1. Background
The orogastric tube (OG) plays a pivotal role in neonatal care, facilitating enteral nutrition, medication administration, and alleviation of abdominal distension in the neonatal intensive care unit (NICU) (1). Given the physiological inability of premature and ventilated infants who are unable to suckle and swallow properly, the OG tube has emerged as a crucial medical apparatus in their care (2, 3). If the insertion of the gastric tube tip is too short, leading to positioning in the esophageal or gastroesophageal junction, it can result in ineffective feeding, an increased risk of aspiration, infant discomfort, inaccurate medication administration, and potential gastric complications (4, 5). Conversely, if the tip is inserted too deep, the tube may coil inside the stomach or even advance into the intestine or near the pylorus, leading to poor weight gain, malabsorption, and diarrhea (6, 7).
Radiological examination is the gold standard for confirming the correct positioning of a gastric tube tip within the stomach. While radiography remains an accurate method for verifying tube placement, its selective use is advised due to the potential long-term risks associated with cumulative ionizing radiation exposure, especially in preterm newborns (3, 8). As concerns about the potential long-term harm caused by cumulative exposure to ionizing radiation have increased, ultrasonography has emerged as a preferred method for determining the position of medical devices such as feeding tubes, central venous catheters, and umbilical catheters in infants (9, 10). Previous studies have explored ultrasound as a potential replacement for radiological methods but reported accuracy varies, necessitating further investigation to establish ultrasound's efficacy in confirming gastric tube position (3, 11, 12).
2. Objectives
To address this gap, we conducted an observational study in a Chinese NICU, aiming to assess the accuracy of bedside ultrasonography in verifying OG tube placement.
3. Methods
3.1. Study Design
This was a single-center observational study involving Chinese newborns that was conducted at a children’s hospital in Guangdong Province, China, from October 17, 2021, to May 28, 2022. The inclusion criteria were as follows: (1) Newborns had a gestational age exceeding 28 weeks and a birth weight over 1 000 g, thereby minimizing potential complications associated with additional bedside ultrasound checks; (2) had no gastrointestinal system surgery and did not have malformations; (3) had stable vital signs, initiated feeding, confirmed by the attending neonatologist, and a documented need for OG tube insertion; The exclusion criteria: (1) Newborns for whom medical decisions advocating minimal manipulation; and (2) radiologic assessments were not conducted for other medical issues.
3.2. Sample Size
Kappa statistics were employed to assess the agreement between radiography and ultrasonography in verifying the position of an OG tube. The null hypothesis assumed a κ value of 0.20, while the alternative hypothesis proposed a κ value of 0.45. Sample size calculation was performed using PASS 2021 software (v21.0.3) to test the agreement between two raters, aiming for a statistical power of 90% and a two-sided alpha level of 5%. Based on this calculation, a sample size of 126 individuals was determined.
3.3. Orogastric Tube Insertion
The OG insertion procedure was performed by registered nurses in the NICU who had at least one year of clinical experience in neonatal care. Prior to the study, these nurses received comprehensive training from the lead researchers on the insertion procedure itself, with the aim of minimizing potential biases and complications. To ensure the safe and effective insertion of the OG tube, a pediatric disposable stomach tube kit from VERACON was used, and length was calculated using the weight-based equation of length (kg) +12 cm (13). After insertion, a pH test using strips from DFph0-14 (GZJZ, China) was conducted. A pH reading of 5.5 or below within 10 - 15 seconds confirms tube placement in the stomach (14).
3.4. Radiological Assessment
In our study, the placement of OG was verified through radiographic analysis, which was conducted for other clinical indications. To ensure accuracy and objectivity, expert radiologists with specialized knowledge in neonatal radiology meticulously reviewed each image to determine the exact anatomical location of the gastric tube. The radiologist remained blinded to the essential patient information, as well as the results from the gastric content pH test and ultrasound examination. The median duration from OG tube insertion to radiographically verified positioning was 3.7 hours. In the primary analysis, the radiologist evaluated each radiological image to identify the location of the tube's tip, including the esophagus, gastroesophageal junction, gastric body, or pylorus.
