1. Background
Burn injuries are among the most common traumas encountered in clinical settings, with children, particularly those aged 1 to 4 years (1), being highly susceptible due to their young age, lack of maturity, and active nature. Between 2000 and 2018, it's estimated that around 203 180 children under the age of 20 in the US were treated for facial burns, averaging approximately 10 694 cases annually, or 130 burns per million children (2). Common causes include scalds from boiling or hot liquids, with less frequent incidents involving flames, explosions, or chemical burns (3). The young and delicate nature of a child's skin, combined with their organism's overall immaturity, results in a decreased tolerance for burns and pain. This increases the likelihood of severe complications such as sepsis and shock, potentially jeopardizing the child's life and health, even in milder cases (4). Moreover, burn healing processes can disrupt the normal structure of collagen and elastic fibers, leading to scarring that may impair wound healing and cause significant physical and emotional distress due to scarring and limb contracture (5).
Current clinical treatments primarily involve conventional debridement, dressing changes, and skin grafting to encourage the growth of granulation tissue and wound healing. However, the extended healing time and the pain associated with dressing changes often result in low treatment compliance and suboptimal healing outcomes (6). While existing literature has explored pain management and scar management for children during burn wound healing, there remains an incomplete understanding of factors influencing healing speed and quality (7, 8). Particularly for children with second-degree burns, these influencing factors could be more complex due to their body tissues' differing regeneration and recovery capabilities compared to adults. Despite mentions of age, burn size, and depth as potential prognostic factors for hospitalized burn patients, comprehensive studies focusing on the healing of second-degree burns are scarce, offering limited benefits for affected children (9).
2. Objectives
This study undertook a retrospective analysis of 87 children with second-degree burns treated in our hospital's burn surgery department from January 2020 to December 2022. The objective was to investigate the factors impacting wound healing in this specific patient group, aiming to provide insights for improving their prognosis.
3. Methods
3.1. Research Subjects
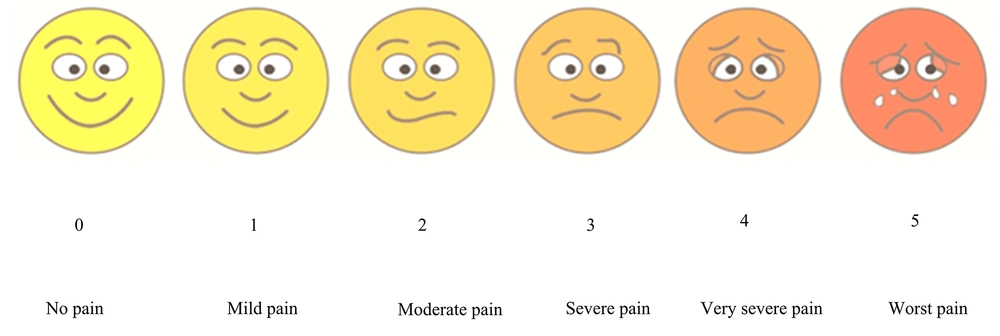
This study employed a retrospective analysis. Children diagnosed with second-degree burns at our burn surgery department from January 2020 to December 2022 were selected. Their general information was obtained and screened through the hospital's medical record system and outpatient follow-up records. The inclusion criteria were as follows: (1) the injuries were burn-induced and classified as second-degree burns, including both superficial and deep second-degree burns (10); (2) the age range was 1 - 13 years; and (3) the patients were admitted for treatment within 2 days post-injury. Exclusion criteria included: (1) significant organ dysfunction such as heart or lung issues; (2) immune or coagulation disorders; (3) complications from sepsis or shock; and (4) patients with incomplete primary clinical data. The study received approval from the hospital's medical ethics committee (Figure 1).
For sample size determination, we adhered to the events per variable (EPV) (11) principle, requiring that the number of events in the dependent variable be at least ten times the number of independent variables in the model. Based on previous findings indicating a 25% probability of poor wound healing in burned children, the study aimed to include five influencing factors with an EPV of 10, necessitating a minimum of 200 participants. To account for a potential 10% dropout rate, the target recruitment was set at 220 individuals.
