1. Background
The modern medical model (1) emphasizes dynamic complementarity among bodily, psychological, and social factors, moving beyond the previous solely biological model. However, due to their incomplete physiological and psychological development, children have poor adaptability to unfamiliar environments. This is especially evident during invasive diagnostic and therapeutic processes, where they are more likely to cry and experience fear (2). This not only complicates diagnosis and treatment, impacting children’s recovery, but also induces anxiety and tension in both children and parents. This can indirectly lead to medical disputes, or even affect the children's emotional and cognitive development, potentially influencing their social behavior in adulthood (2-4). Studies have indicated that during hospitalization, 50% of children's pain and fear are not relieved in time, and that repeated pain without prior intervention significantly increases the incidence of chronic pain in adulthood (2-5). The European Society for Pediatric Anesthesiology advocates for non-pharmacological preventive strategies to manage postoperative pain in children, as analgesics do not alleviate anxiety (6). These non-pharmacological strategies involve diverting children’s attention to more engaging activities to distract them from pain stimuli.
Alternative therapies such as massage therapy, relaxation techniques, diversion, and music therapy are methods to control your child’s pain without medicine and can be effective in improving their comfort during treatment (7). In the 1980s, Dr. Michael Christensen in the United States collaborated with clown actors to implement clown therapy in hospitals. He discovered that through humorous and witty language, along with comical and exaggerated performances, he could quickly establish a relationship of trust and friendship with the children, significantly alleviating their pain, fear, and anxiety. This has proven to be positively significant in improving treatment compliance. The medical clown care model is a behavioral intervention method that aims to relieve stress and anxiety by using clowns' performances and interactions to attract children's attention and help them shift their focus away from pain and illness (8). This not only effectively relieves the fear and stress caused by treatment for children but also improves the doctor-patient relationship and achieves harmony between doctors and patients (9-11).
Several hospitals offer clown care therapy. For example, the Hospital for Sick Children in Toronto has a therapeutic clown program that has been in operation for over 25 years and has helped thousands of children (11). Another example is the Emunah Children’s homes, which have a Social Clowning Program instrumental in helping at-risk children begin to heal from their past trauma (9). The Dr. Clown Foundation also brings joy to Montreal’s long-term care homes and hospitals (10).
However, due to cultural differences and variations in medical backgrounds, there has been limited research on the medical clown care model in China. With a large population and relatively scarce medical resources, hospitals in China tend to focus more on disease resolution, often overlooking the importance of a comfortable medical experience for children. By adapting foreign medical clown models (8-11), we have developed our own medical clown care team tailored to the local conditions of our hospital.
2. Objectives
This study aims to explore the effectiveness of the medical clown care model during the perioperative period for children with inguinal hernia in our hospital, in order to provide a reference for the implementation of medical clown care in pediatric healthcare in China.
3. Methods
3.1. General Clinical Data
A total of 173 boys and 63 girls with an average age of 4.95 ± 0.83 years, who underwent laparoscopic high ligation of the inguinal hernia sac at Huai'an First Hospital Affiliated to Nanjing Medical University between January 2019 and January 2023, were selected as research subjects. The children were grouped according to the admission sequence. At the start of the study, using a blinded method, a nurse assigned the first child admitted to the hospital to the control group, then the next child admitted was placed in the intervention group by the same nurse, and so forth. The doctors explained the medical clown care model to the parents of the children in the intervention group and requested their approval for their children to participate. If the parents did not agree to the medical clown care model, their children were assigned to the control group.
Inclusion criteria for the children included: (1) preschool children aged 4 - 6 years with normal growth and development; (2) parents (father or mother) who voluntarily agreed to participate in this study and signed informed consent. Exclusion criteria included: (1) children with incarcerated inguinal hernia undergoing emergency surgery or those undergoing other surgical procedures at the same time; (2) children with severe illness, significant complications, or severe complications during treatment; (3) children with incomplete clinical data and treatment process.
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of our hospital (KY-2018-122-01, approved on Nov. 24, 2018). Written informed consent was obtained from the parents of the children participating in the study.
