1. Background
Today, health information is recognized as an essential element in changing the health behavior of society. People should have access to information about their diseases and related problems so that they can make informed decisions about treatment options (1). Hence, healthcare systems all over the world are looking for ways to promote self-care, patient empowerment, and informed decision-making (2).
Patient health information is provided through various channels, including individuals, public or private organizations, and mass media, in printed, electronic, and audio-visual formats (1). Patient information materials are an important factor in improving patients' health literacy. They also form the basis for collaborative decision-making regarding health and medical therapies, thus facilitating the doctor-patient relationship and improving the patient's health (3).
Today, imaging techniques such as radiography, fluoroscopy, angiography, CT scans, sonography, and MRI are essential tools for evaluating childhood disorders. These techniques can be used with or without ionizing radiation and are currently routine in children's imaging (4). Statistics show that between 2000 and 2016, there were 532 774 cases in Canada related to children, with a total of 5 439 874 cases. During this period, the use of imaging techniques in children, excluding CT scans, has increased (5). According to the latest report from the NHS in 2023, the rate of use of imaging techniques in the UK is 45 million, of which 2 659 165 are related to the use of imaging techniques in children. In general, the rate of use of imaging techniques in the country over the last year shows a 2.2 percent increase (6).
Children often have unmet informational needs when attending diagnostic and treatment centers, which may cause anxiety and uncertainty, followed by fear and a lack of agency in making choices and decisions related to healthcare. Moreover, children's lack of confidence can lead to a sense of unpreparedness, dissatisfaction, and refusal to attend diagnostic and treatment centers in the future (7).
Usually, children of different ages have distinctive limitations and challenges that affect therapeutic and diagnostic processes, including pediatric imaging techniques. They are usually unable to cooperate with the requirements of adult imaging, such as the ability to remain still and/or in a certain position, concentrate for a long time, remain, and hold their breath (8).
Considering the unique characteristics of children's imaging compared to adults, successful imaging in this group of people requires special considerations as it can be attractive and challenging for children, requiring specialized and valid training, knowledge, and expertise, as well as a variety of adapted and exclusive equipment (9).
During children's imaging, special attention should be paid to their body size, sensitivity to radiation, ability to understand and cooperate in the process, drug therapy such as contrast and anesthesia, and also the thermal and sound effects of imaging (10). Non-cooperation or additional movement of child patients during the imaging process may result in half-finished or low-quality imaging, leading to a decrease in diagnostic certainty, repeating the process, the possibility of potential risks, and additional costs. Therefore, paying due attention to children's emotional needs, providing information according to their age, and designing attractive sets of photos for children will help them to cooperate with the staff (11).
Accordingly, it is necessary to provide health information and education before performing therapeutic and diagnostic processes in order to create a clear understanding of the patients' needs, benefits, and risks. Health information improves the patients’ experience by increasing their ability to understand and predict the imaging processes (12).
The review of related literature shows that most of the studies conducted in the field of imaging have investigated the level of health literacy and awareness of parents, personnel, and adults referring to imaging centers mainly using quantitative approaches (13-24).
Despite the importance of children's health information and the necessity of preparing information content based on their needs in the imaging department, to our knowledge, almost no research has so far investigated these important issues separately. For instance, Bray et al. have examined the information needs of children from the children’s perspective using child-centered methods (write and tell) or examined the perspective of parents and staff about the treatment processes, including blood tests, surgery, and radiography in England (7). Another study has evaluated the health literacy content available on the website related to radiology processes (9). Also, Pahade et al. have addressed the preferences and demands of adults attending the imaging centers (14).
It is worth noting that various institutions, organizations, and associations, especially radiology, medical physics, and children's associations in developed countries, provide health information materials about information sharing with children, parents, personnel, and doctors with the aim of reducing the risk of exposure to false information. Among them, we can refer to “Image Gently” and “Radiology Info” (25, 26).
Despite the importance of pediatric imaging and the necessity of producing health information content based on children's needs, currently, children are not given the necessary information or training on the imaging processes. In addition, there is no structured knowledge about the production of health information content appropriate to the needs of children, especially in Iran, while according to the latest census statistics, children make up 28.8% of the country’s population (27). This issue highlights the need to produce health information tailored to the needs of children and their families in a specific period of time.
