1. Background
Viral encephalitis (VE) refers to acute intracranial inflammation primarily caused by various viral infections and clinically manifests with symptoms such as fever, vomiting, and convulsions. In severe cases, it can lead to motor dysfunction and disorders of consciousness (1). Children with VE, especially those with acute VE, often experience a prolonged course of illness and multiple complications, making subsequent rehabilitation nursing more challenging (2). The acute onset of VE frequently induces cerebral edema, which can lead to seizures in severe cases, eventually resulting in multiple mental and physical dysfunctions (3). Consequently, it is challenging for children with acute VE to achieve desirable treatment outcomes, which can further impact their recovery, exacerbate sequelae, and increase the risk of disability.
Currently, there are no specific drugs available for the clinical treatment of VE. Symptomatic treatment is used to alleviate the clinical symptoms of children and reduce the extent of viral infections, with some cases achieving favorable results (4). However, the majority of children with VE, especially those with acute VE, experience sequelae such as limb spasticity and motor dysfunction after recovery, which seriously affects their daily lives. Therefore, symptomatic treatment should be combined with targeted rehabilitation nursing interventions for children with VE to achieve more desirable clinical outcomes (5).
Rehabilitation nursing effectively improves the swallowing function in children with viral encephalitis (VE), promoting the effective intake of nutrients and thus enhancing their quality of life (6). The timing of nursing interventions for children with VE is closely related to their recovery time and the efficacy of the nursing care (7). However, determining the optimal timing is challenging, as these children often experience severe and rapid deterioration in a short period of time (8). Rehabilitation nursing interventions for children with acute VE can begin from the 2nd or 4th week after admission (9), but the benefits and drawbacks of these timings remain a topic of debate.
2. Objectives
Therefore, we evaluated the effect of early (2nd week after admission) and late (4th week after admission) rehabilitation nursing interventions on children with acute viral encephalitis (VE), aiming to provide valuable evidence for clinical treatment.
3. Methods
3.1. Study Design
This was a retrospective clinical study.
3.2. Case Selection
Sixty children with acute viral encephalitis (VE) were selected as subjects for this study. They were divided into two groups: An early intervention group (n = 30, where rehabilitation nursing started from the 2nd week after admission) and a late intervention group (n = 30, where rehabilitation nursing began from the 4th week after admission).
The inclusion criteria were as follows:
(1) Children meeting the diagnostic criteria for VE (10), (2) those in the acute phase of their condition, (3) those aged 3 - 12 years, (4) those whose caregivers gave informed consent for participation in the study, and (5) those in whom VE occurred within 72 hours.
The exclusion criteria included:
(1) Children with motor dysfunction not caused by VE, (2) those with limb spasticity not resulting from VE, (3) those with other infectious diseases, and (4) those with organ functional abnormalities.
3.3. Methods
Rehabilitation nursing interventions were applied to both groups after assessing the severity of the disease. The intervention commenced in the second week after admission for the early intervention group and in the fourth week for the late intervention group, continuing for a total of four weeks. The details of the rehabilitation nursing are as follows:
(1) Basic Clinical Nursing: Children with acute VE were provided with a quiet and comfortable hospital environment. Their private areas were kept clean, and their skin was regularly wiped with warm water to maintain moisture and prevent pressure sores.
(2) Functional Exercise: Nursing staff regularly turned the children to inspect and record skin conditions. They also assisted the children with acute VE in performing limb exercises. The sequence for upper limb exercises was from shoulder to elbow, wrist, and fingers, while for lower limbs, it was from hip to knee and ankle. Limbs and joints were exercised opposite to the direction of their contracture, gradually (30 minutes each session, twice daily). If children with acute VE exhibited low muscular tension, they received massages. Each joint was massaged multi-dimensionally (15 - 30 minutes per session, 4 - 6 times daily) from proximal to distal ends and from upper to lower limbs. During massage, the rhythm was kept slow and the pressure gentle to promote blood circulation in the limbs.
(3) Music Intervention: Songs were selected according to the children's preferences and played early in the morning (once daily), with adjustments made based on the children’s mood during playback.
(4) Psychological Nursing: Nursing staff provided psychological support to both the children with VE and their parents, tailored to their specific situations. Given that parents of children with VE were often nervous and anxious due to the serious condition and high risk of complications, the nursing staff actively communicated with them, disseminated relevant knowledge, and guided them to participate actively in the rehabilitation training of their children.