3.2. Control Group Implementation Plan
After admission, children underwent the routine diagnostic and treatment processes associated with fast recovery surgery. This included preoperative health education, prevention of postoperative complications, and drug treatment. Detailed instructions were provided on perioperative precautions, with particular emphasis on communication with parents to collaboratively complete preoperative blood collection, peripheral venipuncture, and other invasive procedures with medical staff. Preoperative evaluation may also require intravenous injections to facilitate the administration of anesthesia. In clinical practice, after venipuncture was performed by nursing staff, blood was collected from the indwelling needle for testing, allowing one invasive procedure to accomplish two tasks and thus reduce the pain experienced by the children. After the surgery, the doctor injected 5ml of 0.25% ropivacaine into the local surgical incision to manage pain. During the postoperative period, the children were still fasting, making oral analgesics unfeasible. When anesthetics are administered intravenously, they can easily induce side effects such as nausea and vomiting in children. Therefore, in this study, when postoperative pain occurred, analgesics were administered according to the child's condition (e.g., ibuprofen suppository for children at 10 mg/kg per rectum).
3.3. The Intervention Group Implemented Medical Clown Diagnosis and Treatment Model on the Basis of the Above-Mentioned Methods
The detailed process is as follows:
(1) Establishment of a specialized medical clown team: Under the guidance of the head nurse, the team included bed doctors, nursing team leaders, ward assistants, and specialist nurses. Searches were conducted through Web of Science, Wiley InterScience, Elsevier Science Direct, Springer Link, PubMed, Wanfang Medicine, CNKI, VIP, and other domestic and international databases for relevant literature on clown care during the perioperative period for children. Chinese keywords included: Clown (including medical clown, clown doctor, clown nursing), children; English keywords included: Clown, Child. After screening the retrieved literature based on its relevance to the subject and evidence level, data extraction was carried out. Based on the scientific validity and authenticity of the data, as well as the practicality and cost-effectiveness for our department, a preliminary implementation plan was formulated.
(2) Inviting relevant experts to evaluate the preliminary plan: This included one director of the infection control department, one preschool education teacher, and three doctors or nurses from outside the hospital who had experience in clown care.
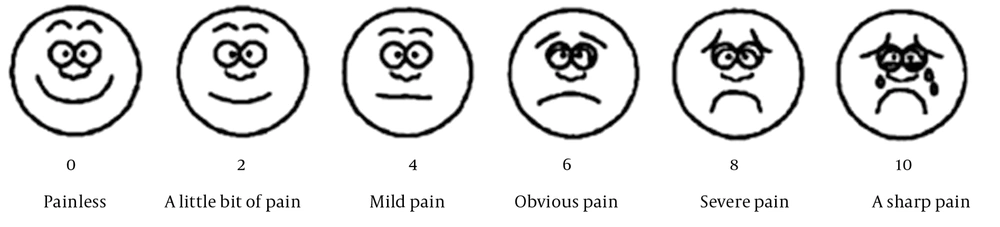
(3) Summarizing expert opinions and discussing within the group to determine the final clown care intervention plan, as shown in Figure 1.
(4) Conducting quality control training for bed doctors and ward assistants in our department to ensure the balance of intervention measures. After they have mastered the skills, they can carry out the application.
3.4. Certification and Regulation of Medical Clown Volunteers
(1) Training: Medical clown volunteers must complete professional training, which includes child psychology, medical knowledge, and interaction skills, as well as uphold patient privacy, adhere to medical ethics, and refrain from seeking undue benefits. This training ensures they acquire the appropriate qualifications and skills.
(2) Examination: Medical clown volunteers are required to pass an examination following their training to demonstrate that they possess the necessary knowledge and skills.
(3) Registration and Certification: After passing the examination, medical clowns must be registered and certified within their own organizations. This process ensures that they are qualified to provide healthcare services.
(4) Supervision: Medical clowns must undergo regular supervision by hospitals and community experts, which includes assessments, certification, and evaluations, to ensure they continue to provide high-quality services.
3.5. Implementation of the Medical Clown Model
(1) Pre-treatment assessment: Before starting clown therapy, a comprehensive assessment of the children is conducted, involving healthcare personnel and parents. This assessment gauges the children's needs, fears, anxiety levels, and pain, as well as their physical and emotional states. It includes understanding the children's personalities, interests, hobbies, taboos, favorite cartoon characters, music, and more.
(2) Pre-treatment preparation: Based on the assessment results, targeted preparatory work is developed. This preparation involves selecting appropriate props and toys, wearing brightly colored clothes, and preparing performances and interactive content. Additionally, healthcare personnel explain the medical clown model to the parents, gaining their agreement and support.