3.2. Research Methodology
In this retrospective study, data was systematically collected. Information on each child's gender, age, and body mass index (BMI) was obtained from electronic medical records and through demographic questionnaires. Detailed information on the burn incident, including the cause, admission method, wound medication usage, dressing type, wound area, and location, was recorded to comprehensively understand the burn context. Signs of wound infection were closely monitored, and the time, symptoms, and infection degree were meticulously documented. Adherence to diagnostic criteria was ensured for accurate infection diagnosis, with confirmation from senior medical personnel. Dressing change frequency, extent, and compliance scores were noted, providing valuable insights into the therapeutic and rehabilitation progress of patients. Additionally, family burn care knowledge levels were assessed through questionnaires, offering practical implications for enhancing home care quality and preventing complications.
To accurately assess wound infections, medical personnel monitored for symptoms such as swelling, pain, increased secretions, and elevated body temperature. Then, samples of wound secretions were collected from the children for laboratory tests. The samples were analyzed by professional inspectors in the microbiology laboratory, where they underwent Gram staining, smear tests, and quantitative assessments to evaluate their characteristics. Bacterial identification was performed using the VITEK 2 Compact automatic microbial analyzer. A positive result indicated a wound infection, whereas a negative result indicated no infection.
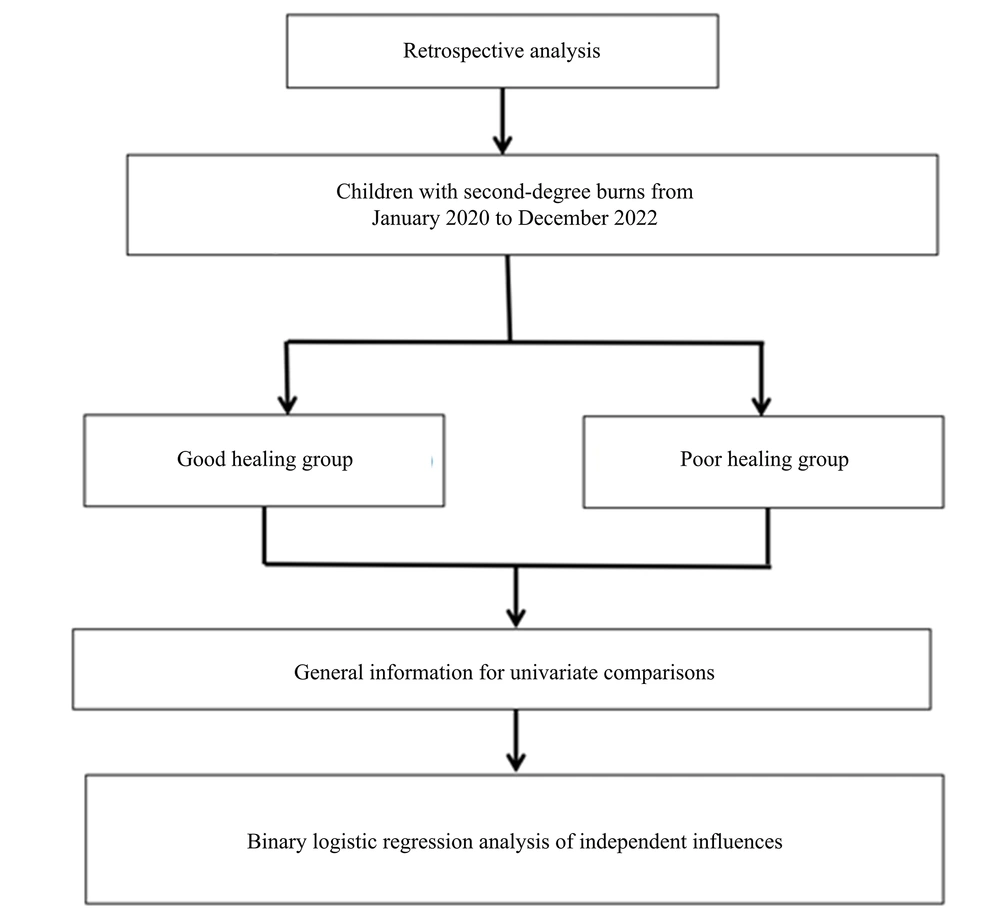
Pain in children was assessed using the Wong-Baker FACES Pain Rating Scale, which features six facial expressions corresponding to scores from 0 to 5, ranging from a smile (no pain) to tears (severe pain) (12). Before the assessment, children were instructed on how to interpret each facial expression in terms of pain levels and choose the one that best represented their own pain. Cross-assessor reliability was ensured by involving three experienced physicians from other departments who were trained in using the scale. To maintain consistency in evaluations, these evaluators discussed and consulted with each other as needed to ensure the reliability of the assessment outcomes (Figure 2).
