1. Background
The efficiency of a country's healthcare system is assessed by many factors, with one of the most crucial being neonatal mortality (1). Neonatal mortality is defined as the death of a newborn within the first 28 days of life (2). The neonatal mortality rate (NMR) in communities has decreased due to economic and social developments and the implementation of effective interventions. According to the second target of the Health-related Sustainable Development Goals (SDG-3), countries worldwide committed to reducing the NMR to 12 deaths per 1 000 live births by 2030 (3, 4). Previously, reducing infant mortality by two-thirds between 1990 and 2015 was one of the Millennium Development Goals (MDGs) adopted voluntarily by 189 countries (5).
There are numerous indices to measure child mortality rates, including the under-five child mortality rate (U5MR), NMRs, child mortality rates (CMRs), and infant mortality rates (IMRs) (6). In 2015, there were 2.7 million cases of NMR worldwide, accounting for 45% of all deaths in children under 5 years of age (7). Reports indicate that upper-middle-income countries experienced a substantial 73% decrease in NMR from 1990. In contrast, low-income countries exhibited a lower decrease of 45%, highlighting the need for further improvements in these regions (8).
A wide range of studies have revealed that the most common causes of neonatal mortality in developing countries are infectious diseases, asphyxia, and congenital disorders (9, 10). According to the World Health Organization (WHO), preterm birth accounts for 30% of neonatal deaths worldwide, sepsis or pneumonia 27%, asphyxia 23%, birth defects 6%, neonatal tetanus 4%, diarrhea 3%, and other causes contribute to 7% of all neonatal mortality (11). In the past decade, neonatal mortality has significantly declined, largely due to decreases in deaths caused by 2 main factors: Birth asphyxia (34% of total reductions) and prematurity (21%) (12).
To achieve the Sustainable Development Goals (SDGs), it is crucial to identify and update factors affecting NMR through applied research. Several studies have been conducted in Iran and other countries to determine the factors influencing NMR (13-17); however, there is no comprehensive research on the West Azerbaijan province in Iran.
2. Objectives
In this study, we aimed to investigate the rates and causes of NMR in West Azerbaijan to provide local policymakers with data for designing effective strategies to accelerate the reduction of neonatal mortality.
3. Methods
3.1. Data Sources
We conducted a population-based cross-sectional study using data from the Child Mortality Surveillance System (CMSS) in West Azerbaijan province, Iran. The target population comprised all children under 28 days of age who were permanent residents of West Azerbaijan and who died between 2013 and 2022. Data were obtained from the CMSS conducted by the West Azerbaijan University of Medical Sciences, which is designed to be provincially and regionally representative. The system covers all deaths of children under 28 days old in all 17 counties (Shahindezh, Poldasht, Tekab, Shot, Maku, Urmia, Khoy, Naqadeh, Mahabad, Salmas, Oshanvieh, Chaldoran, Miandoab, Sardasht, Chaypareh, Piranshahr, Bukan). The study was approved by the Ethical Committee of Urmia University of Medical Sciences (No: IR.umsu.rec.1395.450) and the WHO Regional Office for the Eastern Mediterranean.
3.2. Procedures
To compile a comprehensive database, we collected data on various aspects of the neonates, including their age at death, gender, date and place of death, delivery type, and gestational age, in order to create a worklist for each deceased case. The NMR was calculated as the number of deaths within 28 days from birth per 1 000 live births during the same time period. Neonatal deaths were categorized as early neonatal deaths (within 7 days after birth), late neonatal deaths (deaths between 7 and 27 days after birth), and post-neonatal deaths (occurring 28 days after birth). Additionally, preterm birth was defined as infants born alive earlier than 37 weeks of pregnancy, full-term birth was classified as birth occurring between 37 and 42 weeks, and infants born after 42 weeks were considered post-term. Statistical analyses were performed using SPSS (version 21.0, SPSS Inc., Chicago, Illinois, USA). The resulting data were recorded in Microsoft Excel 2019 and analyzed using descriptive statistics (mean ± SD) and No. (%).
