1. Background
Intermittent exotropia (IXT) is a common eye misalignment condition in children, with prevalence rates ranging from 0.12% to 3.9% (1, 2). Intermittent exotropia is characterized by an intermittent outward deviation of one or both eyes (3). Fusional vergence plays a crucial role in maintaining binocular functions during exotropia and realignment, including fixation, visual performance, and binocular motility (4). Various surgical and non-surgical treatments can be used to control exodeviation (5).
Surgery is the primary treatment for IXT, aimed at maintaining ocular alignment and preserving binocular vision. Many factors, such as the preoperative deviation angle, control of binocular synergy, stereopsis, and their complex interactions, are essential for predicting surgical success (SS). However, there is limited evidence on widely accepted factors affecting surgical outcomes. Current challenges in IXT treatment include predicting ocular alignment, the potential for postoperative recovery of binocular vision, and the predictability of postoperative outcomes. Fusional vergence maintains binocular vision across a range of vergences. Recent studies have compared the vergence range between IXT patients and normal subjects. Although fusional vergence in IXT has been studied, conclusions remain contradictory (6). Fu et al. reported reduced convergence amplitudes detected by both prism bar and synoptophore in IXT patients (7). Hatt et al. noted a subnormal convergence reserve at distance divergence (8). Sharma et al. found reduced distance fusional divergence and poor fusion vergence amplitudes in IXT patients (9). Additionally, fusional vergence has been reported to recover to normal levels after surgery. To our knowledge, only one report has focused on differences in fusional vergence changes among surgically successful patients. Therefore, it remains unclear how fusional vergence changes in surgical failure (SF) cases and whether fusional vergence is related to the success or failure of surgery.
2. Objectives
This study aimed to evaluate changes in fusional vergence after strabismus surgery and explore the predictive effect of fusional vergence on surgical outcomes.
3. Methods
3.1. Study Design and Patients
This is a cross-sectional study. The project was approved by the Institutional Review Board of Beijing Tongren Hospital, Capital Medical University (TRECKY2014-022), and conforms to the tenets of the declaration of Helsinki. Written informed consent was obtained from the participant or a parent or legal guardian. The study was registered with the Chinese Clinical Trial Registry (ChiCTR-RCC-1800018005). All patients diagnosed with IXT by an experienced pediatric doctor (F.J.) from March 2015 to October 2016 were included. Patients with symptomatic exotropia who underwent strabismus surgery were included in the study.
3.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (a) aged 4 to 18 years; (b) exotropia of 15 prism diopters (pd) or greater; (c) best corrected visual acuity (BCVA) of 6/6 or better in each eye; and (d) basic type IXT [where the angle of exodeviation is the same at distance and near, and less than 10 (pd), or where the distance deviation is within 10 pd of the near deviation].
The exclusion criteria were as follows: (a) amblyopia; (b) history of ocular surgery; (c) insufficient convergence or excessive divergence with IXT (where the angle of exodeviation measures greater than 15 pd at near and distance); and (d) developmental delay or neurologic problems.
3.3. Surgical Procedure
All surgeries were performed by the same experienced pediatric surgeon (F.J., the corresponding author). Subjects aged 14 years and younger underwent surgery under general anesthesia, while those aged 15 years and older were operated on under local anesthesia, unless general anesthesia was specifically required. All patients underwent bilateral rectus recession. The amount of lateral rectus recession was determined based on the maximum angle of exodeviation.
(SS) was defined as having 10 (PD) or less of exotropia or 6 PD or less of esotropia at the 6-month follow-up. Patients meeting the criteria for (SS) were classified as having achieved (SS), while those failing to meet these criteria were classified as SFs.
3.4. Ophthalmologic Examinations
All subjects underwent a complete ophthalmologic examination. The angle of deviation was measured using the prism and alternate cover test (PACT). Refractive conditions were assessed by cycloplegic refraction with 1% cyclopentolate hydrochloride.
3.5. Fusional Vergence Examination
Fusional vergences were measured by experienced orthoptists using the synoptophore L-2510B/L-2510HB (Inami & Co., Ltd., Japan). The position of superposition (where a slide of a lion is aligned with a slide of a cage) was detected and recorded. The breakpoints for fusional divergence and fusional convergence were measured using fusion slides that subtended a visual angle of 6 degrees horizontally and 8 degrees vertically. To ensure consistency, all subjects were examined under uniform test conditions to minimize the effects of fixation target size and examination environment.
