1. Background
Neural tube defects (NTDs) occur when the neural tube fails to close completely or remains open, resulting in severe brain malformations (anencephaly, encephalocele) and/or spinal malformations (spina bifida) (1, 2). These abnormalities can lead to fetal or newborn death and lifelong complications in survivors, including motor and sensory deficits, as well as bowel and bladder incontinence (2). Due to their preventable nature, health professionals have placed significant emphasis on NTDs (3).
Typically, fetuses with NTDs are stillborn, causing early abortion in 50% of cases. Among the remaining cases that survive, various medical interventions are required, including shunts for hydrocephalus, as well as orthopedic and urological treatments (4). Birth defects of unknown etiology accounted for 18% of admissions in children's hospitals, with 40% of surgical admissions attributed to congenital malformations. It has been reported that over 137 deaths per 100,000 live births occur due to these disorders (1, 3).
In low-income countries, NTDs contribute to 29% of infant deaths among visible birth defects. As morbidity and mortality from infectious diseases decrease globally, the proportion of under-5 morbidity and mortality attributable to birth defects will increase (5). NTD assessment varies worldwide due to differences in risk factors such as socioeconomic status and surveillance (2).
Neural tube defects (NTDs) have a multifactorial origin, with genetic and environmental factors playing significant roles. However, the genetic basis is not fully understood, and questions remain regarding the mechanisms through which folic acid prevents NTDs. Folate deficiency has been shown to increase the risk of NTDs in genetically predisposed individuals (2).
The prevalence of NTDs at birth varies among different countries and is influenced by factors such as climate, race/ethnicity, and environmental conditions. Prevalence ranges from 1 in 100 live births in some regions of China to 1 in 5000 births in Scandinavia (6).
Environmental factors, including alcohol consumption, diet, nutritional status, socioeconomic status, diseases such as diabetes mellitus, drug abuse, smoking, and folic acid deficiency, as well as genetic factors such as the baby’s gender and homozygous twins, can contribute to the occurrence of these disorders (4).
Recent interventional trials have demonstrated that approximately 90% of prevalent and severe neural tube defects can be prevented by the use of multivitamins before pregnancy (at least one month prior to conception and continuing for at least two months after conception) (6). Simultaneously, about 70% of congenital heart defects can be prevented through folic acid supplementation before pregnancy. Three potential applications of this innovative primary preventive strategy for neural tube defects and congenital heart defects are (1) dietary folate intake, (2) the use of a folic acid supplement or multivitamin before pregnancy, and (3) flour fortification with folic acid (6). The European Union has set regulations to control food fortification and the addition of vitamins and minerals. Countries voluntarily enrich a broad spectrum of foods with folic acid, including flour/bread, breakfast cereals, dairy products, and fruit juices (7). In the study by Abdollahi et al., the impact of flour fortification with folic acid on reducing NTDs and improving folate status in women of childbearing age was evaluated. The average serum folate level increased from 13.6 to 18.1 nmol/L. The prevalence of folate deficiency decreased from 14.3% to 2.3% (P < 0.001). Furthermore, the incidence of NTDs in the post-enrichment period fell by 31% (P < 0.01) compared to the pre-enrichment period (8).
A 2014 review analyzing temporal trends in the incidence of NTDs and the impact of folic acid fortification on their prevalence in Latin America found significant geographic variations. In certain regions of Latin America, the prevalence of NTDs was among the lowest in the world, whereas other regions reported some of the highest rates. Over time, there was a notable decrease in the prevalence of NTDs, particularly in countries like Chile and Costa Rica, where widespread folic acid fortification reached the majority of the population at risk (9). Incorporating essential nutrients into foods, such as bread, can support the development of the neural tube structure during the fetal period, thereby reducing the prevalence of this condition. Fortification of flour with folic acid commenced in June 2007 in Golestan province, and subsequent studies, including one referenced earlier (10), have shown a decrease in the incidence of neural tube defects in this region.
2. Objectives
This study was conducted over 2 years, from 2016 to 2018, to determine the prevalence of neural tube defects, coinciding with the period of flour fortification with folic acid.