4. Results
In this study, a total of 3,689 immediate reports of neonatal deaths (< 28 days) were investigated from 2013 to 2022. Among them, 52.97% were males, with an average gestational age of 31.85 ± 5.56 weeks. Of the total deaths, over 72 percent occurred in preterm infants, and 69 percent were associated with cesarean section deliveries. In both genders, most deaths occurred in the hospital, with death at home ranking second, and a lower percentage of deaths occurred during dispatch (Table 1).
| Variables | Male | Female |
|---|---|---|
| Total Number | 1957 | 1732 |
| Gestational age | ||
| Preterm | 969 (73.3) | 756 (72.4) |
| Full term | 346 (26.1) | 287 (27.5) |
| Post-term | 7 (0.5) | 1 (0.001) |
| Death age (day) | ||
| Early neonatal death | 1289 (76.2) | 989 (74.7) |
| late neonatal death | 378 (23.4) | 319 (24.1) |
| Post neonatal death | 23 (1.4) | 15 (1.2) |
| Delivery types | ||
| Caesarean | 1318 (69.7) | 984 (68.4) |
| Natural | 571 (30.2) | 454 (31.5) |
| Death places | ||
| Hospital | 1803 (95.4) | 1375 (94.3) |
| Home | 59 (3.1) | 61 (4.2) |
| During dispatch | 28 (1.5) | 21 (1.5) |
a Variables are expressed as No. (%).
In total, neonatal deaths from 17 major causes were reported (Table 2). The top four primary causes were perinatal prematurity (32.3%), perinatal cardiovascular and respiratory disorders (25%), chromosomal and congenital disorders (15.3%), and perinatal hematologic and hemorrhagic disorders (10.9%) in 2013. While the order of diagnosis was similar in 2022, it became perinatal prematurity (36.8%), perinatal cardiovascular and respiratory disorders (14.6%), perinatal hematologic and hemorrhagic disorders (13.5%), and chromosomal and congenital disorders (8.7%) (Table 2).
| Cause of Death | 2013 | Cause of Death | 2016 | Cause of Death | 2022 |
|---|---|---|---|---|---|
| Perinatal prematurity | 129 (32.3) | Perinatal prematurity | 127(35.2) | Perinatal prematurity | 130 (36.8) |
| Perinatal cardiovascular and respiratory | 100 (25) | Chromosomal and congenital disorders | 66 (18.4) | Perinatal cardiovascular and respiratory | 52 (14.6) |
| Chromosomal and congenital disorders | 61 (15.3) | Perinatal hematologic and hemorrhagic disorders | 50 (13.8) | Perinatal hematologic and hemorrhagic disorders | 48 (13.5) |
| Perinatal hematologic and hemorrhagic disorders | 44 (10.9) | Perinatal cardiovascular and respiratory | 42 (11.6) | Chromosomal and congenital disorders | 31 (8.7) |
| Perinatal infection | 20 (5) | Other prenatal disorders | 27 (7.4) | Other prenatal disorders | 22 (6.2) |
| Other prenatal disorders | 18 (4.4) | Perinatal infection | 14 (4) | Cardiovascular disorders | 14 (4) |
| Unknown | 7 (1.6) | Unknown | 7 (2.0) | Perinatal infection | 11 (3) |
| Metabolic and nutritional disorder | 6 (1.4) | Metabolic and nutritional disorder | 6 (1.6) | Gastrointestinal disorders | 8 (2.2) |
| Accidents | 6 (1.4) | Cardiovascular disorders | 5 (1.4) | Respiratory disorders | 7 (2) |
| Cardiovascular disorders | 3 (0.7) | Accidents | 4 (1.2) | Nervous system disorders | 7 (2) |
| Meconium aspiration | 3 (0.7) | Meconium aspiration | 4 (1.2) | Accidents | 6 (1.7) |
| Gastrointestinal disorders | 2 (0.3) | Gastrointestinal disorders | 3 (0.8) | Meconium aspiration | 6 (1.7) |
| Respiratory disorders | 2 (0.3 | Respiratory disorders | 2 (0.5) | Unknown | 5 (1.4) |
| Nervous system disorders | 2 (0.3) | Urogenital disorders | 2 (0.5) | Metabolic and nutritional disorder | 4 (1.2) |
| Immune and hematopoietic system disorders | 1 (0.2) | Immune and hematopoietic system disorders | 1 (0.2) | Infectious and parasitic diseases | 2 (0.56) |
| Infectious and parasitic diseases | 1 (0.2) | Nervous system disorders | 0 | Immune and hematopoietic system disorders | 1 (0.27) |
| Urogenital disorders | 0 | Infectious and parasitic diseases | 0 | Urogenital disorders | 0 |
a Variables are expressed as No. (%).