The compliance of children with dressing changes was evaluated using a questionnaire designed by our hospital. This questionnaire was distributed to the children’s family members by nursing staff on the day before discharge. It consisted of 25 items covering four categories: Nursing emotions, behavioral expressions, skin reactions, and the dressing change process, with each item scoring up to 4 points for a total of 100 points. Similarly, the burn nursing knowledge of family members was assessed through a self-created questionnaire distributed by nursing staff the day before discharge. This questionnaire comprised 25 items on common issues faced by burn patients and their parents' coping strategies, with each item worth 4 points for a total score of 100 points.
To ensure the accuracy and reliability of the children’s dressing change compliance score and the family’s burn nursing knowledge score, we verified the reliability and validity of the questionnaire. Reliability was evaluated using Cronbach's alpha coefficient and the test-retest method. The internal consistency was determined by calculating Cronbach's alpha, while the test-retest method involved administering the questionnaire to the same group at two different times to assess its stability. Cronbach's alpha coefficients for the questionnaires were 0.812 and 0.824, respectively. For validity, we assessed content, construct, and confirmatory validity. Content validity was reviewed and revised by experts in the field. Construct validity was examined through factor analysis, among other methods. Confirmatory validity required comparison with similar, validated questionnaires. The validity tests showed that both questionnaires have practical application.
Blood routine data were gathered via the hospital's medical record system at the first examination upon admission. Selected indicators for commonly elevated values in children with second-degree burns included white blood cell count (WBC), neutrophil (NEUT) count, neutrophil ratio (NR), and hemoglobin (HGB). Data compilation was conducted by one researcher and verified by two others.
3.3. Evaluation Criteria for Wound Healing
(1) The trauma area for children in both groups was measured at 14 and 21 days after admission using transparent paper tracing and a computer-aided imaging system. The healing rate was calculated based on complete epithelialization of the trauma (13): Healing rate = (total trauma area - unhealed trauma area)/total trauma area × 100%. A healing rate above 70% scored 0, and below 70% scored 1.
(2) Scar formation on the trauma surface was scored using the Vancouver Scar Scale (VSS) (14) after 14 days of treatment, with scores up to 7. A lower score indicated better scar formation.
(3) Wound healing quality was evaluated based on healing rate and scar formation post-treatment. The cumulative score of healing rate and scar formation defined the healing quality: A total score of < 3 was considered good healing, and ≥ 3 was poor healing.
3.4. Analysis of Influencing Factors
All patients were categorized into a good healing group and a poor healing group based on the condition of their wounds. Data from both groups were compared to analyze factors influencing wound healing in children with second-degree burns.
3.5. Statistical Methods
The statistical analysis was conducted using SPSS 27.0 software, employing both univariate and logistic regression analyses to compare and analyze the data. Univariate analysis was used to compare general data between children with good and poor healing outcomes. Continuous variables such as age and BMI score were compared using the t-test, while categorical variables like gender and the cause of burn were analyzed using the chi-squared (χ2) test.
A binary logistic regression model was applied to examine factors affecting healing, using independent variables that may influence healing and the dependent variable of healing quality (good or poor). The Hosmer-Lemeshow test assessed the model's fit, and the impact of independent variables on the dependent variable was expressed through the odds ratio (OR) and 95% confidence interval (95%CI). A P-value of < 0.05 was considered statistically significant.