In the secondary analysis, we introduced the concept of an accurate position for the tube in the X-ray examination. This procedure involved ensuring that the tube was not looped back within the stomach and had penetrated more than 2 cm but less than 5 cm into the stomach, referred to as the tenth thoracic vertebra (T10) in the plain radiograph (2, 11, 15). In this study, the neonatal physician, who served as the first author, measured the distance between the tip of the feeding tube and T10 on the image.
3.5. Ultrasound Examination
In this study, a neonatal physician with prior experience in ultrasound techniques for clinical purposes such as lung ultrasound and peripherally inserted central catheter (PICC) placement received specialized training in esophageal and gastric ultrasound at the sonography department over a period of one month. The physician utilized an Esaote ultrasonic diagnostic apparatus and a linear array probe set at a frequency of 10 - 14 MHz to carry out abdominal ultrasonography procedures before administering feedings (16).
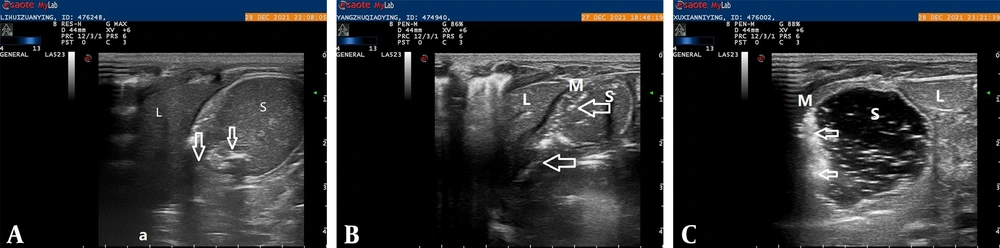
The procedure involved three distinct steps. In the first step, the infants were placed in the supine position, and the mid-epigastric area was scanned by the transducer to visualize two parallel hyperechogenic lines in the stomach (Figure 1A). If there was any uncertainty regarding the tube's tip position, a repeated check was conducted during a feeding, and the milk that flowed into the stomach was observed to ascertain the correct placement of the tip (Figure 1B). In the second step, the physician visualized the tip of the tube adherent to the stomach wall (Figure 1C). Finally, in the third step, the transducer was positioned in the upper right quadrant toward the duodenum to determine whether the OG tube reached the pylorus. By following this multi-step protocol, the physician could accurately determine the location of the feeding tube and ensure correct placement in the stomach (12).
The results of the ultrasound examination performed in this study. Specifically, A shows a coronal oblique sonogram demonstrating the OG tube (indicated by arrows) within the stomach (S). The liver (L) was visible on the sonogram. In B, a sonogram shows milk (M) flowing from the OG tube (also indicated by arrows) into the stomach (S). Finally, C shows that the tube had adhered to the wall of the stomach.
A definition of an accurate position of the tube on ultrasound involved visualizing the tip of the tube within the stomach and confirming that it was not attached to the wall.
3.6. Pilot Study
The pilot study sought to evaluate the viability of ultrasound as a method for OG tube placement in newborns. Employing a prospective observational approach, participants meeting predetermined criteria were recruited. Ultrasound assessments, administered by trained NICU physicians, typically lasted between 10 to 20 minutes. In instances of complexity, confirmation of OG tube placement was facilitated by a sonographer.
3.7. Blinding
To ensure impartiality and mitigate potential bias in the assessment of gastric tube placement, our study incorporated a blinding method. The neonatologist responsible for determining tube placement via ultrasound remained unaware of the radiology results, maintaining a strict blinding protocol. Additionally, the blinding extended to the radiologist, who remained unaware of essential patient information, as well as the results obtained from the gastric content pH test and ultrasound examination. This blinding approach aimed to enhance objectivity and reliability in evaluating the effectiveness of ultrasound and radiology for gastric tube placement.
3.8. Data Collection
To facilitate research, the study team collected data from medical records for each newborn participant, including their sex, gestational age, birth weight, and days of life. The principal authors of the study measured the distance between various anatomical landmarks on radiological images. Additionally, the newborns were weighed on the same baby weighing scale before tube insertion to ensure consistency. Finally, the insertion depth was calculated in centimeters, incorporating all relevant factors that may affect tube placement.