2. Objectives
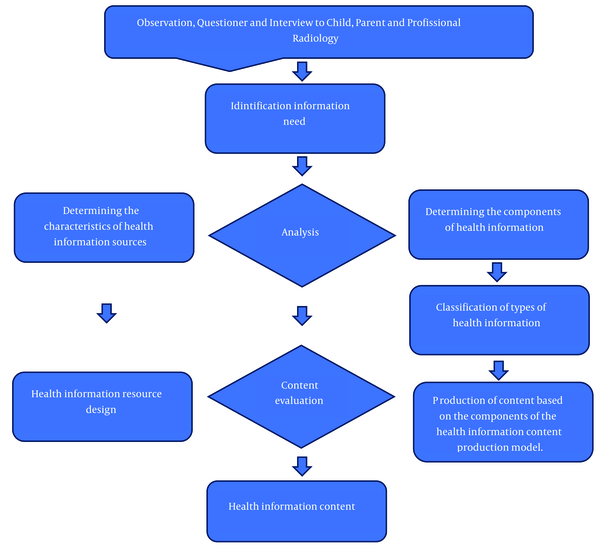
Therefore, it was firstly necessary to develop a model for producing children's health information content for imaging centers in order to investigate the information needs of children from the perspective of children, parents, staff, and doctors of imaging departments, as well as child psychologists.
3. Methods
The present qualitative exploratory case study aimed to investigate the components of children's health information in imaging centers to design a model for producing children's health information content. We adopted the protocol proposed by Eisenhardt (28) to determine the views of children, parents, and staff (radiology technicians and doctors) of imaging centers regarding the information needs of children to produce related health information content. Children over six years old, parents of children under fourteen years old, and personnel of the imaging department were selected as the most suitable (most productive) information sources for this research. Thus, 25 children aged 6 - 14 years, 25 parents of 0 - 14 years old children referring to the Imaging Department at Children's Medical Center Hospital (Tehran, Iran), and 23 radiology technicians and doctors working in the center were interviewed. The children had come to the center from different cities of Iran, including Tabriz, Khorramabad, Zabul, Sabzevar, Shahroud, Saveh, Hamedan, Kermanshah, Tehran, and others to perform various radiology examinations.
The criteria for entering the study are given in Table 1. Data collection in this research began after receiving the code of ethics and a letter of introduction from the Ethics Committee of Tehran University of Medical Sciences, and also making some arrangements with the Children's Medical Center in January 2019 for three months. It is a specialized children's center in Iran that admits clients from all over the country. Moreover, all the diagnostic processes studied in this research (imaging processes, including MRI or CT scan or ultrasound or radiography or fluoroscopy) were performed in this center.
| Inclusion Criteria for Children | Inclusion Criteria for Parents | Inclusion Criteria for Staffs (Radiology Technicians and Doctors) |
|---|---|---|
| - Not having a history of imaging; Being able to speak and understand; Being developmentally and intellectually healthy; Speaking in Farsi language and being Iranian; Aged 6 - 14 years | - Having a 0 - 14 years old child, who is developmentally and intellectually healthy; Being able to speak and understand; Speaking in Farsi language and being Iranian | - Being employed in the relevant department; Having direct communication with the patient; Being the attending physician, including pediatrician or child neurologist, and the requester of imaging process; Working in the department as staffs, who are the first people that children encounter as soon as they enter the imaging department; Being radiology technicians as people who are directly in contact with the child during the imaging process; Being radiology specialists, who are effective in carrying out some imaging processes with the child and making decisions about the imaging process; Willing to participate in the study |
Inclusion Criteria
The required data were collected from several sources (children, parents, and personnel) through observation, interviews, questionnaires, and available documents according to the studied groups. Semi-structured and in-depth interviews (lasting 15 - 30 minutes) were conducted to obtain enriched data and uncover the experiences of participants. Additionally, researcher-made observation forms were utilized to record the children's behavior before, during, and after the imaging examinations. The children's behavioral reactions were noted in the observation forms while the researcher observed their objective behavior.
Sampling was performed using a theoretical and targeted method. Participants were selected based on the type of imaging process among children and parents referring to the Radiology Department at Children's Medical Center Hospital (Tehran, Iran) for radiography, ultrasound, MRI, CT scan, or fluoroscopy. Interviews were carried out with children aged 6 - 14 years, parents of children aged 0 - 14 years, and staff (radiology technicians and doctors) at the Radiology Department of Children's Medical Center Hospital (Tehran, Iran). All participants provided written informed consent.