4. Results
4.1. Wound Healing in Children with Second-Degree Burns
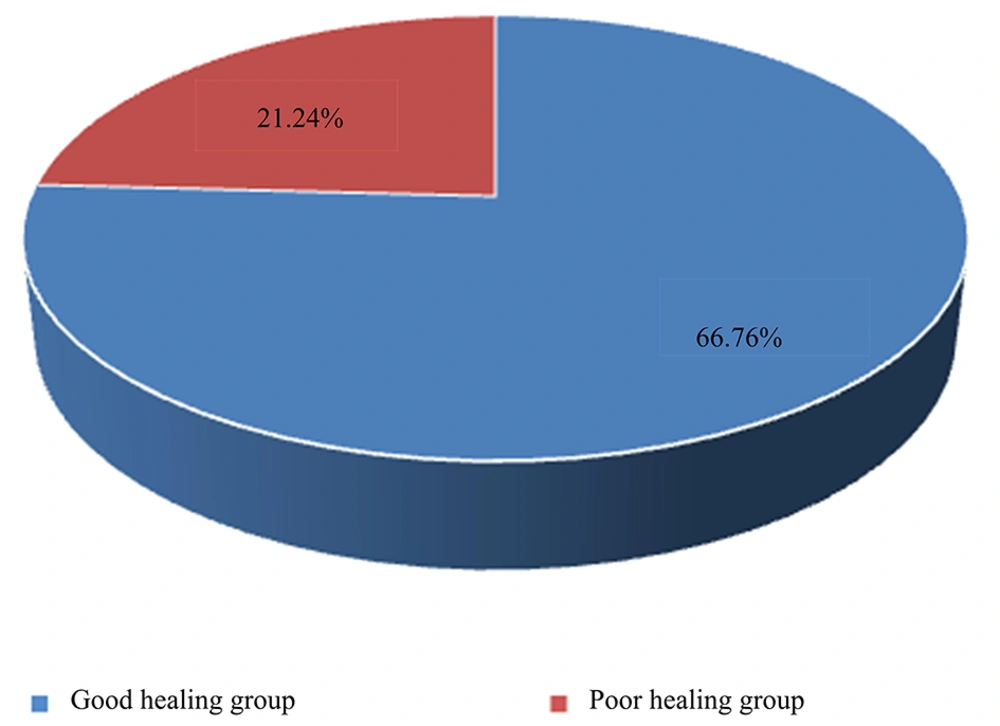
Out of the 220 children admitted to the hospital, 166 cases (75.46%) were observed to have good healing, and 54 cases (24.54%) had poor healing. Accordingly, 166 children were included in the good healing group and 54 children in the poor healing group (Figure 3).
4.2. Analysis of Single Factors Affecting Trauma Healing in Children with Second-Degree Burns
Basic clinical data from the good healing group and the poor healing group were compared for single-factor analysis. The results indicated that therapy methods (surgery or drugs), dressing type (new breathable sterile dressing or traditional oil sand dressing), burn area, number of dressing changes, children's medication change compliance score, WBC, NEUT, and NR were statistically significant (P < 0.05). Other factors did not show statistical significance (P > 0.05), as shown in Table 1.
| Factors | Good Healing Group (n = 166) | Poor Healing Group (n = 54) | Statistics | P-Value |
|---|---|---|---|---|
| Gender | χ2 = 1.124 | 0.267 | ||
| Male | 115 (69.28) | 33 (61.11) | ||
| Female | 51 (30.72) | 21 (38.89) | ||
| Age (y) | 4.89 ± 2.79 | 4.48 ± 2.72 | t = 0.965 | 0.336 |
| BMI (kg/m2) | 21.22 ± 3.25 | 21.39 ± 3.20 | t = -0.347 | 0.729 |
| Burn cause | χ2 = 1.099 | 0.777 | ||
| Scald | 131 (78.91) | 39 (72.22) | ||
| Electrical burn | 16 (9.64) | 7 (12.96) | ||
| Fire wound | 11 (6.63) | 5 (9.26) | ||
| Chemical burn | 8 (4.82) | 3 (5.56) | ||
| Therapy method | χ2 = 5.518 | 0.019 | ||
| Surgery | 101 (60.84) | 23 (42.59) | ||
| Drugs | 65 (39.16) | 31 (57.41) | ||
| Dressing type | χ2 = 6.613 | 0.010 | ||
| New breathable sterile dressing | 123 (74.10) | 30 (55.56) | ||
| Traditional oil and sand dressing | 43 (25.90) | 24 (44.44) | ||
| Burn area (cm2) | 16.47 ± 4.46 | 21.04 ± 5.55 | t = -6.138 | < 0.001 |
| Wound infection | χ2 = 2.404 | 0.121 | ||
| Negative | 120 (77.29) | 33 (61.11) | ||
| Positive | 46 (22.71) | 21 (38.89) | ||
| White blood cell (× 109/L) | 17.32 ± 5.38 | 21.88 ± 8.39 | t = -4.654 | < 0.001 |
| Neutrophil (× 109/L) | 18.16 ± 7.31 | 22.47 ± 6.74 | t = -3.831 | < 0.001 |
| Neutrophil ratio (%) | 72.48 ± 10.16 | 74.14 ± 11.53 | t = -1.011 | 0.026 |
| HGB (g/L) | 161.97 ± 13.58 | 165.46 ± 11.67 | t = -1.697 | 0.135 |
| The degree of pain | 2.88 ± 1.21 | 3.09 ± 1.15 | t = -1.115 | 0.266 |
