1. Background
Deep vein catheterization is currently the main puncture technique for the clinical rescue of critically ill children. It is widely used for repeated intravenous infusion, blood transfusion, hemodialysis, total parenteral nutrition, and central venous pressure detection. This technology can reduce the damage of viscous or irritant drugs to veins and also reduce the pain of repeated venipuncture in children (1). However, it still has its unique problems, such as deep vein thrombosis (DVT). In the latest consensus document "Diagnosis and Management of Acute DVT" (2) published by the European Society of Cardiology (ESC) in 2021, indwelling venous catheters are clearly defined as an important risk factor for DVT.
Traditional clinical nursing for critically ill children mainly focuses on ensuring unobstructed pipelines, avoiding twisting, folding, and compression, regularly sealing the tubes, and replacing dressings if necessary. However, these measures have little effect on DVT prevention in critically ill children. Near-infrared spectroscopy (NIRS) is a non-invasive, real-time monitoring technique for local tissue oxygen saturation (crSaO2). It has become a non-invasive method for continuously evaluating micro-circulation, local tissue hypoxia, and monitoring tissue perfusion (3). Near-infrared spectroscopy can penetrate human tissues to measure the proportion of oxygenated hemoglobin and deoxygenated hemoglobin in tissues, thereby assessing tissue oxygen metabolism status (4). Oxygen is essential for maintaining life activities and the function of tissues and cells in the body. When the body is in a state of hypoxia, it can lead to functional and metabolic disorders. Clinicians focus on the oxygenation status and tissue oxygen metabolism of critically ill children (5).
Foreign scholars have conducted extensive research on using NIRS to detect DVT, but there are few relevant reports in China. Helmelt et al. (6) used blood model experiments to test the potential of NIRS in DVT detection. Scott et al. (7) used NIRS technology combined with the occlusion ischemia test to measure the difference in HbO2 and Hb in the legs of normal and DVT patients. Hosoi's team and Yamaki's team reported experiments in detecting thrombus by measuring Hb and obtaining the venous retention index under exercise paradigm conditions (8, 9).
Therefore, this study investigates the risk analysis of DVT and the effectiveness of targeted nursing measures for lower limb crSaO2 detection in children with indwelling catheters through NIRS. The report is now elaborated as follows.
2. Methods
2.1. General Information
Eighty children with indwelling catheters admitted to the first pediatric intensive care unit of our hospital from January 2022 to December 2022 were selected as the study subjects. According to ultrasound imaging examinations, they were divided into two groups: The DVT group (N = 20) and the non-DVT group (N = 60). The sixty non-DVT patients were randomly divided into a study group and a control group using a random number table method, with 30 patients in each group. Both groups' families were informed of the purpose of this survey and signed informed consent forms. This study is in accordance with the declaration of Helsinki (10) and has been approved by the Medical Ethics Committee.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria: (A) age between 28 days and 14 years; (B) catheter placed in a deep vein after admission; (C) legal guardian agrees and signs the informed consent form.
Exclusion criteria: (A) trauma and shock caused by various reasons; (B) coagulation dysfunction; (C) previous history of thrombosis; (D) previous physical activity disorders.
2.3. Survey Methods
Children were divided into a DVT group (N = 20) and a non-DVT group (N = 60) based on whether DVT had occurred. The gender, age, puncture site, catheter type, Body Mass Index (BMI), bed rest time, limb immobilization, serum albumin (ALB), fibrinogen (FIB), white blood cell count (WBC), and D-dimer (D-D) of the children were recorded.
2.4. Research Method
Sixty non-DVT children were randomly assigned using a number table, and the following nursing measures were taken.
2.4.1. Control Group
The control group received routine nursing measures. After catheterization, the puncture site was cleaned, and sterile dressings were replaced daily at regular intervals.