3.9. Statistical Analyses
In this study, data analysis was performed using SPSS Statistics for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables were presented as either the mean ± standard deviation, and categorical data was expressed as frequency and percentage values. Furthermore, the Kappa statistic was used to evaluate the level of agreement between results obtained via radiology and ultrasonography. Radiology verification was considered the gold standard, and sensitivity referred to the accurate detection of tube placement by both radiology and ultrasonography. Specificity was defined as the inaccurate detection by both methods. The false positive was defined as the detection of accurate placement by ultrasonography but incorrect placement by radiology. The false negative was defined as inaccurate placement by ultrasonography, but accurate placement was detected by radiology.
4. Results
4.1. Sample Characteristics
In this study, 159 newborns initially met the eligibility criteria. However, three infants were excluded due to a lack of parental consent, resulting in a final sample size of 156 infants for analysis. Among the analyzed participants, the majority (n = 86; 55.1%) were classified as late preterm or term infants with a gestational age of more than 34 weeks. The average birth weight was 2 200.8 ± 757 g, and the average weight at the time of OG tube placement was 22 265.8 ± 750.3 g. Of the total participants, 101 were male (64.7%). The median age at tube insertion was 1 day after birth, and the median length of the inserted tube was 20.0 ± 2.3 cm.
4.2. Anatomical Position Assessment
In the radiological assessment, gastric tubes predominantly occupied the stomach, constituting 85.3% (133 patients). Concurrently, ultrasound analysis confirmed accurate stomach placement in 88.5% (138 infants). Further precision analysis revealed accuracy rates of 67.3% for radiology and 60.3% for ultrasonography. The overall kappa value, calculated at 0.14 (P = 0.049), is detailed in Table 1.
| Placement | Radiology (N = 156) | Ultrasonography (N = 156) | Kappa | P-Value |
|---|---|---|---|---|
| Anatomical location | 0.28 | 0.001 | ||
| Stomach | 133 (85.3) | 138 (88.5) | ||
| Esophagus | 3 (1.9) | 2 (1.3) | ||
| GE junction | 1 (0.6) | 1 (0.6) | ||
| Duodenum | 19 (12.2) | 5 (3.2) | ||
| Uncertainty | 0 (0) | 10 (6.4) | ||
| Accurate position | 0.14 | 0.049 | ||
| Yes | 105(67.3) a | 94 (60.3) b | ||
| No | 51 (32.7) | 52 (33.3) | ||
| Uncertainty | 0 | 10 (6.4) |
a In an accurate position on radiological images, the tip of the tube should not form a loop within the stomach. Additionally, the tip should be placed from 2 cm to 5 cm from the 10th thoracic vertebra (T10).
b In a precise ultrasound position, the tube's tip should not adhere to the stomach wall, and there should be no loop back into the stomach.
4.3. Agreement Assessment
In the agreement assessment, excluding 10 patients without ultrasound confirmation, sensitivity and specificity stood at 68.6% and 46.3%, respectively. Among false-negative cases, 30 patients had tubes attached to the inner stomach wall, undetected by radiology, and 3 patients had tubes in the duodenum, unconfirmed via radiological assessment. In false-positive instances, 17 patients had tubes inserted too short and 5 patients too deep on radiological images, escaping ultrasound detection. Additional details are outlined in Table 2.
| Ultrasound | Radiology | ||
|---|---|---|---|
| Correct | Incorrect | Total | |
| Correct | Sen:72 (68.6) | FP:22 (53.7) | 94 |
| Incorrect | FN:33 (31.4) | Spe:19 (46.3) | 52 |
| Total | 105 | 41 | 146 |
Abbreviations: Sen, sensitivity; Spe, specificity; FN, false negative; FP, false positive.