| Number of drug changes | 2.82 ± 1.60 | 4.11 ± 1.11 | t = -5.501 | < 0.001 |
| Child's medication change compliance score | 85.66 ± 12.67 | 81.35 ± 12.60 | t = 2.175 | 0.031 |
| Family member burn care knowledge score | 83.28 ± 8.28 | 81.19 ± 10.24 | t = 1.518 | 0.130 |
a Values are expressed as No. (%) unless otherwise indicated.
4.3. Analysis of Multiple Factors Affecting Trauma Healing in Children with Second-Degree Burns
Binary logistic regression analysis was utilized to explore the factors influencing wound healing in children with second-degree burns. The dependent variable was categorized into two groups: The good healing group and the poor healing group. The independent variables included were those statistically significant factors listed in Table 1, namely therapy methods (surgery or drugs), dressing type (new breathable sterile dressing or traditional oil sand dressing), burn area, number of dressing changes, children's medication change compliance score, WBC, NEUT, and NR, totaling eight factors. The specific details of these variables are presented in Table 2.
| Argument | Assignment |
|---|---|
| Therapy method | Surgery = 0, drugs = 1 |
| Dressing type | New breathable sterile dressing = 0, Traditional oil and sand dressing = 1 |
| Burn area (cm2) | The original value |
| Number of drug changes | The original value |
| Child's medication change compliance score | The original value |
| White blood cell (× 109/L) | The original value |
| Neutrophil (× 109/L) | The original value |
| Neutrophil ratio (%) | The original value |
The final regression analysis indicated a good fit of the logistic regression model, as evidenced by the Hosmer-Lemeshow test (χ2 = 9.739, P = 0.28). Among the variables, five were statistically significant: Burn area (OR = 1.217, 95%CI = 1.109 ~ 1.335, P < 0.05), number of medication changes (OR = 1.902, 95%CI = 1.392 ~ 2.599, P < 0.05), WBC (OR = 1.076, 95%CI = 1.008 ~ 1.150, P < 0.05), NEUT (OR = 1.080, 95%CI = 1.018 ~ 1.146, P < 0.05), and NR (OR = 1.040, 95%CI = 1.002 ~ 1.081, P < 0.05). The therapy method, indicated by a β value of 0.737, suggested that surgical intervention might increase the likelihood of good healing (as it is positive) compared to medication alone, though this effect was not statistically significant (P = 0.076), as P > 0.05. Detailed regression analysis results are depicted in Table 3.