2.4.2. Study Group
In addition to the measures taken by the control group, nursing interventions were implemented to assess the DVT risk through lower limb crSaO2 detection in children with indwelling catheters using NIRS. The detailed procedures are as follows: (1) Preliminary settings: Select two wavelengths of near-infrared light at 730 nm and 810 nm, maintaining a distance of 2.8 cm between the light source and the detector; (2) detection method: Place the detection probe on the skin surface of the gastrocnemius muscle of both legs, transmit the signal to the host through optical fiber, and read the crSaO2 value of the child's lower limbs. Detect every 4 hours for 20 minutes each time, considering 60 - 65% as normal. Multidisciplinary team nursing measures are implemented based on different levels, with specific nursing measures shown in Table 1.
| Operators | Responsible Nurse and Attending Physician | Responsible Nurse and Rehabilitation Specialist | Dietitian |
|---|---|---|---|
| Risk free lower limb crSaO2: 60 - 65% | (1) ensure unobstructed pipelines;(2) avoid twisting, folding, and compression; (3) timing sealing; (4) replace the dressing if necessary. | Guide children to engage in normal activities without disease restrictions. | Maintain a normal diet |
| Low risk lower limb crSaO2: 55 - 59% a | (1) assess whether there is pipeline compression or restricted posture; (2) regularly observe blood circulation, skin color, and swelling; (3) measure the circumference of the lower limbs and record it in the nursing record. If there is a difference of 2 cm in the measured dimensions of both legs, the attending physician should be notified immediately. | Regularly roll over: Roll over every 2 hours and maintain the position for 30 minutes once | 28 d – 18 m children: Regular infant formula powder, residue free complementary food; Children ≥ 19 m: Partial oral feeding, partial nutrient support with enteral nutrition |
| Moderate risk lower limb crSaO2: 50 - 54% b | (1) is there a low body temperature? If the body temperature is less than 36.0℃, a hat or hand and foot warmer should be worn, and a care towel should be used to cover the abdomen and lower limbs; (2) for the infusion liquid, keep it at a constant temperature of 37.0℃. | Local massage: Spread a massage towel on the surface of the Gastrocnemius muscle skin of both legs, slowly massage from the foot tip to the lower leg to the knee joint, 30 - 50 times each time, twice a day. | 28 d – 18 m children: Regular infant formula powder, residue free complementary food; Children ≥ 19 m: Adjust the amount of enteral and parenteral nutrition support according to the digestive status of the child |
| High risk lower limb crSaO2: 45 - 49% c | (1) anticoagulant therapy (2) warfarin treatment | Passive movement: Slowly press down on the foot surface to hold the action for 5 seconds; rest for 1 - 2 seconds; press the foot up and hold for 5 seconds; rest for 1 - 2 seconds; rotate left and right and hold for 5 seconds, rest for 1 -2 seconds. 30 - 50 times per session, 2 - 3 times per day | 28 d – 18 m children: Regular infant formula powder, residue free complementary food; Children ≥ 19 m: complete parenteral nutrition support |
a Low risk lower limb crSaO2: 55 - 65%.
bModerate risk lower limb crSaO2: 45 - 55%.
c High risk lower limb crSaO2: 35 - 46%.
2.5. Observed Indicators
2.5.1. Biochemical Examination
Nursing staff extracted 5 mL of peripheral venous blood from the patient on an empty stomach in the morning and sent it to the biochemical laboratory after 3 days (T0), 7 days (T1), and 14 days (T2) of catheterization. The laboratory personnel performed 1:9 anticoagulation with 0.109 mmol/L sodium citrate and centrifuged the samples at a rate of 3000 r/min for 10 minutes. Plasma was collected using a fully automated coagulation analyzer for immunoturbidimetric detection of thrombin time (TT), activated partial thromboplastin time (APTT), FIB, D-D levels, WBC, and ALB.
2.5.2. Symptoms Related to Lower Limb Deep Vein Thrombosis
Lower leg pain, skin flushing, elevated skin temperature, limb swelling, and incidence of limb stiffness were monitored. Bedside ultrasound examinations were conducted by ultrasound room personnel to detect the occurrence of DVT.
2.6. Quality Control
(A) the nursing staff participating in this survey received a 4-week training. After training, an assessment score of ≥ 95 points was considered a pass. If the assessment was not passed, additional training was required until a passing score was achieved; (B) to avoid contamination issues, the two groups of patients were placed on opposite sides of the ward. Patients and their families were informed to prevent conversations between the two groups regarding the content of this study and the effectiveness of nursing care; (C) to ensure the authenticity of data collection, the personnel involved in data collection were not the same as those performing the nursing operations.
2.7. Data Collection
A total of 60 questionnaires were distributed in this study. The entire process was completed in the hospital, with participation from all staff under the supervision and encouragement of the nursing staff. All 60 questionnaires were returned and deemed valid, resulting in a 100% response rate.