3.4. Observation Indicators and Evaluation Criteria
(1) Limb Spasticity: Before nursing and at 4 weeks after nursing, limb spasticity was compared between the two groups using the Modified Ashworth Scale (MAS) (11). The criteria are as follows:
- Grade 0: No increase in muscular tension, and no resistance to passive movement of the affected limb.
- Grade I: Slight increase in muscular tension, with minimal resistance to passive flexion and extension of the affected limb.
- Grade II: Moderate increase in muscular tension, with a sudden pause within 50% of the range of motion (ROM) during passive flexion and extension, followed by minimal resistance.
- Grade III: Significant increase in muscular tension within the majority of ROM during passive movement of the affected limb, with high ease of movement.
- Grade IV: Stiffness of the affected limb during passive flexion and extension, and inability to move.
(2) Daily Living Ability: Before nursing and at 4 weeks after nursing, daily living ability was compared between the two groups using the Activities of Daily Living (ADL) scale (12). This scale evaluates functions such as eating, walking, dressing, and control of defecation and urination, with a total score of 0 - 100 points. A higher score indicates better daily living ability in children with acute VE.
(3) Motor Function: Motor function was compared between the two groups before nursing and at 4 weeks after nursing. Gross motor function was evaluated using the Gross Motor Function Measure-88 (GMFM-88) scale (13), which is scored as follows:
- 0 points: Unable to initiate or completely unable to move.
- 1 point: Able to complete 0 - 10% of the task.
- 2 points: Able to complete 10 - 99% of the task.
- 3 points: Able to complete 100% of the task.
(4) Rehabilitation Nursing Efficacy: The efficacy of rehabilitation nursing—which includes the time for recovery from convulsions, cranial nerve disorders, and consciousness disorders—was compared between the two groups in children with acute VE.
3.5. Statistical Analysis
SPSS 26.0 software was used to test the normality of measurement data. The normally distributed measurement data were expressed as mean ± standard deviation (x ± s). Intergroup comparisons were performed by the independent-samples t-test, and intragroup comparisons were conducted with the paired t-test. The count data were represented as percentage [n (%)] and analyzed using the χ2 test. The rank data were subjected to the rank sum test. P < 0.05 was considered statistically significant.
4. Results
4.1. Baseline Clinical Data
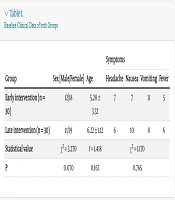
There were no statistically significant differences in baseline clinical data, including gender ratio, age, and symptoms, between the two groups (P = 0.070, 0.162, 0.765) (Table 1).
| Group | Sex [Male/Female] | Age | Symptoms | |||
|---|---|---|---|---|---|---|
| Headache | Nausea | Vomiting | Fever | |||
| Early intervention (n = 30) | 12/18 | 5.20 ± 3.32 | 7 | 7 | 11 | 5 |
| Late intervention (n = 30) | 11/19 | 6.22 ± 1.12 | 6 | 10 | 8 | 6 |
| Statistical value | χ2 = 3.270 | t = 1.418 | χ2 = 1.170 | |||
| P | 0.070 | 0.162 | 0.765 | |||
4.2. Limb Spasticity
At 4 weeks after nursing, the limb spasticity of the early intervention group was significantly ameliorated compared to that of the late intervention group (P = 0.005) (Table 2).
| Group | n | Before Nursing | 4 Weeks After Nursing | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Grade 0 | Grade I | Grade II | Grade III | Grade IV | Grade 0 | Grade I | Grade II | Grade III | Grade IV | ||
| Early intervention | 30 | 0 | 0 | 8 | 12 | 10 | 0 | 8 | 9 | 5 | 8 |
| Late intervention | 30 | 0 | 0 | 7 | 10 | 13 | 0 | 2 | 1 | 14 | 13 |
| Z | 0.678 | 2.803 | |||||||||
| P | 0.498 | 0.005 | |||||||||
4.3. Daily Living Ability
At 4 weeks after nursing, the daily living ability of the early intervention group was significantly superior to that of the late intervention group (P = 0.024) (Table 3).