3. Methods
This descriptive-analytical study was conducted on all cases of neural tube defects in Golestan province, northern Iran, from March 1, 2016, to February 28, 2018. The Medical Ethics Committee of the Deputy Research of GOUMS approved the study (Code: IR.GOUMS.REC.1399.430). Data were collected using a questionnaire for each subject, and consent forms were completed by the parents of the subjects. The Ministry of Health, Treatment, and Medical Education initiated the plan for flour fortification with folic acid in Golestan province at the beginning of June 2007. The premix powder used for flour fortification contained 30 ppm of iron and 1.5 ppm of folic acid. Given the varying types of wheat, the total iron content in the flour was adjusted to between 80 and 85 ppm (11). The mixture for fortification, comprising 42% ferrous sulfate, 0.75% folic acid, and 57.25% corn starch, was added at a rate of 200 grams per ton of flour, effectively adding 30 ppm of iron and 1.5 ppm of folic acid.
Information on age, ethnicity, living place (city or village), parental residence within Golestan province (east, west, or center), maternal education, and types of neural tube defects was recorded for each subject.
The three primary ethnic groups residing in the area are the native Fars, Turkmen, and Sistani groups. Native Fars constitute the predominant ethnic group in the region. Turkmen migrated from Central Asia three centuries ago, while Sistanis moved to this province from the southeastern part of Iran about 70 years ago.
Golestan province, located in the north of the country, borders Turkmenistan to the north with a 438 km land border and a 90 km water border. It is adjacent to Semnan Province to the south, North Khorasan Province to the east, and Mazandaran Province and the Caspian Sea to the west. The province covers an area of 20,438 square kilometers.
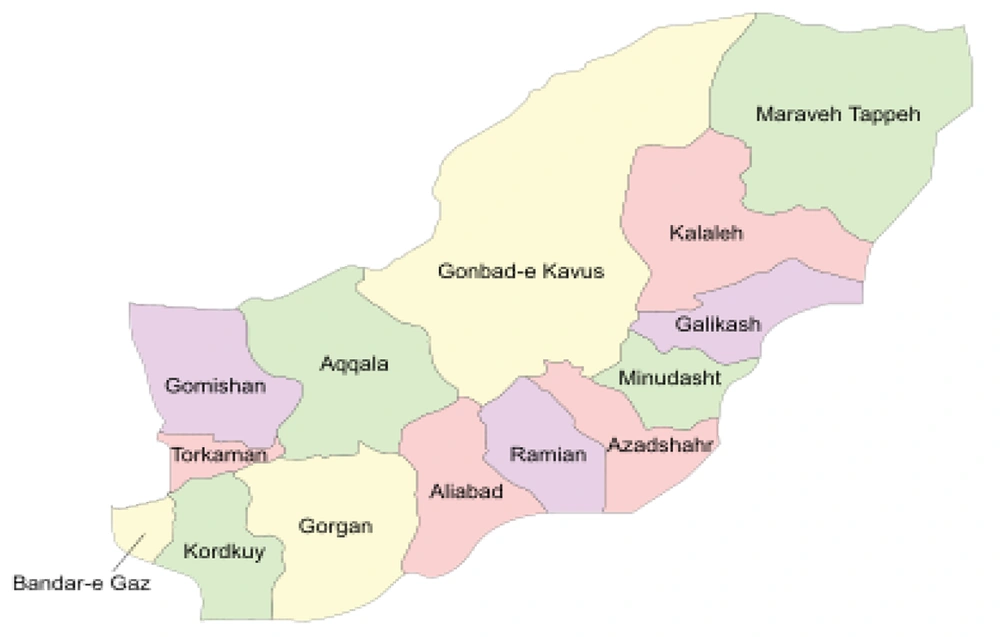
The geographical distribution of Golestan province is categorized into east, west, and center. The eastern part includes the cities of Kalaleh, Galikash, Gonbad-e Kavus, Maraveh Tappeh, Minudasht, Azadshahr, and Ramian. The central area comprises Gorgan, Aqqala, and Aliabad, while the western part encompasses the cities of Kurdkoy, Bandar Torkaman, and Bandar-e Gaz (Figure 1).
The types of NTDs were identified through pregnancy documentation, including screening tests and ultrasounds. Their classification was based on the International Classification of Diseases, Tenth Revision (ICD-10). In each hospital, 2 staff members (registered nurses) were selected and trained to review all birth records and to document and categorize NTDs. The types of NTDs recorded included anencephaly (Q00.0), spina bifida (Q05), and encephalocele (Q01), with diagnoses confirmed by a pediatrician.