| Factors | β-Value | SE | Wald | OR | 95%CI | P-Value |
|---|---|---|---|---|---|---|
| Therapy method | 0.737 | 0.415 | 3.149 | 2.089 | 0.926 ~ 4.713 | 0.076 |
| Dressing type | 0.415 | 0.425 | 0.116 | 1.156 | 0.502 ~ 2.660 | 0.733 |
| Burn area (cm2) | 0.196 | 0.047 | 17.116 | 1.217 | 1.109 ~ 1.335 | < 0.001 |
| Number of drug changes | 0.643 | 0.159 | 16.303 | 1.902 | 1.392 ~ 2.599 | < 0.001 |
| Child's medication change compliance score | -0.019 | 0.016 | 1.394 | 0.982 | 0.952 ~ 1.012 | 0.238 |
| White blood cell | 0.074 | 0.034 | 4.773 | 1.076 | 1.008 ~ 1.150 | 0.029 |
| Neutrophil | 0.077 | 0.030 | 6.429 | 1.080 | 1.018 ~ 1.146 | 0.011 |
| Neutrophil ratio | 0.040 | 0.019 | 4.159 | 1.040 | 1.002 ~ 1.081 | 0.041 |
5. Discussion
Burns are notably common in pediatric accidents. A study conducted in the Enugu area over seven years (June 2011 to May 2018) reported that 56.7% of 198 cases involved thermal fluid burns, while a smaller percentage resulted from flame burns (15). Clinically, second-degree burns are categorized into superficial partial-thickness burns, affecting only the dermis with generally shorter healing times, and deep partial-thickness burns, which damage below the papillary layer of the dermis but spare parts of the reticular layer. The latter are not consistent in-depth and require a longer time for repair (16). Children with second-degree burns face challenges in cooperating with treatment due to their young age, lower immunity, sensitive skin, and inability to avoid injury causes. The severe pain post-scalding and unsightly wounds also contribute to poor healing conditions and extended recovery times. Hence, identifying factors that influence wound healing in children with second-degree burns is crucial. This study aims to expedite wound healing, enhance therapeutic outcomes, and lay a foundation for the clinical application of scientific and efficient nursing interventions.
5.1. Burn Area
In this study, among 220 children with second-degree burns, 166 (75.45%) experienced good wound healing, while 54 (24.55%) had poor wound healing. The patients were categorized into good and poor wound healing groups based on their recovery outcomes. Univariate analysis indicated that the burn area in the poor healing group was significantly larger than in the good healing group. Furthermore, multivariate logistic regression analysis identified the burn area as an independent factor influencing wound healing in children with second-degree burns. The analysis concluded that the larger the burn area, the more challenging the healing process for the children. This finding aligns with Rashid et al.'s team's (17) observations in a postoperative healing study of 217 volunteers undergoing rotator cuff surgery, which also concluded that larger areas of skin or tissue damage negatively impact wound healing. Additionally, Mason et al.'s team (18), through a systematic review of burn injury literature, found that the burn area was a risk factor affecting return to work in burn injury patients. Rashid et al.'s team (17) also highlighted the close relationship between age and wound healing; however, age did not show a statistically significant difference between the two groups in our study. Our study focused on children aged 1 - 13 years, a group generally believed to have superior tissue repair capabilities compared to adults or the elderly, without significant collagen loss (19). Thus, in children with second-degree burns, the extent of the wound area should receive ample attention. It's well-understood that larger wound areas often indicate more severe patient conditions, with burn wounds causing typical local and systemic physiological disruptions that intensify with the wound's size and depth. Minimal systemic changes occur with small total burn areas, but as burns enlarge, complications such as shock and infections become more probable, delaying wound healing (20). This underscores the need for more effective treatments and protective measures for children with extensive burns, vigilance for complications, and recommendations for prolonged hospital stays to improve the condition of children with second-degree burns effectively.
5.2. The Number of Dressing Changes
Multivariate logistic regression analysis identified the number of dressing changes as an independent factor affecting wound healing in children with second-degree burns. This analysis revealed a negative correlation between the number of dressing changes and healing, indicating that dressing changes that are too frequent hinder wound recovery. This finding has yet to be highlighted in other literature. However, most discussions on caring for children with burns emphasize wound protection, highlighting the risks of complications such as bacterial infections due to improper wound care and the adverse effects of frequent medication changes on children's emotional states (21). It's evident that increasing the number of medication changes can also increase the frequency of trauma exposure to external environments and potentially elevate the child's pain, leading to resistance and non-cooperation with treatment. Interestingly, the necessity for dressing changes is influenced by various factors. For instance, Mofazzal et al. (22) found that advanced dressings utilizing nanotechnology not only inhibited microbial growth but also modulated immune responses and expedited wound healing, thereby reducing the need for frequent dressing changes. Similarly, Resch et al. (5) reported favorable outcomes from using an innovative nanocellulose-based dressing on children's burns, which significantly sped up healing and decreased the number of dressing changes required. Malhotra and Kaimal (23) discovered that a new care model focusing on the psychological state of the burned child did not necessitate increased dressing changes. Instead, it alleviated the child's distress and fostered more positive cooperation in family care.