The amplitude of fusional divergence was defined as the difference between the superposition and the divergence breakpoint. The fusional amplitude of convergence was defined as the difference between the superposition and the convergence breakpoint. The total fusional vergence amplitude was defined as the difference between the breakpoints for divergence fusion and convergence fusion.
3.6. Stereopsis Detection
The near stereopsis was assessed using a random spots stereo book, while distant stereopsis was evaluated using dissociated pictures on a synoptophore.
3.7. Statistical Analysis
Statistical analysis was performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Independent sample Student’s t-test or Mann-Whitney U test, as appropriate, were used to compare various parameters between the SS group and the (SF) group. Paired t-tests were used to compare preoperative and postoperative parameters within each group. A P-value of < 0.05 was considered statistically significant.
4. Results
4.1. Baseline Demographic
Of the 297 patients who underwent surgery for IXT during the study period, 82 patients met the inclusion criteria, including 41 females and 41 males. The baseline preoperative clinical characteristics are shown in Table 1. The average age at diagnosis was 5.16 ± 2.59 years, and the duration of deviation was 4.12 ± 2.94 years. The average refraction was -0.25 diopters in the right eye and -0.38 diopters in the left eye. Additionally, 10.98% of subjects had a recorded family history.
| Preoperative Characters | Average |
|---|---|
| Age at onset (y) | 5.16 ± 2.59 |
| Duration of deviation (y) | 4.12 ± 2.94 |
| Age at surgery (y) | 9.33 ± 4.01 |
| Refraction (spheric equivalent, diopters) | |
| Right eye | -0.25 (-2.00 - 0.53) |
| Left eye | -0.38 (-1.56 - 0.50) |
| Breakpoint (degrees of arc) | |
| Fusional divergence | -14.46 ± 4.87 |
| Fusional convergence | 3.50 (-2.25 - 9.00) |
| Amplitude (degrees of arc) | |
| Fusional divergence | 6.10 ± 3.85 |
| Fusional convergence | 12.06 ± 6.80 |
| Angle of deviation (prism, diopters) | 36.16 ± 14.19 |
| BMI (kg/m2) | 22.36 ± 6.72 |
| Family history | |
| Yes | 9 (10.98%) |
| No | 73 (89.02%) |
Preoperative Clinical Demographic Characteristics of Intermittent Exotropia a
4.2. Differences of Fusional Vergence Between Surgical Success and Failure Groups
Surgical success was achieved in 62 subjects (75.61%) at the 6-month follow-up. Twenty subjects had residual exodeviation, and no patient developed consecutive esotropia. There were no statistically significant differences in preoperative characteristics between the SS group and the SF group. These characteristics included age at onset (5.14 ± 2.61 vs. 5.21 ± 2.54, P = 0.985), gender (30:32 vs. 10:10, P > 0.05), duration of deviation (4.08 ± 2.92 vs. 4.23 ± 2.99, P = 0.971), age at surgery (9.29 ± 4.06 vs. 9.44 ± 3.85, P = 0.979), the angle of deviation (36.70 ± 14.20 vs. 34.50 ± 14.17, P = 0.913), and near and distance stereopsis (P > 0.05). As shown in Table 2, no significant differences were found in preoperative fusional vergence parameters between the groups.