(3) Interaction during treatment: Clown therapists engage with patients through performances, magic tricks, games, etc., to capture the children's attention. These activities are designed to help the patients relax and alleviate their pain and discomfort. Parents are encouraged to stay nearby to comfort the children when necessary, especially if the child becomes overly frightened or cries continuously for more than three minutes. Specific activities may include:
(1) Interactive games: Medical clowns can engage children in various enjoyable interactive games, such as a "treasure hunt" using small toys and props to create a joyful distraction from their ailments.
(2) Storytelling: Medical clown volunteers can narrate stories that help children understand their illnesses and teach them how to manage their health through engaging storylines.
(3) Performances: Medical clowns can entertain children with comical shows, including magic tricks, bubble blowing, and dancing.
(4) Painting: Medical clown volunteers can lead children in painting activities, which are effective for expressing emotions and feelings while simultaneously relieving stress and anxiety.
(5) Interactive Q&A: Medical clowns can conduct engaging Q&A sessions with the children, answering their questions about illness and health, and imparting health knowledge.
Post-treatment reflection: After the treatment is over, the clown volunteers need to reflect on the process of treatment, summarise the experience and lessons learnt from the treatment, and report to the healthcare personnel, so as to implement the next treatment in a better way. Follow-up assessment: After the child is discharged from the hospital, the clown volunteer needs to conduct a follow-up assessment of the child to understand the child's recovery, the effect of the treatment and the need for further treatment.
3.6. Evaluation Indicators
3.6.1. Children’s Pain Assessment
After invasive operations such as preoperative blood collection and peripheral venipuncture in both groups of children, their pain conditions were evaluated using the following methods:
1. FLACC Scale: Nurses used the modified Facial Expression, Legs, Activity, Cry, and Consolability (FLACC) Scale (12) to evaluate the children's pain level. The FLACC scale is designed for individuals who cannot verbalize their discomfort, particularly applicable to children between the ages of 2 months and 7 years. This scale ranges from 0 – 10 points, with 0 indicating no pain and 10 indicating severe pain. Each criterion—facial expression, limb movement, behavior, crying, and consolability—is scored 0, 1, or 2, with 0 points for relaxation and comfort, 1-3 points for slight discomfort, 4 - 6 points for moderate pain, and 7-10 points for severe pain or discomfort.
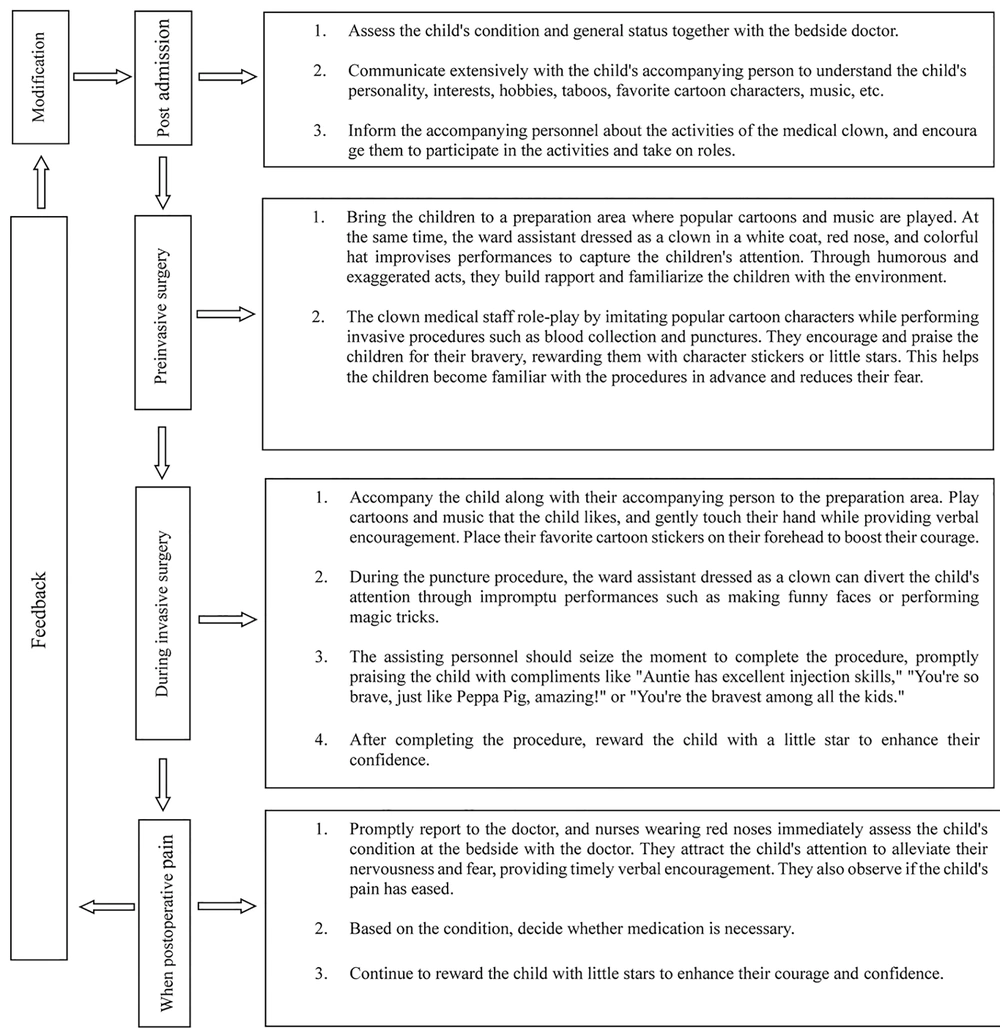
2. Wong-Baker FACES Pain Rating Scale – Revised (W-B FPS-R): Children described their pain level using six cartoon pictures from the W-B FPS-R, which is a self-report measure of pain intensity. The scale ranges from 0 (no pain) to 10 (most severe pain) and is ideally suited for children aged 4 to 16 years. It shows a strong linear correlation with visual analog pain scores (13). This tool requires no special equipment besides the provided photocopied faces, and is particularly recommended for use with young children (13-15). Emotional expressions on the scale range from smiling to crying, and children rated their pain accordingly (Figure 2).