5.3. Blood Routine Index
White blood cell count, NEUT, and NR are identified as risk factors for poor wound healing in children with second-degree burns. The elevated levels of WBC, NEUT, and NR are associated with an increased risk of poor wound healing. A significant pathophysiological response to burn injury is the onset of oxidative stress. Ischemic tissue perfusion following thermal trauma leads to a discrepancy between reactive oxygen species (ROS) and the body's antioxidant defense, resulting in increased vascular permeability and lipid peroxidation of plasma membranes, potentially triggering local or systemic inflammatory responses post-burn (24). White blood cell count, NEUT, and NR serve as crucial indicators of the immune system's reaction. They are instrumental in managing burn infections and facilitating tissue repair, especially neutrophils, which eliminate infections and clear damaged tissues through phagocytosis and the release of inflammatory mediators. However, an exaggerated inflammatory response may cause further tissue damage and delay healing (25). Elevated levels of WBC, NEUT, and NR could indicate ongoing inflammation or infection, which disrupts the natural wound-healing process. Clinical studies suggest that WBC, NEUT, and NR can act as predictors of poor wound healing. For instance, Nie et al. (26) compared the clinical data between children with burns and traumas, noting higher values of RBC, HB, WBC, and AST in the burn group. Yeong et al. (27) analyzed the blood routine data of 73 burn patients within the first 24 hours post-injury and proposed that Hb and WBC could serve as indicators for diagnosing extensive burns, especially in critical cases. Sen et al. (28) examined hematological changes post-burn, observing that severe burns induce dynamic shifts in complete blood count (CBC) within a week after the injury, with WBC considered a critical index for predicting the clinical progression in burn patients. Animal research has demonstrated that NEUT and NR can assess burn severity and guide anti-inflammatory treatments in burned rats (29).
5.4. Other Confounding Factors
The univariate analysis indicated that the method of therapy (surgical or drug), the type of dressing (new breathable sterile dressing or traditional oil-sand dressing), and the child’s medication change compliance score were similar in both the good and poor healing groups, but these results did not achieve significance in the multifactorial analysis. This discrepancy might be attributed to a limited sample size, which could introduce bias. Additionally, a potential correlation between the type of dressing, wound infection, treatment method, and the number of dressing changes, as well as the correlation between the degree of burn, pain, and burn area, might have influenced the results (17, 22). Despite these factors, optimal wound healing treatment and care should prioritize the wound condition, devise reasonable treatment plans based on injury size, and minimize medication changes to ensure safe wound healing.
5.5. Future Prospects
While this study identified factors like burn area, number of dressing changes, white blood cell count, neutrophil count, and neutrophil ratio as influential on wound healing, the precise mechanisms remain to be clarified. Future studies might explore the use of machine learning and artificial intelligence to enhance the accuracy of poor prognosis predictions in children with burns, offering valuable guidance to clinicians. Although our study did not find significant effects of treatment methods and age on wound healing, these avenues merit further investigation. Interdisciplinary collaboration, incorporating insights from physics, material science, and bioengineering, could introduce innovative approaches and breakthroughs in burn treatment, including advancements in burn dressings.
5.6. Limitations
This single-center retrospective study has its limitations, including potential bias inherent in analyzing wound healing rates and scar formation within a singular study population without comparison to other centers.
5.7. Conclusions
Children with second-degree burns demonstrating smaller burn areas, fewer medication changes, and lower levels of white blood cells, neutrophils, and neutrophil ratio exhibit better wound healing. Clinical treatment and post-intervention care plans, informed by these influential factors, can facilitate rapid wound recovery in children with second-degree burns. This study confirms that informed consent was obtained from all participants or their parents/legal guardians for those below the age of consent, in accordance with the Declaration of Helsinki.