| Parameters | SS Group; (n = 62) | SF Group; (n = 20) | P-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Before (a) | After (b) | P-Value | Before (c) | After (d) | P-Value | P1 (a vs. c) | P2 (b vs. d) | |
| Breakpoint (degrees of arc) | ||||||||
| Fusional divergence | -14.26 ± 5.03 | -7.52 ± 4.14 | 0.303 | -15.10 ± 4.42 | -10.00 ± 5.96 | 0.496 | 0.505 | 0.040 |
| Fusional convergence | 4.11 ± 8.23 | 10.03 ± 4.36 | 0.526 | 2.40 ± 7.81 | 4.65 ± 7.27 | 0.834 | 0.415 | < 0.001 |
| Amplitude (degrees of arc) | ||||||||
| Fusional divergence | 6.52 ± 4.10 | 6.11 ± 1.96 | 0.928 | 5.00 ± 2.15 | 4.8 ± 1.61 | 0.941 | 0.209 | 0.008 a |
| Fusional convergence | 11.85 ± 6.70 | 11.44 ± 3.43 | 0.957 | 12.60 ± 6.34 | 9.85 ± 4.63 | 0.728 | 0.632 | 0.104 |
Comparisons of Fusional Vergence Parameters Before and After Surgery Between Surgical Success and Surgical Failure Groups
The postoperative fusional vergence breakpoints showed significant changes in both the SS group and the SF group (P < 0.05), with greater changes observed in the SS group compared to the SF group. The postoperative fusional divergence breakpoints were -7.52 ± 4.14 degrees in the SS group and -10.00 ± 5.96 degrees in the SF group (P = 0.040). The postoperative fusion convergence breakpoints were 10.03 ± 4.36 degrees in the SS group and 4.65 ± 7.27 degrees in the SF group (P < 0.001). The amplitude of fusional divergence was higher in the SS group compared to the SF group (P = 0.008). Although the amplitude of fusional convergence was also higher in the SS group, the difference was not statistically significant (P = 0.104).
4.3. Univariate Analysis for Surgical Success
The correlation between fusional vergence and SS was evaluated, revealing a moderate inverse correlation between the breakpoint of fusional divergence and SS (𝑟 = -0.63, P = 0.038). No significant correlation was observed between the breakpoint of fusional convergence (𝑟 = 0.28, P = 0.120) or the amplitude of fusional convergence (𝑟 = 0.08, P = 0.711) and SS.
As shown in Table 3, there was no significant difference in the age at onset or age at surgery between the two groups. However, the duration of deviation was significantly different between the groups (2.08 ± 0.84 vs. 4.23 ± 1.36, P < 0.001), suggesting that the SS rate is affected by the length of disease development. Subjective deviation (-8.00 vs. -11.00, P = 0.049) and amplitude of fusional divergence (6.52 ± 4.10 vs. 4.80 ± 2.59, P = 0.032) were also significantly different between the SS and SF groups.
| Characteristics | SS Group (n = 62) | SF Group (n = 20) | t/z/χ2 | P-Value |
|---|---|---|---|---|
| Age at onset (y) | 5.30 ± 2.63 | 4.77 ± 2.55 | 0.636 | 0.531 |
| Gender; No. (%) | ||||
| Male | 29 (46.8) | 12 (60.0) | 1.058 | 0.221 |
| Female | 33 (53.2) | 8 (40.0) | ||
| Duration of deviation (y) | 2.08 ± 0.84 | 4.23 ± 1.36 | 8.457 | < 0.001 |
| Age at surgery (y) | 7.24 ± 3.84 | 8.60 ± 4.57 | 1.134 | 0.193 |
| Subjective deviation (range) | -8.00 (-12.00 - 4.00) | -11.00 (-14.00 - 7.25) | -1.965 | 0.049 |
| Refractive (spherical equivalent, diopters) | ||||
| Right eye | -0.25 (-2.00 - 0.53) | -0.75 (-2.09 - 0.69) | -0.357 | 0.721 |
| Left eye | -0.38 (-1.31 - 0.50) | -0.50 (-1.75 - 0.50) | -0.314 | 0.753 |
| Breakpoint (degrees of arc) | ||||
| Fusional divergence | 3.50 (-1.00 - 9.00) | 3.50 (-3.75 - 9.75) | -0.536 | 0.592 |
| Fusional convergence | -14.26 ± 5.03 | -15.10 ± 4.42 | 0.669 | 0.505 |
| Amplitude (degrees of arc) | ||||
| Fusional divergence | 6.52 ± 4.10 | 4.80 ± 2.59 | 2.204 | 0.032 |
| Fusional convergence | 11.85 ± 6.99 | 12.70 ± 6.28 | -0.481 | 0.632 |
| Angle of deviation (prism, diopters) | -35.08 ± 13.54 | -39.50 ± 15.97 | 1.214 | 0.228 |
| BMI (kg/m2) | 22.56 ± 4.88 | 23.89 ± 6.98 | 0.949 | 0.346 |
| Operation duration (min) | 35.23 ± 10.55 | 38.26 ± 14.23 | 1.022 | 0.310 |
| Family history; No. (%) | 3.277 | 0.070 | ||
| Yes | 10 (16.1) | 7 (35.0) | ||
| No | 52 (83.9) | 13 (65.0) |
Univariate Analysis of Surgical Success a
4.4. Multivariate Analysis for Surgical Success
To control for potential confounding variables, a multivariate analysis of SS was performed. As shown in Table 4, the duration of deviation (OR = 1.217, 95% CI: 1.021–1.447, P = 0.031), the angle of deviation (OR = 1.190, 95% CI: 1.013–1.376, P = 0.033), and subjective deviation (OR = 1.127, 95% CI: 1.024–1.582, P = 0.030) were identified as independent factors for SS. However, gender, age at surgery, right and left eye refraction, fusional vergence, fusional divergence, fusional convergence, Body Mass Index (BMI), operation time, and family history were not found to be independent factors affecting SS.