Qualitative data analysis, conducted using the content analysis method, revealed initial themes, concepts, and relationships between the variables. In the subsequent step, the relationships between the phenomena and the available evidence were examined. Sampling was discontinued upon reaching data saturation. Finally, through data analysis, the model for producing children's health information content in the imaging department was developed.
4. Results
4.1. Participants’ Characteristics
The research population in this study consisted of 71 individuals, comprising 25 children aged 6 - 14 years (both boys and girls), 25 parents of children aged 0 - 14 years, and 23 staff members (radiology technicians and doctors) (Table 2).
| Type of Examination and Index and Population | Residences | Education | Gender | Age | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non- native | Native | BSc. /Higher | BSc. /Lower | Male | Female | 6 - 10 | 11 - 14 | ||
| MRI | |||||||||
| Child | 3 | 2 | - | - | 2 | 3 | 3 | 2 | 5 |
| Parent | 4 | 3 | 4 | 3 | 2 | 5 | - | - | 7 |
| Technicians | 0 | 3 | 3 | 0 | 2 | 1 | - | - | 5 |
| Doctors | 0 | 2 | 2 | 0 | 0 | 2 | - | - | |
| CT | |||||||||
| Child | 2 | 3 | - | - | 3 | 2 | 3 | 2 | 5 |
| Parent | 2 | 1 | 0 | 3 | 0 | 3 | - | - | 3 |
| Technicians | 0 | 3 | 3 | 0 | 2 | 1 | - | - | 5 |
| Doctors | 0 | 2 | 2 | 0 | 0 | 2 | - | - | |
| Flouroscopy | |||||||||
| Child | 2 | 1 | - | - | 1 | 2 | 2 | 1 | 3 |
| Parent | 3 | 2 | 3 | 2 | 1 | 4 | - | - | 5 |
| Technicians | 0 | 3 | 3 | 0 | 2 | 1 | - | - | 5 |
| Doctors | 0 | 2 | 2 | 0 | 0 | 2 | - | - | |
| Radiography | |||||||||
| Child | 1 | 6 | - | - | 4 | 3 | 5 | 2 | 7 |
| Parent | 0 | 3 | 1 | 2 | 1 | 2 | - | - | 3 |
| Technicians | 0 | 3 | 3 | 0 | 2 | 1 | - | - | 5 |
| Doctors | 0 | 2 | 2 | 0 | 0 | 2 | - | - | |
| Sonography | |||||||||
| Child | 1 | 4 | - | - | 2 | 3 | 3 | 2 | 5 |
| Parent | 3 | 4 | 4 | 3 | 2 | 5 | - | - | 7 |
| Technicians | 0 | 0 | 0 | 0 | 0 | 0 | - | - | 3 |
| Doctors | 0 | 3 | 3 | 0 | 0 | 3 | - | - | |
Demographic Characteristics of the Interviewees in the Imaging Department
In qualitative data analysis, 1 683 initial codes were summarized into 483 final codes and 17 categories (Table 3). The researcher conducted direct interviews with children, parents, technicians, and doctors at Tehran Children's Medical Center. The interviews were conducted both before and after the radiology technique.