2.8. Statistical Analysis
SPSS 27.0 was used to process and analyze the data, and the Kolmogorov-Smirnov test was used to verify whether the data conformed to a normal distribution. The measurement data are represented by the mean ± standard deviation (SD). Independent t-tests were conducted between groups, and paired t-tests were conducted within groups. Repeated measures analysis of variance was performed on repeated measurement data. The number and percentage of data use cases [n (%)] were counted, and χ2 tests were performed. Logistic regression analysis was conducted on items with P < 0.05 in univariate analysis, and the regression coefficients (β), standard error (SE), odds ratio (OR), and 95% confidence interval (CI) for each item were recorded. P < 0.05 indicates a statistically significant difference.
3. Results
3.1. Single Factor Analysis of Deep Vein Thrombosis in Critically Ill Children Undergoing Catheterization
The results of the univariate analysis showed that bedtime, limb immobilization, WBC, FIB, D-D, and ALB were the influencing factors (P < 0.05) for critically ill children with catheterization (Table 2).
| Indicators | DVT Group (N = 20) | Non-DVT Group (N = 60) | P | |
|---|---|---|---|---|
| Gender | 0.017 | 0.897 | ||
| Male | 11 | 32 | ||
| Female | 9 | 28 | ||
| Age of years | 8.51 ± 1.46 | 7.95 ± 2.01 | 1.147 | 0.255 |
| Puncture site | 0.818 | 0.664 | ||
| Femoral vein | 18 | 57 | ||
| Jugular vein | 1 | 2 | ||
| Sub-clavian vein | 1 | 1 | ||
| Conduit model | 3.118 | 0.210 | ||
| 6F | 3 | 19 | ||
| 8F | 4 | 15 | ||
| 11F | 13 | 26 | ||
| BMI (kg/m2) | 17.35 ± 2.01 | 18.01 ± 1.16 | 1.807 | 0.075 |
| Bed rest time (d) | 4.689 | 0.030 | ||
| < 3 | 3 | 25 | ||
| ≥ 3 | 17 | 35 | ||
| Limb braking | 7.742 | 0.005 | ||
| Yes | 13 | 18 | ||
| No | 7 | 42 | ||
| ALB (g/L) | 35.38 ± 2.16 | 36.23 ± 0.51 | 2.851 | 0.006 |
| WBC (×109/L) | 9.41 ± 1.39 | 7.42 ± 2.24 | 2.044 | 0.044 |
| FIB (g/L) | 3.89 ± 1.19 | 2.55 ± 1.65 | 3.347 | 0.001 |
| D-D(mg/L) | 15.21 ± 2.13 | 14.09 ± 1.16 | 2.988 | 0.004 |
Abbreviations: DVT, deep vein thrombosis; BMI, Body Mass Index; ALB, albumin; WBC, white blood cell; FIB, fibrinogen; D-D, D-dimer.
a Values are expressed as No (%) or mean ± SD.
3.2. Logistic Regression Analysis of Deep Vein Thrombosis in Critically Ill Children with Catheterization
This study used DVT as the dependent variable in critically ill patients with catheterization and used bed rest time, limb immobilization, WBC, FIB, D-D, and ALB as independent variables (assignment method shown in Table 3) for multiple logistic regression analysis. The results showed that bed rest time ≥ 3 days, limb immobilization, FIB, and D-D were all independent risk factors affecting DVT in critically ill patients with catheterization (P < 0.05) (Table 3).
| Variables | Assigned Method |
|---|---|
| Dependent variable | DVT in critically ill children with catheterization |
| Independent variable | |
| Bed time | < 3 = 0, ≥ 3 = 1 |
| Limb braking | No = 0, Yes = 1 |
| WBC | Input with original value |
| FIB | Input with original value |
| D-D | Input with original value |
| ALB | Input with original value |
Abbreviations: DVT, deep vein thrombosis; ALB, albumin; WBC, white blood cell; FIB, fibrinogen; D-D, D-dimer.