| Characteristics | OR | 95% CI | χ2 | P-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender (female vs. male) | 0.175 | 0.029 | 1.063 | 3.584 | 0.058 |
| Age at surgery (y) | 1.104 | 0.616 | 1.332 | 0.252 | 0.615 |
| Duration of deviation (y) | 1.217 | 1.021 | 1.447 | 4.615 | 0.031 |
| Refractive right eye | 1.225 | 0.395 | 1.687 | 0.301 | 0.583 |
| Refractive left eye | 1.149 | 0.390 | 1.940 | 0.116 | 0.733 |
| Angle of deviation (prism, diopters) | 1.190 | 1.013 | 1.376 | 4.524 | 0.033 |
| Subjective deviation | 1.127 | 1.024 | 1.582 | 4.709 | 0.030 |
| Fusional vergence | 1.026 | 0.897 | 1.174 | 0.140 | 0.708 |
| Fusional divergence | 1.025 | 0.873 | 1.088 | 0.208 | 0.648 |
| Fusional convergence | 1.024 | 0.913 | 1.046 | 0.441 | 0.507 |
| BMI (kg/m2) | 0.932 | 0.659 | 1.318 | 0.160 | 0.689 |
| Operation duration (min) | 1.148 | 0.597 | 1.271 | 0.513 | 0.474 |
| Family history (yes vs. no) | 4.225 | 0.072 | 8.776 | 0.374 | 0.865 |
Multivariate Analysis of Surgical Success
4.5. Predictive Indices of Subjective Deviation for Surgical Success
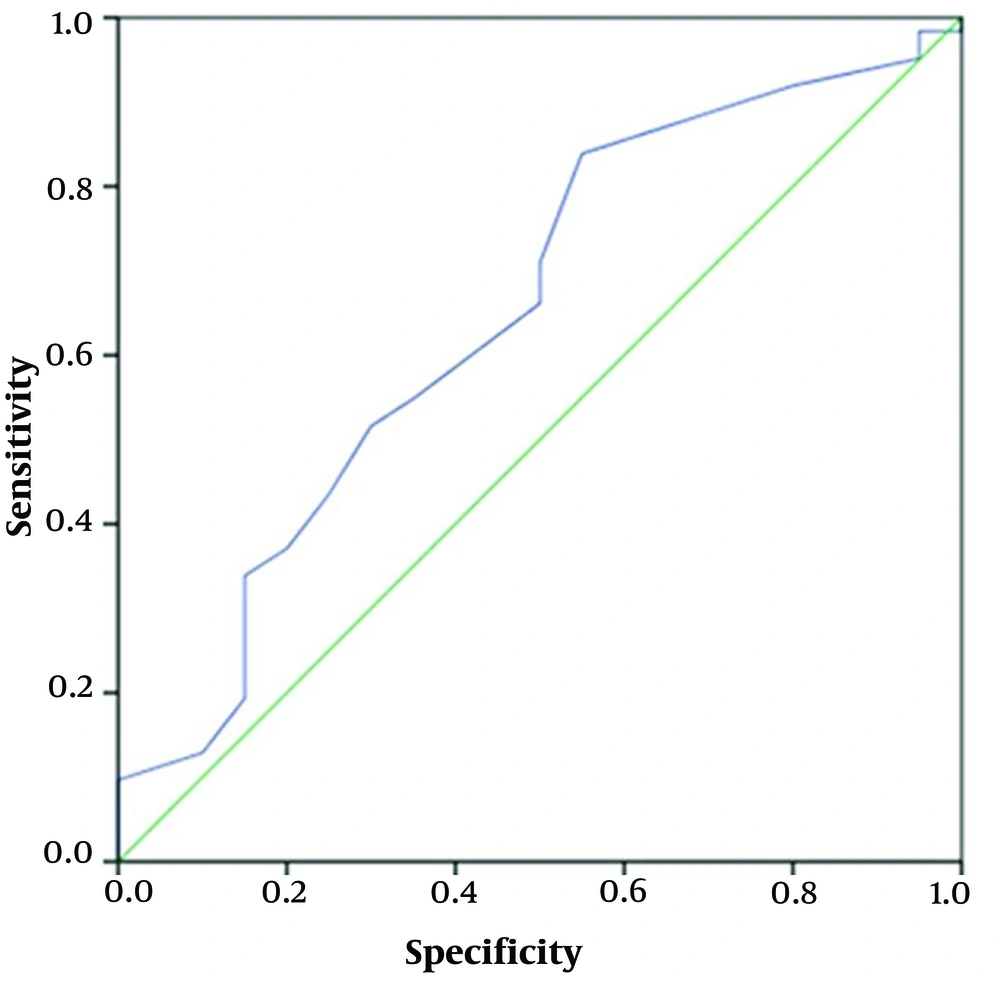
Finally, we evaluated the predictive index of potential independent factors for SS. As shown in Table 5, only subjective deviation (AUC = 0.646, 95% CI: 0.504–0.789, P = 0.049) demonstrated predictive value for SS. This suggests that subjective deviation may also reflect the severity of strabismus. When the subjective deviation is less than -12.5, the likelihood of a successful operation decreases (Figure 1). Additionally, the postoperative adverse reactions reported in the two groups included foreign body sensation caused by sutures (12 cases), conjunctival edema (17 cases), brief visual doubling (22 cases), and postoperative nausea under general anesthesia (3 cases).
| Predictors | Cut-off Value | ROC Curve | ||
|---|---|---|---|---|
| AUC | 95% CI | P-Value | ||
| Subjective deviation for SS | -12.5 | 0.646 | 0.504 - 0.789 | 0.049 |
ROC Curve
5. Discussion
Intermittent exotropia is the most common type of pediatric strabismus and is often preceded by a stage of exophoria, which significantly affects visual performance (10). The findings from the present study indicate no significant difference in age between the SS and SF groups. However, the duration of deviation was significantly different. Studies have reported that surgery before age 7 can lead to better surgical outcomes, including improved post-operative stereoscopic vision (11, 12). In our study, the lack of significant age differences between the groups suggests that disease duration more clearly impacts prognosis. A possible explanation could be the structural changes in the periocular tissue due to the longer duration of IXT, which alters elastic forces and affects final postoperative correction.
