies in interpretations between raters.
CT scans can provide high diagnostic reliability for patients when SPM cannot be confirmed by direct radiographs and clinical suspicion persists. However, CT is unnecessary for diagnosing SPM when the classical triad is detected and pneumomediastinum is evident on a chest X-ray (9, 17).
Contrast-enhanced esophagograms were conducted on 23 patients in the pediatric surgery clinic, unlike Gerazounis et al., (18) who included an esophagogram in the initial examination of all their patients, our study, along with an increasing number of publications, questions the necessity of an esophagogram and which patients should undergo the procedure (9, 19-21).
No leakage was observed in any of the esophagograms in our series. After the esophagogram, patients resumed oral feeding, and mediastinitis prophylaxis was discontinued. During this period, oral feeding was halted for an average of 28 hours. The pathogenesis of SPM remains unclear, and there is no discernible cause of fragility and leakage in the alveoli, unlike the bullae and blebs seen in spontaneous pneumothorax, a similar condition. This unknown pathogenesis complicates patient management. Today, when air is observed in the mediastinum, patient management begins with excluding other secondary causes before diagnosing SPM. Although SPM typically follows a benign course free from complications, the fear of overlooking esophageal perforation remains high in the centers consulted.
Boerhaave syndrome, a specific type of spontaneous esophageal rupture, involves a transmural tear in the esophagus due to a sudden increase in intraesophageal pressure. It typically occurs in men aged 50 - 70 years with a history of excessive alcohol intake and severe postprandial vomiting and retching. In a meta-analysis study, the most frequently reported symptoms of Boerhaave syndrome were vomiting (100%), chest/epigastric pain (88%), and dyspnea (62%) (22). Patients with Boerhaave syndrome typically present with a toxic appearance, and clinical deterioration becomes apparent within the next 24 hours. Hypotension, tachycardia, and filiform pulse are common (23). In contrast, SPM primarily affects young and healthy individuals. Vomiting symptoms are rare, as observed in our series, and epigastric pain is not commonly reported. Unlike Boerhaave syndrome, symptoms regress, and radiological findings improve during patient follow-up. Despite initial presentations that may overlap with SPM, a 24-hour clinical follow-up with a thorough history and physical examination findings is essential to exclude spontaneous esophageal perforation.
In the literature review, three studies discussing the presence of pleural effusion in SPM with direct radiography were found, noting that effusion was not observed in any of those studies (8). However, Bakhos et al.'s study found the rate of effusion in the esophageal perforation group to be 31%, where they compared 13 cases of esophageal perforation with SPM patients. In these patients, the incidence of effusion increased in the following period, although not at the time of the initial presentation (24).
Further radiological examinations should be considered in patients with clinical and/or radiological suspicion of esophageal perforation after a 24-hour follow-up. However, there is ongoing debate about the next examination. While an esophagogram with fluoroscopic contrast has been accepted as the gold standard in identifying esophageal perforation (25), fluoroscopy may not always be accessible, especially in nighttime conditions and in advanced centers. An important advancement in this area is studies suggesting that contrast-enhanced CT and esophagograms have equivalent or even higher sensitivity and negative predictive value (NPV) than conventional fluoroscopic contrast esophagograms (26). In Swanson et al.'s study, which included 103 patients with suspected esophageal perforation in the emergency department, when the only finding on CT was pneumomediastinum, the NPV for esophageal perforation was found to be 100%, and the use of IV contrast did not improve examination performance (25). Fluoroscopic esophagograms do not provide additional information that alters clinical management beyond what CT provides. Since CT is accessible in most centers, it can prevent inter-center transfers, and because it can be performed at night, it can shorten the prolonged fasting period in children suspected of having Boerhaave syndrome. It should be noted that pneumomediastinum is due to a foreign body in the esophagus, although rare and can be seen, especially in pediatric patients.
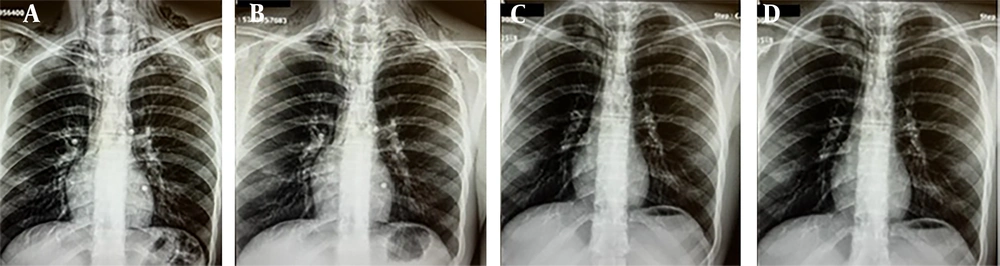
Contrast-enhanced CT can be useful for demonstrating non-opaque foreign bodies and perforation areas that cannot be seen on plain radiographs. CT also best maps the parenchyma for interstitial disease that may predispose to SPM. In emergency room patients with suspected esophageal perforation, an oral contrast CT esophagogram should be considered the first choice and is a candidate to become the gold standard (Figure 1). No clinical worsening was observed in any of our patients during the follow-up. Except for tube thoracostomy, which was performed in two of the four patients with pneumothorax, no additional procedures were required. The mean hospital stay was 4.4 days after the patients were admitted to the emergency room. Takada et al. reported that the symptoms resolved within 24 - 48 hours, but the resolution on the X-ray took about a week (27). It was observed that the longer hospital stay in our series was due to waiting for radiological improvement, and we think that it did not contribute additionally to the patients. Figure 2 demonstrates the resolution of subcutaneous emphysema over time in the daily anterior-posterior chest radiographs of the same patient from the first day to the fourth day. The patient had no symptoms on the third day.
Treatment of SPM is generally conservative and consists of bed rest and analgesics (2). Therefore, Mondello et al. argue that stable patients can be discharged from the emergency room after being informed about possible symptoms that require urgent hospitalization (28). In our series, all patients were consulted with pediatric pulmonology department, but no additional recommendations or examinations were made during the consultation. The patients came to the outpatient clinic at least two times during their follow-up, and no features were detected in the direct X-rays during the controls. The incidence of recurrence of SPM is very low (29). Kumeda et al. reported that SPM recurrence was very rare, usually seen within a year after the first attack, and showed milder clinical manifestations than the first attack (30). No recurrence was observed in our series' 9-year follow-up of 24 patients.
5.2. Conclusions
Spontaneous pneumomediastinum is a benign condition that is still under-recognized in children and young adults, often resolving spontaneously without treatment. In our series, SPM often went undiagnosed or was not treated optimally in the initial hospital setting, indicating a lack of awareness among physicians in the emergency departments. Surgeons' concerns about overlooking Boerhaave's syndrome may contribute to increased testing, prolonged fasting, and hospitalization times in SPM patients. Therefore, it is essential to be selective in further examining pediatric patients with air in the mediastinum, relying on history, physical examination, and brief follow-up for triage.
In suspected cases, oral contrast CT may serve as the gold standard for diagnosing esophageal perforation, being as sensitive and informative as a fluoroscopic esophagogram and more readily available to prevent unnecessary transfers between hospitals. If direct X-rays confirm SPM in a pediatric patient with stable vital signs and no additional clinical or radiological deterioration after 24 hours, oral nutrition initiation can be considered without an esophagogram. However, as SPM is rare, the study's main limitation is the small number of patients. Conducting a larger, multi-center prospective study would offer more robust evidence.
Managing confirmed SPM diagnoses without broad-spectrum antibiotics, shorter fasting, and reduced hospital stays is feasible.