3.3. Logistic Regression Analysis on the Impact of Deep Vein Thrombosis on Critically Ill Children
According to multivariate logistic analysis, bed rest time ≥ 3 days, limb immobilization, FIB, and D-D were independent risk factors for DVT in critically ill children with deep vein catheterization (P < 0.05) (Table 4).
| Projects | B | S.E. | Wald χ2 | P | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||
| Constant | -23.267 | 9.998 | 5.416 | 0.020 | 0.000 | - | - |
| Bed time ≥ 3 days | 1.086 | 0.428 | 6.452 | 0.011 | 2.963 | 1.282 | 6.852 |
| Limb braking | 1.045 | 0.436 | 5.735 | 0.017 | 2.843 | 1.209 | 6.685 |
| FIB | 4.056 | 0.832 | 23.764 | < 0.001 | 57.765 | 11.308 | 295.094 |
| D-D | 1.228 | 0.457 | 7.236 | 0.007 | 3.415 | 1.396 | 8.359 |
Abbreviations: FIB, fibrinogen; D-D, D-dimer, OR, odds ratio; CI, confidence interval.
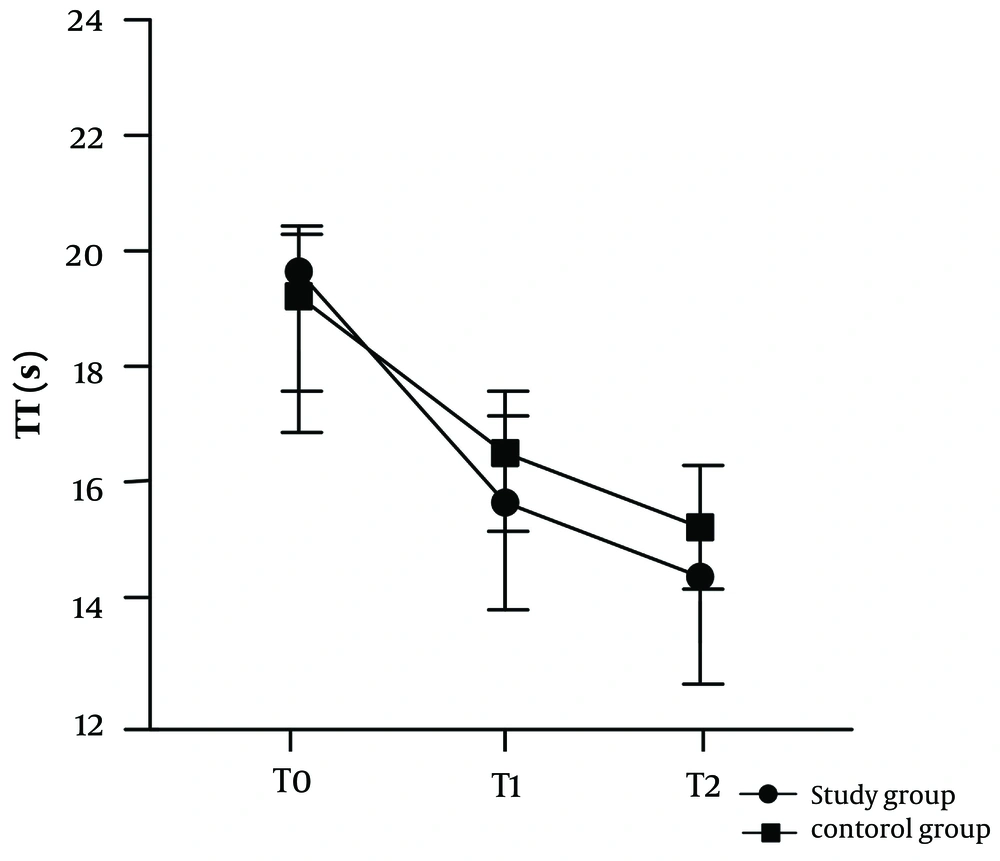
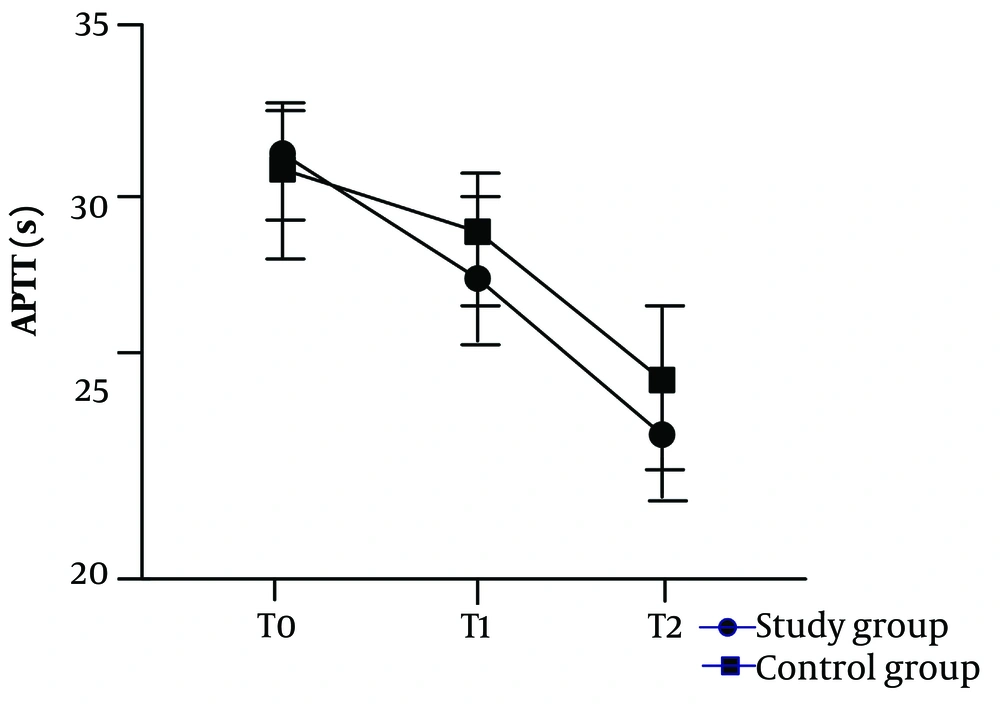
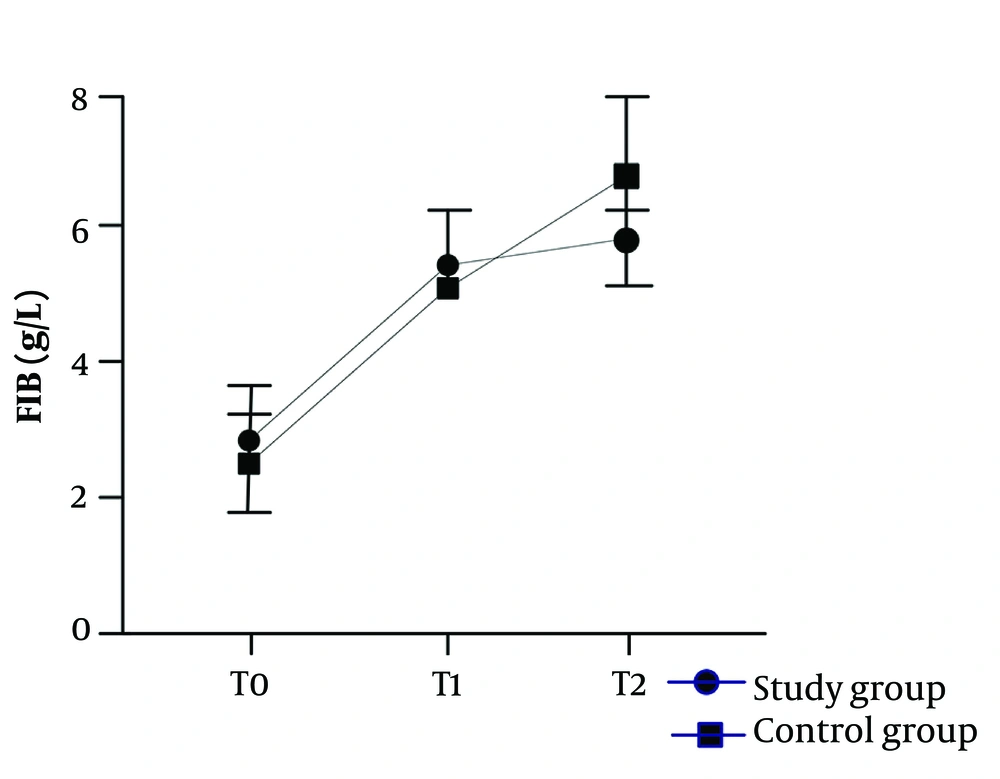
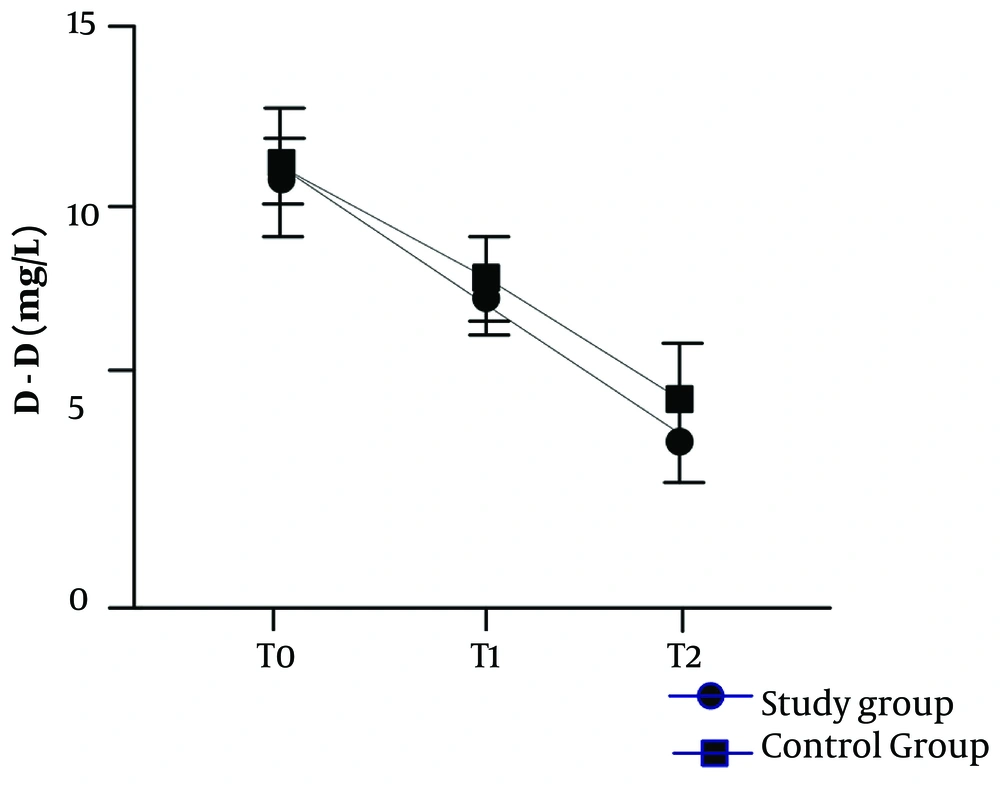
3.4. Comparison of Four Coagulation Indicators Between Two Groups of Patients at Different Time Periods
Overall comparison: There were statistically significant differences in the TT, APTT, FIB, and D-D indicators, as well as in time and interaction among the study group's children (P < 0.05). Please refer to Table 5 and Figures 1 - 4 for details.
| Divisions | No. | T0 | T1 | T2 |
|---|---|---|---|---|
| TT (s) b | ||||
| Study group | 30 | 19.72 ± 2.18 | 15.23 ± 1.41 | 14.22 ± 1.20 |
| Control group | 30 | 19.29 ± 2.51 | 16.01±1.19 | 15.29 ± 1.27 |
| χ2/t | 0.708 | 2.316 | 3.354 | |