The most significant characteristic of IXT is the intermittent onset of exotropia, which can range from occasional to nearly constant throughout daily life (13). Despite IXT being one of the most common subtypes of strabismus, its natural etiology remains unclear. Exodeviation or divergent squint results from obstacles to the development or maintenance of binocular vision and/or defective action of the medial rectus muscles. Fusion is thought to be related to the control of IXT (14). Fusional vergence, the ability to maintain binocular vision under specific conditions, is usually examined with prisms or a synoptophore (15, 16). Deteriorating binocular vision, especially at a distance, is a frequent reason for surgical intervention in IXT (17). Measuring the vergence range is a standard method to assess the stability of binocular vision and the ability to cope with heterophoria (18). The synoptophore, derived from the laboratory instrument originally conceived by Hering (19), plays a fundamental role in studying the sensorimotor cooperation of the eyes. Although prisms are commonly used to detect fusion vergence amplitude, the synoptophore is crucial for this assessment (20). Jampolsky noted that when fusion vergence in IXT was detected with a prism bar, the patient had already used convergence to maintain orthophoria, resulting in a smaller amplitude of fusion convergence due to the "deconvergence" state (21, 22). Consequently, the amplitude of fusion divergence was usually larger.
Fusional vergence is crucial for maintaining normal ocular alignment during fixation of an object, and the amplitude of fusional vergence reflects the ability to maintain orthophoria under specific conditions (23). In the present study, we examined changes in fusional vergence after IXT surgery using a synoptophore. Initially, superposition was detected and recorded, followed by a detection process intended to reflect the true fusional vergence in patients with IXT. We found that postoperative fusional vergence breakpoints showed significant changes in both the SS group and the SF group, with greater changes observed in the SS group. This suggests that patients in the SS group had a better ability to maintain orthophoria compared to those in the SF group.