(3) Statistical analysis: This involved the evaluation of the crying rate using the FLACC scale and the crying cessation rate after 1 minute of the invasive operation in both groups. Crying time was measured using a nurse's clock timer; the nurse started the timer when the child cried and stopped it once the child was comforted by the medical clowns and ceased crying after 1 minute.
To minimize bias and error, the FLACC scale was assessed by a nurse, and the W-B FPS-R scale was described by the children themselves.
3.6.2. Parents’ Anxiety State Assessment
Due to the immature psychological and physiological development of children, anxiety assessments may be misunderstood and contain errors. Therefore, Zung’s Self-Rating Anxiety Scale (SAS) (16) was used to evaluate the anxiety state of parents in both groups at admission and before the operation, but not the children. This scale consists of 20 items, with mild scores ranging from 50 - 59 points, moderate scores from 60 - 69 points, and severe scores of 70 points or more. The Cronbach's α coefficient of the Chinese version (17) used in this study is 0.788, and the content validity index is 0.954.
3.6.3. Clinical Intervention Effect Analysis
(1) Analyze the incidence of postoperative pain and the use of analgesics in the two groups of children; (2) evaluate the overall compliance of the two groups of children during this hospitalization at discharge, categorized into three levels: Strong resistance (forced to complete treatment), resistance (persuaded to complete treatment), and active cooperation (actively cooperates with treatment); (3) at discharge, the parents of the two groups of children evaluate their satisfaction with the treatment using the Likert Grading Scale (18), where 1 represents dissatisfaction, 2 represents relatively dissatisfied, 3 represents neutral satisfaction, 4 represents relatively satisfied, and 5 represents very satisfied. The Chinese version (19) used in this study, developed by Professor Zhang Tuohong's research team, has a Cronbach's α coefficient of 0.956 and a content validity index of 0.971.
3.7. Follow up
The children were followed for up to 12 months, with follow-ups occurring every three months. The data from the last follow-up were recorded and assessed.
3.8. Statistical Analysis
The data were analyzed using SPSS version 23.0 statistical software. Measurement data with a normal distribution were analyzed using the t-test and expressed as mean ± standard deviation (mean ± SD). Data with a skewed distribution were analyzed using the rank sum test and expressed as median [M (range)]. Count data were analyzed using the chi-square test or Fisher's exact probability method and expressed as rate or composition ratio. A P-value of < 0.05 was considered to indicate a statistically significant difference.