| Main Dimensions | Main Categories | Sub Categories | Quatation |
|---|---|---|---|
| Process information | How it is done | The process of doing technique; Information about the eating contrast agent; Presentation of the information about catheterization; Time spent; done frequency; how to get results; How to deliver results to the practitioner; Clothing; Holding hands and feet; Sleeping on the bed; Child placement in the imaging situation; the immobility of the child; Listening to radiology technicians | [How it is done, how long it takes, what happens here (MRI, child 1)] |
| What is done | The type and nature of the process; Title and name of the process; The degree of invasiveness of the process; Process difference and differentiation; Need to know about the process | [I wanted to know what exactly is (the procdure) (Fluoroscopy, child 2)] | |
| Why/the reason for doing it | Why/the reason the process in children's language | [They explained to me the reason for performing this examination (Radiography, child 3)] | |
| The people involved in it | The people involved | [The doctor (radiologist) should come and insert a catheter (Fluoroscopy, parent 4)] | |
| Complications or risks/benefits | The use of protective devices against exposure to radiation for parents and children; Not being exposed to radiation in case of pregnancy; Complications/benefits of catheterization; The side effects/benefits of eating contrast agent; The complications/benefits of getting a CT scan; complications or benefits of doing MRI; Complications/benefits of using gel in ultrasound | [I didn't know anything about the risks and benefits of the process (CT scan, parent 5)] | |
| Necessary preparation | The fasting period; The presence of two companions; Wearing special clothes; Removal of metal objects; The need to be still; Placement in the position of doing the process; Sleeping on the bed | [About the clothes, it depends on whether their clothes are suitable or not, or whether they have a metal object or not (MRI, parent 6)] | |
| Introduction of equipment and devices | Dimensions of the device; Device sound; How to do the process with the device | [There is a device that is supposed to take a picture (Fluoroscopy, parent 7)] | |
| Emotional information | Emotional interventions before performing the procedure | How parents talk to children; How staff interact with children and parents; How children and parents behave | “I talk to the children and prepare them mentally before doing the procedure ….” (Radiography, parent 9) |
| Emotional interventions during the process | The presence of children with the child if possible; Effective interaction based on the empathy of the technician and the doctor with the child; Talking to the child while doing the process; Child behavior | "We were with the child, and it was a little encouraging." (Fluoroscopy, parent 11) | |
| Emotional interventions after performing the procedure | Effective parent interaction; The interaction of the technicians and the doctors involved in doing process with the child, even after the process; Using the encouraging system; Child behavior | "After the examination is over, it is good to ask the child how was the process or if he/she was hurt." (MRI, parent 14) | |
| Self-regulating information | Child role | The degree of cooperation of the child with the parents, technician and doctor involved in the process; The child's compliance with the preparation instructions and necessary requirements | “We say that if you help us, it will end sooner, you will go home sooner and you will recover sooner." (Fluoroscopy, technician 17) |
| Family support | Presence of parents with the child; Parents' cooperation with the technician and doctor involved in the process; Encouraging the child to cooperate in the process | "The role of the parents is not only to accompany the child; they also need to work with us to prepare the the child." (Fluoroscopy, technician 18) |
Information About Different Aspects of the Model Is Based on Extracted Codes
Upon entering the imaging department, the researcher observed the behavior of both the child and parents, as well as the interactions between them and the staff. The information provided by the parents and reception staff was also noted through a question and answer format during the interview.
The researcher directly observed and recorded the child's emotional behaviors, such as crying, anxiety, fear, screaming, and refusal to cooperate with parents and personnel, before, during, and after the process.
Some medical procedures, such as CT scans, MRIs, and fluoroscopies, require an appointment in advance. During the appointment, the reception department will provide information about the procedure, including its content, presentation, and source. They will also assess the level of understanding and adherence of the parents or children. This information was recorded by the researcher.
The concepts, categories, and related codes are described in the following:
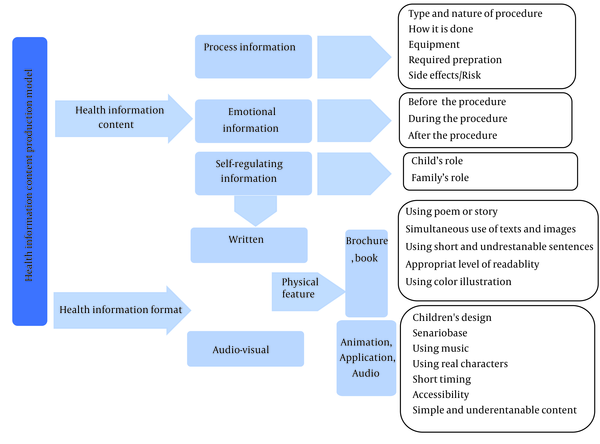
4.2. Health Information Content
Based on the analysis of qualitative data obtained from interviews and observations, one of the main dimensions of the developed model was health information content, which included process information, emotional information, and self-regulating information. In the following sections, the content of health information needed by children in the Imaging Department is explained from the perspective of children, parents, and staff members (radiology technicians and doctors) working in the department.
4.2.1. Process Information: What Children Need to Know and Do
Process information was one of the components comprising the content of health information necessary for children, according to the study participants' perspectives.