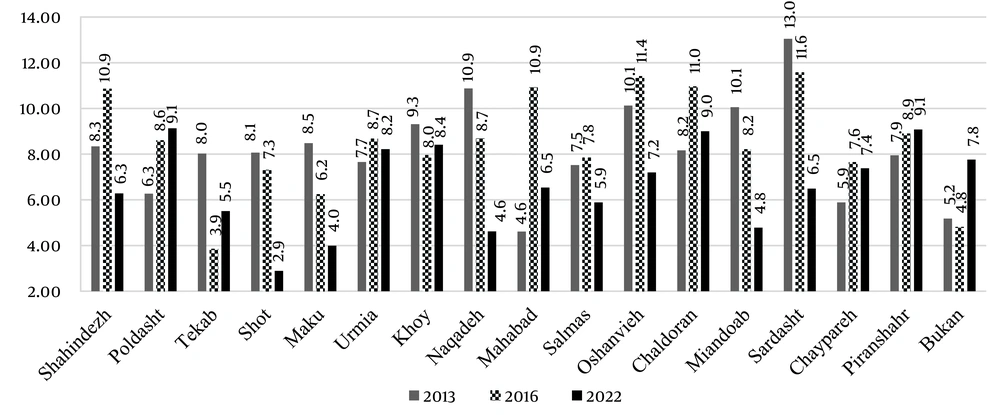
Neonatal mortality is unevenly distributed across cities within the West Azerbaijan province (different cities within the Urmia University of Medical Sciences), with the highest mortality rate in Poldasht city (9.13 per thousand live births) and the lowest mortality rate in the city of Shot (2.89 per thousand live births). The trend in mortality rates in cities also shows that in cities like Poldasht, Piranshahr, and Urmia, an increasing trend is observed from 2013 to 2022 (Figure 1).
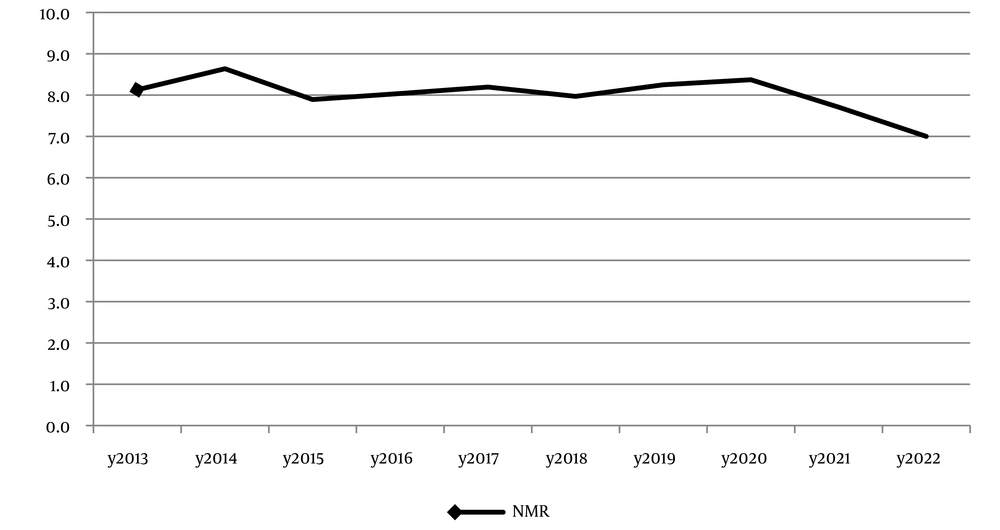
Based on the data depicted in Figure 2, it can be observed that the NMR from 2013 to 2022 has demonstrated slight fluctuations. The NMR has ranged between 7 and 8.6 during this period. The recorded rates for each year are as follows: 8.1, 8.6, 7.9, 8, 8.2, 8, 8.3, 8.4, 7.7, and 7. Overall, there is a general pattern of minor variations, with some years showcasing a slight increase or decrease in the NMR.