4. Results
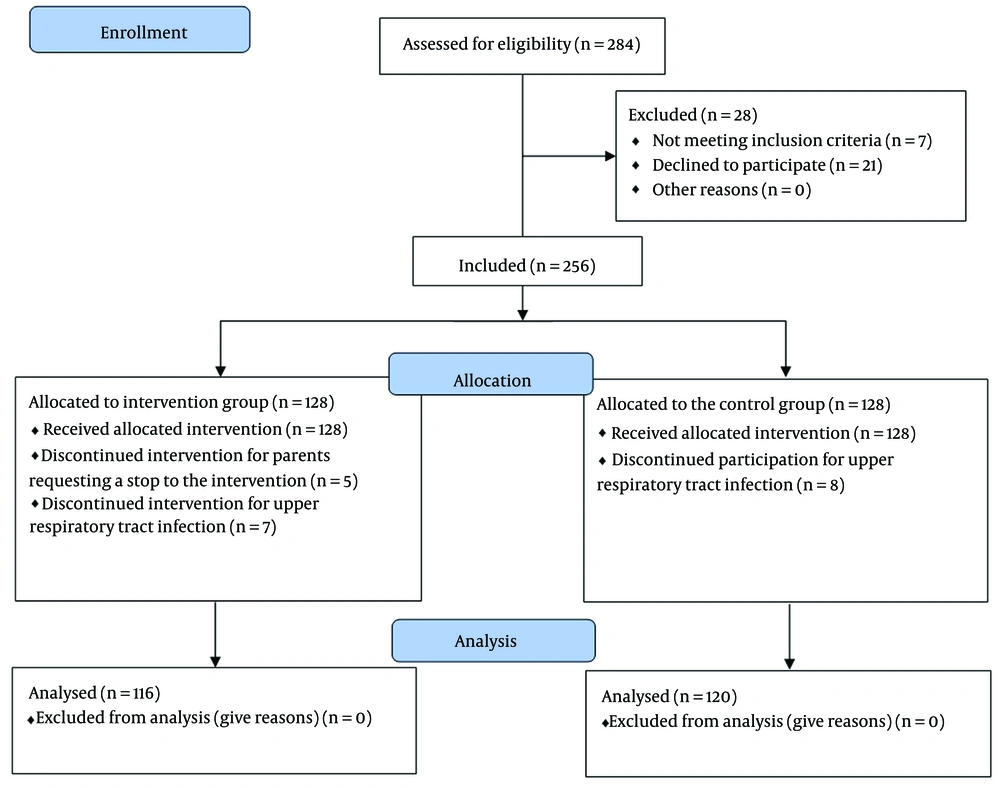
The children were divided into an intervention group (116 cases) and a control group (120 cases) using a random approach (Figure 3).
There were no statistically significant differences between the two groups in terms of age, gender, hernia sac location, operation time, parents' age, education level, and other general clinical data (P > 0.05), indicating that the groups were comparable (Table 1).
| Variables | Intervention Group | Control Group | t/χ2 | P-Value |
|---|---|---|---|---|
| Number of cases | 116 | 120 | ||
| Age (y) | 4.99 ± 0.83 | 4.90 ± 0.83 | 0.769 | 0.443 |
| Sex | 2.137 | 0.144 | ||
| Male | 90 (77.59 ) | 83 (69.17 ) | ||
| Female | 26 (22.41 ) | 37 (30.83 ) | ||
| Hernia sac location | 0.221 | 0.895 | ||
| Left | 68 (58.62 ) | 72 (60.00 ) | ||
| Right | 30 (25.86) | 28 (23.33 ) | ||
| Bilateral | 18 (15.52 | 20 (16.67 ) | ||
| Parent education level | 1.351 | 0.509 | ||
| Junior high and below | 58 (50.00) | 57 (47.50 ) | ||
| High school/vocational | 40 (34.48) | 49 (40.83 ) | ||
| University and above | 18 (15.52) | 14 (11.67 ) | ||
| Parent age (y) | 27.93 ± 4.79 | 28.79 ± 4.38 | 1.441 | 0.151 |
| Operation time (min) | 24.24 ± 5.94 | 25.38 ± 7.05 | 1.334 | 0.183 |
a Values are expressed as No. (%) or mean ± SD.