Based on the research findings, the process information required by children in the imaging department includes details such as how the procedure is conducted, what it entails, why it is performed, who is involved, potential complications or risks, benefits, necessary preparations, introduction to equipment and devices, and the environment.
According to the findings, the information children need in the imaging department pertains to how the procedure is conducted [how it is carried out, its duration, what occurs during the process (MRI, child 1)], what specifically is involved [I wanted to know exactly what the procedure entails (Fluoroscopy, child 2)], the reasons for performing it [They explained to me why this examination is necessary (Radiography, child 3)], the individuals involved [The doctor (radiologist) is supposed to come and insert a catheter (Fluoroscopy, parent 4)], potential complications or benefits [I wasn't aware of the risks and benefits associated with the procedure (CT scan, parent 5)], necessary preparations [Regarding attire, it depends on whether their clothing is suitable and if they have any metal objects (MRI, parent 6)], and an introduction to the equipment and devices [There's a device that takes pictures (Fluoroscopy, parent 7)]. These are some of the pieces of information children require when undergoing imaging procedures.
4.2.2. Emotional Information: The Child's Feelings and How to Interact with Them Based on Empathy
Emotional information constitutes another aspect of children's health information content, as perceived by children, parents, and staff (radiology technicians and doctors) in the imaging department. This aspect encompasses the experiences, emotions, and expressions demonstrated by children before, during, and after the process, along with their expectations of more interactive engagement from personnel during their visit to the imaging department. The codes are categorized into three segments concerning feelings before, during, and after the process, derived from the researcher's direct observations throughout the procedure.
Emotional interventions before the procedure involve (1) providing verbal information by the doctor or radiology technician prior to commencing the procedure; (2) offering verbal reassurance by parents beforehand:
"I explain step by step to children what I'm going to do before proceeding to alleviate their stress because I notice they are anxious and frightened. Based on my experience, I see that after a bit of noise, they calm down, and then we proceed with the procedure." (Fluoroscopy, technician 8)
"I communicate with the children and mentally prepare them before initiating the procedure…" (Radiography, parent 9)
"It would be comforting if the doctor told me to go ahead with the radiography and not to be scared..." (Radiography, child 10)
Emotional interventions during the procedure comprise (1) parental presence with the child; (2) empathetic engagement by the doctor or radiology technician with the child:
"We were there with the child, and it provided some encouragement." (Fluoroscopy, parent 11)
"I hoped they would interact with my child in a kind and sympathetic manner, just as I had spoken to my son and prepared him." (Fluoroscopy, parent 12)
"I wished that when I entered the technician's room, she would speak to me kindly and not angrily…" (MRI, child 13)
Emotional interventions after the procedure involve (1) seeking feedback from the child regarding their experience; (2) offering the child a reward or encouragement; (3) bidding farewell to the child with kind words from a doctor or radiology technician:
"It's beneficial to inquire how the child found the process or if they experienced any discomfort afterward." (MRI, parent 14)
"Even a small token after the procedure is beneficial. For instance, the child would be delighted with a small reward." (Fluoroscopy, parent 15)
"It's nice to see the child off with a smile and kind words to ensure they have a positive experience." (CT scan, parent 5)
"After it was done, I wished she would give me a reward, as I really enjoy receiving one…" (MRI, child 16)
4.2.3. Self-regulating Information: The Child Controls and Regulates Their Behavior
Another critical aspect of health information content is self-regulation information, which pertains to the child's ability to control and regulate their behavior, along with the role of family support in the child's adjustment to the imaging procedure.
Based on the findings of this study, nearly all participants (children, parents, and imaging department personnel) emphasized the importance of children's involvement in making the process as comfortable as possible:
"We tell them that if they cooperate, the procedure will finish sooner, and they can return home and recover faster." (Fluoroscopy, technician 17)
The level of children’s cooperation with parents, technicians, and doctors during the imaging process, as well as their adherence to preparation instructions, are crucial roles they can play in this regard.
The presence of families and their support for the child during the procedure are types of information deemed necessary for children attending the imaging department, as perceived by children, parents, and department personnel. This includes parents accompanying their children, cooperating with technicians and doctors involved in the process, and encouraging children to cooperate during the procedure:
"The role of parents isn't just to accompany the child; they also need to assist us in preparing the child." (Fluoroscopy, technician 18)
Family support is most evident in procedures where parents are permitted to be present and accompany the child.