| Group | Daily Living Ability (Point) | Motor Function Score (Point) | Time for Recovery from Convulsion (day) | Time for Recovery from Cranial Nerve Disorder (day) | Time for Recovery from Consciousness Disorder (day) | ||
|---|---|---|---|---|---|---|---|
| Before Nursing | 4 Weeks After Nursing | Before Nursing | 4 Weeks After Nursing | ||||
| Early intervention (n = 30) | 51.63 ± 21.24 | 63.54 ± 17.56 | 50.62 ± 20.36 | 62.45 ± 15.25 | 5.54 ± 2.25 | 3.12 ± 1.07 | 5.00 ± 1.32 |
| Late intervention (n = 30) | 50.85 ± 18.55 | 53.99 ± 14.22 | 52.66 ± 15.45 | 48.22 ± 15.46 | 8.00 ± 3.44 | 9.49 ± 3.86 | 9.00 ± 2.26 |
| t | 0.151 | 2.314 | 0.440 | 3.600 | 3.280 | 8.710 | 8.371 |
| P | 0.880 | 0.024 | 0.660 | 0.001 | 0.002 | < 0.001 | < 0.001 |
4.4. Motor Function
At 4 weeks after nursing, the motor function score was significantly higher in the early intervention group than in the late intervention group (P = 0.001) (Table 3).
4.5. Outcomes of Rehabilitation Nursing
The recovery time from convulsions, cranial nerve disorders, and consciousness disorders was shorter in the early intervention group than in the late intervention group (P = 0.002, < 0.001, < 0.001) (Table 3).
5. Discussion
In this study, the improvement in limb spasticity in the early intervention group was significantly greater than that in the late intervention group, and the time for recovery from clinical symptoms and signs was significantly shorter in the early intervention group compared to the late intervention group. These findings suggest that early rehabilitation nursing (starting from the 2nd week after admission) is beneficial for alleviating limb spasticity and reducing recovery time for clinical signs in children with acute viral encephalitis (VE). The possible reasons are as follows:
First, early rehabilitation nursing, including mask oxygen inhalation, can increase the oxygen content in brain tissues, improve blood and oxygen supply, reduce degeneration and necrosis of nerve cells, and thus promote the recovery of cranial nerve functions (14).
Second, early rehabilitation nursing facilitates regular motor training, accelerates metabolism, promotes blood circulation in the brain region, reduces abnormal discharge of cerebral neurons caused by brain cell injury, prevents convulsions, and shortens recovery time from convulsions in children with acute VE (15).
Third, techniques such as limb massage, skin care, and regularly turning the body over are employed in early rehabilitation nursing to enhance the children's perception of themselves and their environment, improving their cooperation with clinical treatment, thus promoting the recovery of limb function and alleviating limb spasticity (16). It has also been reported that rehabilitation nursing significantly facilitates the recovery of motor function and ameliorates limb spasticity in children with acute VE (17).
The results of this study showed that the GMFM-88 score was higher in the early intervention group than in the late intervention group after 4 weeks of intervention. From the perspective of functional recovery (18), the early abnormal motor pattern has not yet been established, and brain function development during this period exhibits strong plasticity (19). Therefore, gradually increasing exercise and continuously providing benign stimulation to children with acute VE during this period can stimulate the repair of their central nervous system (20), thus promoting the recovery of motor function. In contrast, since the compensatory capacity for brain function development in children with acute VE is limited and faulty motor patterns may exist in severe cases, their motor function can hardly improve after rehabilitation nursing starts from the 4th week after admission, which is not conducive to prognosis (21).
Furthermore, we found that psychological nursing interventions helped children and their parents release negative emotions and accelerate physical self-healing, thus alleviating their psychological stress. Music intervention has proven effective in ameliorating language impairments in children with acute viral encephalitis (VE) (22). Listening to music helps stabilize emotions and improve the mood of children with VE. Music intervention enhances socially responsive behavior, verbal communication skills, and mobilizes motivation in children with VE (23). Functional exercises accelerate local blood circulation, promote the repair of damaged peripheral soft tissues, prevent complications such as muscle atrophy and joint stiffness, reduce muscular tension in affected limbs, and improve limb spasticity (24). Overall, rehabilitation nursing significantly promotes the recovery of children with VE, with early rehabilitation nursing being a key measure to accelerate their physical recovery.
In conclusion, early rehabilitation nursing holds significant clinical value for children with acute viral encephalitis (VE), as it can markedly improve motor function and reduce limb spasticity, thus facilitating physical recovery. However, this study has limitations. Being retrospective, it may be subject to bias. Further prospective studies are needed to confirm these findings.