| P | 0.482 | 0.024 | 0.001 | |
| APTT (s) c | ||||
| Study group | 30 | 30.71 ± 1.19 | 26.34 ± 1.52 | 23.21 ± 1.28 |
| Control group | 30 | 30.27 ± 2.01 | 27.21 ± 1.09 | 24.65 ± 2.11 |
| χ2/t | 1.054 | 2.548 | 3.310 | |
| P | 0.296 | 0.014 | 0.002 | |
| FIB (g/L) d | ||||
| Study group | 30 | 2.95 ± 0.56 | 5.56 ± 0.40 | 5.09 ± 0.46 |
| Control group | 30 | 2.79 ± 0.41 | 5.35±0.21 | 5.91 ± 1.26 |
| χ2/t | 1.263 | 2.546 | 3.348 | |
| P | 0.212 | 0.014 | 0.001 | |
| D-D (mg/L) e | ||||
| Study group | 30 | 8.26 ± 0.54 | 6.09 ± 0.31 | 4.62 ± 0.69 |
| Control group | 30 | 8.34 ± 1.21 | 6.51 ± 0.94 | 5.49 ± 1.11 |
| χ2/t | 0.331 | 2.324 | 3.646 | |
| P | 0.742 | 0.024 | 0.001 |
Abbreviations: TT, thrombin time; APTT, activated partial thromboplastin time; FIB, fibrinogen; D-D, D-dimer.