4.1. Comparison of Pain Levels During Invasive Procedures in Two Groups of Children
Both groups of children experienced some degree of pain during invasive procedures. The FLACC scores and W-B FPS-R scores of the intervention group were significantly lower than those of the control group, with a statistically significant difference between the two groups (P < 0.001). The crying rate during invasive procedures was 44.83% in the intervention group compared to 79.16% in the control group, showing a statistically significant difference (P < 0.001). The crying cessation rate within 1 minute after invasive procedures was 63.46% in the intervention group and 41.05% in the control group, also demonstrating a statistically significant difference (P = 0.009, Table 2).
| Variables | Intervention Group | Control Group | t/χ2 | P |
|---|---|---|---|---|
| Number of cases | 116 | 120 | ||
| Face Legs Activity Cry and Consolability Score (points) | 4.81 ± 2.07 | 6.71 ± 1.92 | 7.302 | 0.000 |
| Wong-Baker FACES Pain Rating Score (points) | 4.69 ± 2.24 | 7.02 ± 2.23 | 7.997 | 0.000 |
| Crying | ||||
| Yes | 52 (44.83) | 95 (79.17) | 29.609 | 0.000 |
| Crying stopped after 1 minute | ||||
| Yes | 33 (63.46) | 39 (41.05) | 6.753 | 0.009 |
a Values are expressed as No. (%) or mean ± SD.
4.2. Comparison of Anxiety Status Between Parents of Two Groups of Children
There was no statistically significant variation between the Zung SAS scores of parents in both groups at admission (P = 0.416), indicating consistency in balance. The Zung SAS score of parents in the intervention group before surgery was significantly lower than that at admission, showing a statistically significant reduction within the group (P < 0.001). In contrast, the decrease in the Zung SAS score before surgery compared to admission was not significant in parents of children in the control group, with no statistically significant change within the group (P = 0.273). There was a statistically significant difference between the two groups, with the Zung SAS score for parents in the intervention group being significantly lower than that for parents in the control group prior to surgery (P < 0.001, Table 3).
| Groups | n | Z-SAS Score Upon Admission | Preoperative Z-SAS Score |
|---|---|---|---|
| Intervention group | 116 | 58.41 ± 18.28 | 42.85 ± 14.17 |
| Control group | 120 | 55.21 ± 17.96 | 52.69 ± 17.54 |
| t | 1.359 | 4.730 | |
| P | 0.175 | 0.000 | |
a Values are expressed as mean ± SD.
4.3. Clinical Intervention Effect Analysis of Two Groups of Children
With a statistically significant difference between the two groups (P = 0.035), the incidence of postoperative pain in the intervention group was 18.97%, which was substantially lower than the 30.83% observed in the control group. The intervention group used analgesics at a rate of 27.27%, significantly lower than the control group's rate of 56.76%, with a statistically significant difference between the two groups (P = 0.028). There was also a statistically significant difference in overall compliance during hospitalization, with the intervention group showing much higher compliance than the control group (P = 0.004). At discharge, parents in the intervention group expressed significantly higher satisfaction with the treatment compared to those in the control group (P = 0.012). The satisfaction levels in the intervention group were higher than those in the control group, demonstrating a statistically significant difference (P < 0.05, Table 4).
| Groups | Cases | Satisfaction Scores of the Parents |
|---|---|---|
| Intervention group | 116 | 4.41 ± 1.01 |
| Control group | 120 | 4.06 ± 1.14 |
| t | 2.529 | |
| P | 0.012 |
4.4. The Follow Up Analysis of Two Groups of Children
During a one-year follow-up after discharge (Table 5), the recurrence rate of postoperative inguinal hernia was 1.72% in the intervention group and 2.5% in the control group, showing no statistically significant difference (P = 0.678). However, the number of cases of chronic pain (6 cases vs. 17 cases, P = 0.020), the duration of pain relief (11 days vs. 21 days, P = 0.048), and the number of cases requiring additional care (such as psychosocial care) (5 cases vs. 22 cases, P = 0.001) were significantly lower in the intervention group than in the control group. The rate of active cooperation in the intervention group was significantly higher than that in the control group (65.52% vs. 15.00%, P < 0.001).