Data were analyzed using SPSS version 18 statistical software. Descriptive statistics such as median, mean, and percentage frequency were utilized, and the Chi-square test (X2) was employed for analysis. In cases where non-parametric conditions were applied, equivalent non-parametric tests were used. A P value of less than 0.05 was considered statistically significant.
4. Results
During the two-year period from 2016 to 2018, this study identified 83 cases of neural tube defects, resulting in an incidence rate of 1.04 per 1000 births. Among these cases, 20 (0.62 per 1000 births) were Native-Fars, 33 (1.25 per 1000 births) were Turkmen, and 14 (1.16 per 1000 births) were Sistani. Consequently, the Turkmen ethnicity exhibited the highest incidence of neural tube defects (P value = 0.016) (Table 1).
| Variable | Deliveries No. | Frequency | Prevalence Rate Per 1000 | P-Value |
|---|---|---|---|---|
| Ethnicity | 0.016 | |||
| Fras | 31984 | 20 | 0.625 | |
| Turkmen | 26386 | 33 | 1.251 | |
| Sistani | 11994 | 14 | 1.167 | |
| Others a | 9596 | 16 | 1.876 |
a The cases whose ethnicity is not identified are classified in the others group.
In terms of geographical distribution, the western region of the province had the highest prevalence rate of NTDs at 1.87 per 1000 births, followed by 1.25 per 1000 births in the eastern region and 1.16 per 1000 births in the central region. Thus, the majority of NTD cases were found in the western part of Golestan province, with Kalaleh City reporting the highest prevalence of neural tube defects (Table 2).
| Variable | Deliveries No. | Frequency | Prevalence Rate Per 1000 | P-Value a |
|---|---|---|---|---|
| Geographical distribution of the province | 0.551 | |||
| East | 26386 | 33 | 1.251 | |
| Center | 11994 | 14 | 1.167 | |
| West | 9596 | 16 | 1.876 | |
| Unknown | 31984 | 20 | 0.625 |
a The result of the X2 test is between the three geographical regions of East, Center, and West.
Regarding maternal age, the prevalence rate of NTDs was higher in the age group under 35 years (P-value = 0.0214) (Table 3).
| Variable | Frequency (%) | P-Value |
|---|---|---|
| Age Group | 0.0214 | |
| < 35 | 67 (82.72) | |
| ≥ 35 | 14 (17.28) |
a The age of the 2 mothers was unknown.
Concerning the residency of the mothers, the prevalence rate was higher in urban areas compared to rural areas; however, the difference between these two areas was not statistically significant (Table 4).
| Variable | Deliveries No. | Frequency | Prevalence Rate Per 1000 | P-Value |
|---|---|---|---|---|
| Residency | 0.828 | |||
| Urban | 36645 | 39 | 1.064 | |
| Rural | 43315 | 44 | 1.016 |
| Variable | Deliveries No. | The Incidence Rate of Anomaly | P-Value |
|---|---|---|---|
| Years | 0.145 | ||
| 2006 - 2009 | 104232 | 0.84 per 1000 births | |
| 2016 - 2018 | 79960 | 1.4 per 1000 births |
5. Discussion
In this study, the incidence rate of NTDs was found to be 1.04 per 1000 births. A previous study conducted in Kashan city reported an incidence rate of 2.33 per 1000 births (12). Similarly, a study in Morocco found the incidence of neural tube defects to be 1 in 1000 births (13), while in Ethiopia, the rate was reported as 5.71 per 100 births (14).
In a community intervention study in Shanxi Province, China, 16,648 women of childbearing age were provided with fortified flour in eight villages, while a control group in three villages received ordinary flour. The intervention group exhibited a higher serum folate level compared to the control group. Additionally, the occurrence of NTDs in the intervention group was 68.2% lower than that in the control group, and the burden of NTDs in the intervention group was approximately 58.5% lower than in the control group. This suggests that flour fortification is linked to a reduced birth prevalence and burden of NTDs in economically developing regions with a high risk of NTDs (15).
To decrease the prevalence of NTDs, the Australian Food Regulatory Ministerial Council, in June 2007, agreed to the mandatory fortification of bread-making flour with folic acid. The regulation mandates the addition of 200 - 300 μg of folic acid per 100 grams of bread-making flour. Implemented in September 2009, this measure is estimated to prevent 14 to 49 NTDs annually in Australia, alongside existing voluntary fortification and supplement usage (16).