aValues are expressed as mean ± SD unless otherwise indicated.
b TT: F division /F intra-group /F interaction = 63.853/388.309/23.147, P division /P intra-group /P interaction = < 0.001/ < 0.001/ < 0.001.
c APTT: F division /F intra-group /F interaction = 32.190/208.896/13.929, P division /P intra-group /P interaction = < 0.001/ < 0.001/ < 0.001.
d FIB: F division /F intra-group /F interaction = 7.561/1932.894/61.723, P division /P intra-group /P interaction = 0.007/ < 0.001/ < 0.001.
e D-D: F division /F intra-group /F interaction = 11.237/954.007/144.597, P division /P intra-group /P interaction = 0.001/ < 0.001/ < 0.001.
3.5. Comparison of Lower Limb Deep Vein Thrombosis Related Symptoms Between Two Groups of Patients
The incidence of lower limb DVT-related symptoms in the study group was significantly lower than in the control group (P < 0.05) (Table 6).
| Divisions | N | Calf PAin | Skin Flushing | Elevated Skin Temperature | Limb Swelling | Limb Stiffness | Total Occurrence Rate |
|---|---|---|---|---|---|---|---|
| Study group | 30 | 1 (3.33) | 1 (3.33) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (6.67) |
| Control group | 30 | 2 (6.67) | 3 (10.00) | 2 (6.67) | 2 (6.67) | 1 (3.33) | 10 (33.33) |
a Values are expressed as No (%).
b χ2 = 5.104; P = 0.024.
4. Discussion
Multivariate logistic regression analysis showed that bed rest time ≥ 3 days (OR = 2.963, 95% CI = 1.282 - 6.852), limb bracing (OR = 2.843, 95% CI = 1.209 - 6.685), FIB (OR = 57.765, 95% CI = 11.308 - 295.094), and D-D (OR = 3.415, 95% CI = 1.396 - 8.359) were independent risk factors for DVT in children with deep vein catheterization. This is due to factors such as prolonged bed rest and reduced limb mobility in critically ill patients with catheterization, causing the blood to lose its "venous pump" function, leading to venous blood stasis or reduced blood flow velocity. Additionally, it results in slower venous blood flow, increased venous obstruction, and blood stasis (11). Furthermore, decreased activity during long-term bed rest and increased consumption of autologous muscle fat can reduce muscle elasticity, increase compression on venous vessels, slow down venous flow velocity, and increase the risk of DVT (12). The study by Broderick C (13) is consistent with the results of this study.
In this study, non-DVT patients were randomly divided into two groups, and corresponding nursing measures were carried out. The results showed that the four coagulation indicators of the study group and the two groups of patients at different time periods were significantly better than those of the control group and the same group before intervention (P < 0.05). This indicates that nursing measures based on DVT risk grading for lower limb crSaO2 testing in children with indwelling catheters can significantly reduce the risk of developing DVT. Research by Yu X et al. has shown that the formation of DVT is mainly due to impaired coagulation function, which is consistent with the results of this study. Based on this, the study analyzed the impact of nursing measures on DVT in children with venous catheterization (14). Activated partial thromboplastin time refers to the time required for blood to coagulate under exogenous pathways, directly reflecting the unique indicator of exogenous coagulation factors. Thromboplastin time indicates the patient's current anticoagulation, coagulation, and fibrinolysis system status. FIB is fibrinogen, the main substance involved in hemostasis, and a decrease in FIB levels can indicate a decline in hemostatic function. Research results show that FIB levels gradually increase from a decreased level after 3 days of catheterization to within the normal range, while APTT and TT gradually shorten and reach normal coagulation time after 7 days. It can be seen that the patient's coagulation function was abnormal 3 days after catheterization, and after receiving different nursing measures, the study group of patients was superior to the control group 14 days after catheterization.