Our results indicated differences in postoperative breakpoints for fusion divergence and convergence, as well as in the amplitude of fusion divergence, between the SS and SF groups. Fu et al. examined fusion vergence in patients with IXT using both traditional prism bars and a synoptophore. They found that the mean breakpoints for divergence were comparable to those of normal subjects when measured with the synoptophore but significantly larger when measured with the prism bar. When fusion vergence is assessed using a prism bar, the patients first undergo detection from a spontaneous binocular fusion state, followed by step prism detection. Consequently, base-in (BI) prisms initially result in a relaxation of convergence until the deviation is neutralized (7). Some researchers suggest that convergence is normal in children with IXT, while others have shown it to be greater than the normal total convergence amplitude (8). In patients undergoing surgery for IXT, eye position may gradually drift outward over time, with fusional vergence potentially playing a role in the deterioration of control (24, 25).
As is known, both breakpoints and amplitudes encompass fusion divergence and fusion convergence (26). Our results suggest that changes in the breakpoint of fusion convergence were more significant than those in fusion divergence between the SS and SF groups. This indicates that external fusion function may have a lesser impact on surgical outcomes in patients with exotropia. Importantly, breakpoints and amplitudes of fusion convergence differed significantly between the SS and SF groups. The greater change observed in the SS group suggests a stronger internal fusion function, which may be related to changes in eye position or the balance of extraocular muscle strength after surgery. Additionally, the significant difference in the duration of deviation suggests that the success rate of surgery is influenced by the cumulative duration of the disease. As IXT progresses, both the strabismus rate and binocular vision are affected differently (27). Typically, distance stereo vision deteriorates first, and the duration of binocular synergy decreases. These factors may contribute to the reduced success rate of surgery with a longer disease course. For heterophoria to remain compensated, the fusional reserve opposing the heterophoria should be at least twice the size of the heterophoria (28). Fu et al. reported that, in children with IXT, the distance between the recovery point and breakpoint for both convergence and divergence was larger than in controls when detected using a prism bar and synoptophore. Additionally, Fan Yuyan’s study demonstrated that fusion function and stereo vision in IXT patients improved after binocular lateral rectus recession (7), which is consistent with our findings. In summary, our results showed that the internal fusion function in patients in the SS group was stronger compared to those in the SF group, and a longer course of IXT may lead to a decreased success rate of surgery. Therefore, clinical surgery is ideally performed in the early stages of the disease.
This study indicated that subjective deviation, duration of deviation, and angle of deviation may be independent factors for SS. Economides et al. found that bilateral occlusion could reduce ocular deviation in IXT (27). Subjective deviation is a key aspect of binocular vision function, representing the ability to integrate sensory information from both eyes. On the synoptophore, subjective deviation refers to the alignment of one examination picture (e.g., a lion) with another (e.g., a cage). In the SS group, the subjective deviation was more inclined toward the front, indicating a greater ability to achieve alignment in this position, which may suggest that preoperative strabismus was not particularly severe. In patients with IXT, a smaller subjective deviation means that the patient needs a larger exotropia angle to receive image information from both eyes and achieve fusion.
The innovation of this paper lies in exploring the independent factors affecting the success of surgery in IXT patients, which could help improve the success rate of clinical surgeries. However, there are some limitations to this study. The sample size used is relatively small, and the single-center design limits the diversity of the patient population studied. Additionally, due to the early approval process of this study, the data may lack timeliness, although it is accurate and reliable. Potential confounding factors such as variations in surgical techniques, surgeon experience, and individual patient differences may also affect the results. Future research will address these issues and focus on investigating the predictive value of fusional vergence measurements for surgical outcomes, as well as examining the long-term stability of postoperative fusional vergence changes.
5.1. Conclusions
The postoperative breakpoints of fusional divergence and convergence, and the amplitude of fusional divergence, were significantly different between the SS and SF groups. The duration of deviation, the angle of preoperative deviation, and subjective deviation are independent factors affecting SS. Subjective deviation demonstrated predictive value for SS and may also reflect the severity of strabismus.