5. Discussion
This study aimed to evaluate the precision of ultrasonography in confirming the placement of OG tubes in Chinese newborns, comparing its efficacy with that of radiological methods. Among the 156 newborns with OG tubes, radiology successfully identified 85.3% of tubes positioned in the stomach, while ultrasonography confirmed 88.5%. In terms of accuracy, rates were 67.3% for radiology and 60.3% for ultrasonography. These results highlight the compelling potential of ultrasonography in accurately determining the correct placement of OG tubes.
Previous studies have investigated the diagnostic accuracy of ultrasonography for verifying gastric tube placement, and the overall agreement was moderate, suggesting that ultrasonography is a promising method for determining OG tube placement in this population. In 2018, a study was conducted to assess the diagnostic accuracy of ultrasonography for verifying gastric tube placement, and the results were compared to those of radiological imaging, which is the gold standard. The results showed that ultrasonography had a good sensitivity (0.98) and positive predictive value (0.99), indicating its potential usefulness in identifying the position of OG tubes in infants. However, the specificity of ultrasonography was not evaluated in this study, which limits the generalizability of the findings (16). Another study reported that ultrasonography had a sensitivity of 92.2% for correctly identifying the location of OG tubes. However, the tube position of four neonates (7.8%) could not verified by bedside ultrasound. The authors concluded that while ultrasonography had good sensitivity, it lacked specificity and predictive value (3). Furthermore, a meta-analysis of four articles published in 2002 estimated the sensitivity of ultrasonography for determining OG tube placement to be between 88% and 100%, with only one study reporting a positive predictive value of 99%. However, these studies had small sample sizes, and none of them reported the specificity values for ultrasonography (17).
Previous studies have reported good sensitivity for ultrasonography in verifying OG tube placement, but there is a lack of specificity and inconsistent results across studies. In this study, the lower specificity of ultrasonography indicates that it may not be a reliable tool for verifying placement when the tube insertion length is too short. One of the major reasons is that ultrasonography has difficulty accurately differentiating the anatomical location when the tube has been placed within the stomach. This information can be easily confirmed by radiological images, which offer a more accurate and detailed view of the internal anatomy.
As previously noted, ultrasonography also has other limitations and challenges that must be considered. One major limitation is its dependence on operator skill and expertise, which can affect the accuracy and consistency of results (16). Another challenge is the potential for image interpretation bias, which can be influenced by factors such as patient positioning, probe orientation, and fluid content in the stomach. These factors can lead to false positive or false negative results, which can have serious implications for patient safety (3, 16).
Despite these limitations, ultrasonography has several advantages over radiological assessment for determining OG tube placement, including the ability to identify the location of tube attachment to the stomach wall, which can be a challenging task using radiology. In our study, the individuals with accurate tube placement, as confirmed by radiology, were misclassified as having inaccurate placement on ultrasound due to the difficulty in visualizing tube attachment to the stomach wall. This highlights the importance of operator expertise and standardized protocols in optimizing the accuracy and reliability of ultrasonography for verifying OG tube placement. Despite these limitations, ultrasonography remains a promising tool for noninvasive and real-time monitoring of OG tube placement in neonates and other patient populations, helping clinicians ensure safe and effective nutritional delivery.
5.1. Limitation
Our study has several limitations that should be acknowledged. First, due to safety considerations, we imposed a 15-minute time limit on ultrasound examinations, potentially affecting our ability to confirm the placement of tubes inserted for longer durations or in critically ill neonates. Second, double-check assessments were not conducted for every ultrasound image due to a shortage of trained personnel in our NICU. To mitigate operator bias, the neonatologist underwent additional training in sonography within the ultrasound department. During the pilot study, both the sonographer and neonatologist performed double checks in each case to minimize bias.
5.2. Conclusions
In conclusion, our exploration of ultrasonography for assessing OG tube placement in Chinese newborns indicated potential accuracy rates for both radiology and ultrasonography (67.3% and 60.3%, respectively). However, ultrasonography exhibits constraints in detecting tubes attached to the stomach's inner wall and identifying short insertions, leading to a sensitivity of 68.6% and specificity of 46.3%. Despite these limitations, ultrasonography presents benefits such as non-radiation imaging and bedside monitoring.