4.3. Health Information Format
Based on the research results, the health information format was another dimension of the model for producing children's health information content in the imaging department. Information brochures, books, animations/films, oral explanations, and applications, along with their features, are some of the information types and formats related to this dimension of the model that are introduced in Figures 1 and 2.
5. Discussion
The findings of the study suggest that the health information content model can be utilized to determine the type and nature of health information required in radiology departments. This involves identifying the features needed from the perspective of children, parents, and imaging personnel to prepare children for imaging techniques. Currently, there is no comprehensive model available that specifically addresses the information needs of children. It is important to develop such a model to ensure that the required information resources are available.
5.1. Type of Health Information Content
The results of the study indicate that information required by children in the radiology sector can be classified into three main categories: (1) Procedural information; (2) information about the nature of the procedure; (3) information on how to perform imaging techniques. Additionally, the study evaluated the information needs of children in radiography, laboratory, and surgery. The study's results included information on children in three main categories: (1) Functional information; (2) emotional information; (3) self-regulation information (7).
In this study, although other diagnostic measures were evaluated, the required information components regarding the child's health, including the type and nature of health information, were found to be no different from the results of this study. These findings suggest that the results of this study may be applicable to other therapeutic and diagnostic environments.
5.2. Educational Health Information/Patient Education
Identifying the types and content of health information needed for children in imaging studies is a crucial aspect of the child health information content model. This can provide appropriate health information education for children, increasing their health literacy in both educational and treatment settings. Parents, radiographers, physicians, and even educational institutions such as schools, media, and television can play a role in providing information to patients and non-patients to increase their awareness in dealing with diagnostic and therapeutic centers.
Based on the study's findings, it appears that parents, as the primary caregivers of their children, lack sufficient knowledge regarding radiology techniques that are necessary for both the child and the parents to know (29). International campaigns have emphasized the importance of parents' awareness and access to information about children's radiology, particularly techniques that use ionizing radiation. Educational content related to children's radiology is available in English (30).
5.3. Health Information Sources
The model extracted from this study can be used to design written and audio-visual educational resources, including films, animations, applications, books, stories, poems, brochures, and pamphlets for children. The study conducted in the radiology department revealed a lack of suitable informational and educational resources for children and their parents. However, the effectiveness of various educational interventions, including the use of informational resources for children and their parents, was confirmed. The results of these studies support the design of a model for producing health information content (31-34).
According to the study results, audio-visual content, particularly animation and applications, were found to be more acceptable for providing information to children. This finding is consistent with Abuzaid et al.'s study, which also reported a higher acceptance rate for audio-visual content compared to written and printed information, as well as a higher level of content comprehension. To enhance the understanding of health information, it is recommended to provide it in both audio and visual formats (12).
This study examines the perspective of children and their parents as an information-consuming society to determine the necessary characteristics or components for designing information resources appropriate to children's level of understanding and knowledge. The design of information resources should be based on their informational and appropriate needs. Improving educational or therapeutic outcomes will follow in an information-consuming society. The results mentioned are in line with studies that have used the community-based participation model to design informational content for patients (35).
5.4. Assessment Tool of Health Information Content
The model for generating children's health information content includes components that can be used to evaluate informational and educational content sources in diagnostic and therapeutic departments. Standard indicators of health literacy, such as PEMAT, are used to evaluate the characteristics and components of written and non-written educational materials in terms of readability, comprehensibility, and applicability (36).
One limitation of this study is the possibility of limited generalization due to its single-center design. However, the diversity of visitors to this center and the company in this study may be transferable to other imaging centers in other Iranian cities. Another limitation of the study is the use of qualitative methods, which cannot be used for statistical analysis.
5.5. Conclusions
The design of a model for the production of health information content can help provide the required information to parents, children, and staff about the process of imaging examinations in a diversity of audio-visual and written formats, including information brochures, books, educational animations, and application programs. The results of this study can further assist parents, staff, and doctors working in imaging departments in providing children with the required information. Health information content produced according to the needs of children can act as a suitable platform for the transfer of information to them in imaging centers. Additionally, due to the limited time of doctors and radiology technicians in providing information to children, the use of attractive and diverse information contents through animation and applications would play a significant role in the efficient transfer of information to children. Finally, the results of this study can be applied in other therapeutic settings as well.