| Groups | Cases | Recurrence of Postoperative Inguinal Hernia | chronic pain | the Time of Relief After the Pain Persists(Day) | Additional Care | Children's Adherence to Follow-up Appointments | Parents ‘overall Evaluation of Treatment | Post-discharge Health Care | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Active Cooperation | Resistance | Strong Resistance | Good | Fair | poor | Outpatient | Hospitalization | Emergency | |||
| Intervention group | 116 | 2 | 114 | 6 | 110 | 11.17±5.42 | 5 | 111 | 76 | 31 | 9 | 96 | 16 | 4 | 101 | 5 | 10 |
| Control group | 120 | 3 | 117 | 17 | 103 | 20.94 ± 10.84 | 22 | 98 | 18 | 55 | 47 | 77 | 33 | 10 | 88 | 13 | 19 |
| t | 0.173 | 5.425 | 2.096 | 11.448 | 68.222 | 10491 | 7.177 | ||||||||||
| P | 0.678 | 0.020 | 0.048 | 0.001 | 0.000 | 0.005 | 0.028 | ||||||||||
The one-year post-discharge follow-up survey revealed that the overall rate of positive feedback from the parents of the children in the intervention group was 82.76%, which was significantly higher than the 64.17% from the parents in the control group (P = 0.005). Regarding healthcare choices after discharge, the intervention group recorded 101 outpatient visits, 10 emergency visits, and 5 hospitalizations, while the control group had 88 outpatient visits, 19 emergency visits, and 13 hospitalizations (P = 0.028).
5. Discussion
Inguinal hernia is one of the most prevalent and frequent conditions in pediatric surgery. The cumulative incidence of inguinal hernia in boys under 15 years of age is 6.62%, and in girls, it is 0.74%, accounting for nearly 23% of major childhood diseases (20). Children represent a unique medical group; they have not yet developed cognitive and behavioral abilities and often lack self-control, which frequently results in low compliance and cooperation, increasing the occurrence of adverse medical events (2-5). Such a high incidence of inguinal hernia in children poses a significant challenge to perioperative diagnosis and treatment nursing. The medical clown care model has been gradually promoted and implemented in many countries, achieving notable clinical application effects in pre-anesthetic induction, invasive medical procedures, and routine management of acute and chronic diseases (9-11, 21).
When a relatively strong external stressor stimulates the body, it increases the secretion of hypothalamic-pituitary-adrenal cortex hormones through the hypothalamus-pituitary-adrenal cortex axis, promotes sympathetic nerve excitement, inhibits the release of endorphins, lowers the pain threshold, and increases the body’s sensitivity to pain. The neuroendocrine response in children is 3 - 5 times that of adults (22). Therefore, negative medical experiences such as encountering a "white coat" and "syringe" in an unfamiliar medical environment not only induce severe physiological stress responses in patients but also cause psychological trauma, such as anxiety and fear. A study shows (21) that nearly 60% of patients experience high levels of fear and stress during medical invasive operations. The results of this study indicate that during invasive procedures like blood collection and peripheral venous puncture, the FLACC score and the subjective W-B FPS-R score of the intervention group were reduced by 2 points compared to the control group. Additionally, the crying rate (44.83%) of the intervention group children and the crying cessation rate after 1 minute (63.46%) were also reduced by 20% - 35% compared to the control group (79.16%, 41.05%). This improvement may be attributed to the positive social trust effect produced by the clown care model.
In this study, clown doctors captured children’s attention in advance with intriguing costumes, such as red noses, and used humorous language, exaggerated performances, and effective encouragement to bridge the gap between doctors and children, alleviate fear of unfamiliar environments, and enhance children and parents’ trust and reliance on medical staff. In subsequent invasive procedures, clown doctors entertained the kids through role-playing, simulating performances of cartoon characters, playing children’s favorite music or cartoons, etc. This effectively diverted attention, relieved anxious emotions, and eased the tense medical atmosphere, preventing children from focusing entirely on the medical procedures. This approach can diminish the subjective sensation of pain influenced by non-somatic psychological factors such as fear (21). After a series of medical clown care interventions produced positive social trust effects, they also yielded remarkable physiological adaptation effects (23-25). By utilizing clown care to boost children’s courage and stimulate their sense of honor, it disrupts the vicious cycle of “pain-fear-pain,” improving their tolerance to postoperative pain.
In this study, only 18.97% of children in the intervention group experienced postoperative pain, significantly lower than the 30.83% in the control group. Moreover, when children in the intervention group experienced postoperative pain, medical staff used simple distractions such as dressing changes to capture the children's attention and alleviate their tension and fear. Through timely encouragement, staff helped children manage some psychological factors contributing to pain, enabling them to accurately assess their condition and decide whether drug treatment was necessary. Consequently, only 27.27% of children in the intervention group required postoperative analgesics, significantly lower than the 56.76% in the control group. This finding is consistent with the research by Zhang et al. (25), who noted that the medical clowning approach during pediatric surgeries can regulate the body's neuroendocrine functions and stimulate endorphin production in the brain, thus reducing responsiveness to painful stimuli. This approach effectively decreases the crying rate among affected children, alleviates pain and anxiety, and enhances treatment compliance, aligning with the outcomes observed in this study.