To analyze the mechanism in critically ill children with deep vein catheterization in this article, two points are noted: (1) this induces the production of thrombin, releases adenosine diphosphate (ADP) to induce the production of TT, APTT, and PT, increases blood viscosity and peripheral resistance, and leads to the loss of the vessel wall's original anticoagulant effect (15); (2) during blood clot formation, FIB in the plasma is converted into fibrin monomers under the action of thrombin, causing numerous fibrin monomers to aggregate. However, due to the involvement of XIIIa in this polymerization, it is not firm and cross-links with adjacent proteins to form cross-linked fibrin, resulting in numerous blood cells forming thrombi in the network. The formation of thrombus is unrelated to the imbalance of coagulation and fibrinolysis systems. The increase in FIB can enhance fibrinolytic activity, indirectly increasing FIB and D-D levels. D-dimer is a sensitive indicator of thrombosis, and the passive activation of fibrinolysis can cleave long chains of fibrin, forming various fragments. The simplest segment represents D-D, where excessive D-D accumulates in the vascular wall and directly damages the vascular endothelium, indicating that the patient is in a hypercoagulable state and increasing the risk of DVT (16).
Nursing measures are more targeted under the guidance of NIRS technology, which allows for continuous monitoring of tissue perfusion. This technology fully considers the diversity of human tissue morphology, utilizing light sources and detectors in close contact with the skin and adopting the commonly used Bolton in biological tissues with particularly low water absorption. The probe drives the light source to collect and transmit data on demand through the circuit function, fully reflecting the hemodynamic parameters and the concentration of free radicals in arterioles, capillaries, and arterioles. It also measures the actual value of crSaO2 in the lower limbs after tube placement. Using a benchmark of > 60%, an upward fluctuation of 10% is considered risk-free, while every downward fluctuation of 10% increases the risk level by one.
For risk-free children, basic care is provided, while for other risk levels, personalized, differentiated nursing plans are developed through interdisciplinary team collaboration. Low-risk children are evaluated for issues such as compression or posture. For moderate risk, consider whether hypothermia occurs and implement temperature protection measures. The dietitian and the rehabilitation teacher should specify personalized nutritional support and passive limb movement programs according to the age of the children. If the risk is high, anticoagulant treatment should be given, and after 2 days, the risk level will be re-evaluated. For children still at high risk, consider whether to remove the indwelling catheter, and implement corresponding plans for those who descend to high risk (17).
Passive exercise with different lower limb crSaO2 values can stimulate sympathetic nervous system excitation, downregulate inflammatory factor expression, promote endothelial function recovery, activate coagulation indicators such as TT, APTT, and PT, enhance limb aerobic metabolism, and promote blood circulation. The individualized plan by the dietitian ensures that nutrients in the food are quickly absorbed, increasing body mass and immune function, inhibiting or weakening inflammatory factors, and reducing the inflammatory reaction caused by mechanical injury after catheterization. Furthermore, it can prevent the risk of DVT occurrence (18) and reduce the incidence of DVT-related symptoms such as leg pain, skin redness, elevated skin temperature, limb swelling, and limb stiffness in children after catheterization.
In summary, a multidisciplinary team collaboration based on NIRS technology to develop intervention plans for assessing DVT risk through lower limb crSaO2 detection in children with indwelling catheters can improve coagulation function, increase limb oxygen saturation, and prevent the incidence of DVT-related symptoms, making it worthy of widespread clinical promotion. Additionally, nursing measures based on this approach can be implemented at different levels of care depending on the child's current risk of DVT. Compared with traditional nursing models, this model avoids the disadvantage of a one-size-fits-all approach and fully reflects a child-centered focus, implementing practical nursing measures aligned with the child's actual situation. This model distinguishes primary and secondary nursing services from key points, making nursing measures more specific and personalized, fully meeting the nursing needs of children in the rehabilitation process with stronger purpose and pertinence. It also conforms to the nursing grading guidelines recommended by the Health Commission.
4.1. Conclusions
Real-time monitoring of lower limb oxygen saturation in children with indwelling catheters using NIRS can effectively assess the risk of DVT. Changes in blood oxygen saturation may become an important indicator for predicting DVT, thus enabling timely and effective nursing interventions. This monitoring method is non-invasive, reducing the pain experienced by children, and can continuously and in real-time monitor lower limb blood oxygen saturation. It provides strong evidence for the prevention and treatment of DVT. Therefore, it is recommended to widely apply this monitoring method in clinical practice to improve the nursing effectiveness for pediatric patients and reduce the incidence of DVT.