In the study conducted by Hosseini et al., which examined two groups of pregnant mothers, it was found that 79% of the mothers with fetuses diagnosed with neural tube defects had consumed folic acid, compared to 94% in the group of mothers with healthy fetuses. The incidence of neural tube defects was reported to be 47.1% in the first group and 16.1% in the second group (3).
A study in Brazil demonstrated that the mandatory fortification of flour with iron and folic acid was linked to a significant reduction in the prevalence of neural tube defects. The overall prevalence of neural tube defects decreased from 0.79 per 1000 births before fortification to 0.55 per 1000 births after fortification (17).
In the study by Abdollahi et al., 580 women aged 15 - 49 in Golestan province were exposed to a diet that included flour fortified with folate, which led to an increase in blood folate levels and a 31% reduction in neural tube defects (8).
Among the factors that may not fully explain the reduction in neural tube defects in our study could be insufficient time or the nonstandard and inadequate doses of folic acid used for fortification. Another contributing factor could be folic acid malabsorption due to the high prevalence of digestive disorders in this region (15).
According to the findings of this study, 82.5% of NTD cases occurred in newborns of mothers under 35 years old. In the study by Talebian et al., the mothers' ages ranged from 14 to 40 years, with no observed relationship between the mothers' age groups and pregnancies affected by neural tube defects (12). In the study by Abeywardana et al. in Australia, a significantly higher prevalence of NTDs was observed among women aged less than 25 years compared to those aged 30-34 years (16). In the study by Golalipour in 2010, the prevalence rate of neural tube defects in babies born to mothers over 35 years old was 4.89 per 1000 births, compared to 2.37 in those aged 20-34 years (18). Thus, the age of mothers can be considered a complex risk factor in the incidence and prevalence of neural tube defects.
Regarding the comparison between the ethnicity of parents and the rate of neural tube defects, this study found that the Turkmen population had the highest rate of 1.25 per 1000 births compared to other ethnicities, with the Fars ethnicity having an incidence rate of 0.625 per 1000 births. During an 8-year study by Golalipour et al. among the Fars ethnic group, the overall rate of neural tube defects was 2.54 per 1000 live births (18). In 2014, Golalipour et al., in a study of 59 mothers with babies affected by NTDs, found that the Fars ethnicity was the most frequent (64.4%), and Turkmen ethnicity was 10.2%. They also discovered that the risk of NTD incidence in the Fars ethnic group was 3.49 times that of the Sistani ethnic group (19).
In another study by Peake et al. in England, the prevalence rate of neural tube defects was 1.21 per 1000 live births, which was 1.8 times higher in Indian mothers and 2.83 times higher in Bangladeshi ethnicity than in white ethnicity (20).
Regarding the mothers' place of residence, the prevalence rate was higher in urban areas than in rural areas. This could be due to the migration of rural residents to areas around cities, leading to demographic changes in cities. In the study by Liao et al. in China, the incidence rate of neural tube defects in eight rural areas of Shanxi province was much higher than the national average, which includes villages and small towns. The causes were attributed to water pollution in the area, with elements extracted from coal mines, including mercury, nickel, and cadmium (21). The highest prevalence of NTD was associated with mothers living in rural areas. In the study by Golalipour et al., 55.9% of mothers with babies born with neural tube defects resided in rural areas (15, 19).
5.1. Conclusions
The prevalence rate of neural tube defects during the years 2016 - 2018, compared to the rate observed in our previous study conducted in this region from 2006 - 2009 (10) (Table 5), showed a relative increase, although this difference was not statistically significant. According to the findings of the current study, there was a non-significant rise in the incidence of neural tube defects compared to our earlier research. This suggests the need for additional efforts, such as enhancing mothers' awareness and knowledge about the importance of folic acid and pre-pregnancy interventions through health centers, as well as improving the provision of folic acid supplementation by these organizations.
5.2. Limitations
This study's results were measured over a limited period, and they may vary with an extended duration of data collection and analysis. Furthermore, existing studies point to some factories' failure to implement fortification or their inefficient execution of the process. This highlights inadequate monitoring and control of the fortification program by the responsible authorities.