5. Discussion
The study revealed that neonatal mortality in West Azerbaijan was 7 per 1 000 live births in 2022, marking a decrease over the previous three years. However, an assessment over 5 years revealed no significant change in mortality trends from 2018 to 2022. The Global Burden of Disease (GBD) report indicated that in 1990, the neonatal mortality rate in West Azerbaijan was 35.5 per 1 000 live births (18). Since then, the likelihood of neonatal death in the first month has decreased by 76.9% over three decades. In response, the Iranian Government's Ministry of Health and Medical Education (MOHME) has launched several nationwide health programs aimed at enhancing care for pregnant women, neonates, and infants. These include primary health care (PHC), screening for congenital abnormalities, immunizations, the family physician plan, and prenatal diagnostic testing. Notably, West Azerbaijan province has met the SDG 3 target for neonatal mortality, which is below 12 per 1000 live births, although cities like Shahindezh and Poldasht still require targeted strategies from local policymakers to further reduce neonatal mortality.
The study also found that the mortality rate among boys (55.7%) was higher than among girls (44.3%), aligning with previous research (19, 20). Furthermore, the neonatal mortality rate (NMR) for cesarean sections was significantly higher than for vaginal deliveries, suggesting cesarean delivery as a potential risk factor for infant mortality. This is supported by population-based case-control study suggests that cesarean delivery may be considered a risk factor for infant mortality (OR = 1.97) (21). Another case-control study in Iran estimated that the risk of neonatal death in caesarean section delivery was 3.34 times higher than normal vaginal delivery (22). Similar to earlier studies conducted in Iran (23, 24), this study demonstrated that perinatal disorders such as prematurity, cardiovascular and respiratory disorders, and hematologic and hemorrhagic disorders as leading causes of neonatal death. A related study in Isfahan highlighted prematurity and congenital malformation as major contributors to NMR. Additionally, a recent study spanning from 1990 to 2019 (18) across Iran's provinces found neonatal disorders and birth defects as the leading causes of NMR (25), with preterm birth being the foremost cause of neonatal death globally, followed by congenital diseases (26).
Despite its strengths, including a population-based approach and comprehensive death coverage, our study acknowledges limitations. It lacked access to potential influencing factors on child mortality, such as birth weight, birth order, pregnancy status, prenatal and postnatal care, and socioeconomic status. The retrospective design and reliance on secondary data may have introduced data quality issues, including misclassification and classification bias. Furthermore, the potential bias from the shifting and relocation of experts in children's programs at health centers could have affected the data quality.
5.1. Conclusions
The findings of the present study indicate that, despite a convergence in trends, disparities in neonatal mortality persist across West Azerbaijan province. While the results of this study, along with those from other Iranian provinces, suggest that the SDG 3 target for neonatal mortality has been met, there remain variations in mortality rates and specific reasons for these differences among the various cities within the province, each with distinct socioeconomic conditions. This necessitates greater focus and the development of tailored intervention strategies.