Moreover, the medical clown not only relieves the pain and anxiety of the patients but also creates a positive atmosphere during the perioperative period and helps improve the emotional climate among medical healthcare personnel, accompanying persons, and patients (26). When parents perceive an improvement in their children's well-being and experience less anxiety following interactions with the medical clown, they tend to be more satisfied with the hospital. Consequently, the children become more cooperative with the treatment and follow-up (27-29). Our follow-up results are consistent with these findings (26-29).
Compared to adults, children have lower cognitive levels and poorer self-control, making them more susceptible to negative medical experiences such as "white coat" and "syringe," often resulting in crying and making noise (30). The clown care model enhances communication with patients by considering the nature and physiological characteristics of children, producing positive trust effects and physiological adaptation effects, and improving patient comfort during treatment. The intervention group's overall compliance was nearly 20% higher than that of the control group, aligning with findings by Meiri et al., who reported a 21.32% increase in child cooperation when using the clown care model to treat children aged 2 to 10 in the emergency department (31).
Children are central to a family, and the parents of sick children are a high-risk group for anxiety disorders. The pain, crying, resistance, and fear of sick children are undoubtedly strong stimuli for their parents. Coupled with concerns about surgery, parents' anxiety levels typically peak before surgery (32). In this study, the implementation of clown care, a "child-centered" full-course "happy therapy," significantly reduced the incidence of pain and negative emotions in children, enhanced the comfort of their medical experience, and allowed parents to be present throughout the process and engage to some extent with the clown doctors in interactions with their children. This positive guidance improved patient compliance, and parents felt cared for and supported during the process, which helped reduce psychological stress and alleviate anxiety. Consequently, the preoperative anxiety score of parents in the intervention group was 15 points lower than at admission, while the control group's score only dropped by 3 points, showing a statistically significant difference (P < 0.001). Furthermore, in terms of treatment satisfaction, the intervention group scored significantly higher than the control group parents, further confirming that the medical clown model can effectively relieve parents' anxiety.
The clown care model employs techniques such as humorous language, comical performances, interesting costumes, and effective encouragement to establish trust with patients and enhance their comfort during treatment. It also entertains patients through role-playing, simulating cartoon characters' performances, and playing children’s favorite music or cartoons to divert their attention and alleviate anxiety. These techniques work in concert to generate positive trust effects and physiological adaptation effects, breaking the vicious cycle of “pain-fear-pain” for patients and enhancing their tolerance to postoperative pain. The clown care model has proven effective in reducing patients' pain levels, alleviating the anxiety of children's parents, improving children's treatment compliance, and increasing satisfaction with diagnostic and treatment activities. It represents a non-pharmacological, humanistic treatment mode that is worth promoting.
Furthermore, the medical clown model in our hospital serves as a public benefit activity. We conduct training sessions every three months to enhance the performance and interaction skills of the clown volunteers. For medical clowns performing an intervention for the first time, guidance is provided by medical staff and an experienced medical clown from the sidelines. Clown volunteers who have participated in medical clowning several times and achieved positive outcomes for patients will receive material incentives. Additionally, their commendable actions will be highlighted in the hospital to express praise and gratitude towards them.
5.1. Limitation of This Study
The study was a single-center study with limited samples, indicating a need for multicenter research to determine the generalizability of the results. The scope of this study was limited to preschool children with inguinal hernia during the perioperative period, thus the application field of the clown care model is relatively narrow. Further exploration of the practicality of the clown care model is still needed across multiple age groups and diseases. Additionally, due to the young age of the children, parents may participate in the medical clown model intervention where necessary. The direct participation of parents in the clown activities may have influenced the results, potentially leading to some bias.
5.2. Conclusions
Applying the clown care model during the perioperative period for pediatric inguinal hernia can effectively reduce children's pain levels, relieve parents' anxiety, improve children's treatment compliance, and increase satisfaction with diagnostic and treatment activities. Its impact is significant, making it a comfortable, non-pharmacological, humanistic treatment mode worth promoting.