1. Background
Breast milk plays a crucial role in promoting the physical and mental health of both mothers and infants. Breastfeeding contributes to maternal-infant bonding, decreases neonatal mortality, and lowers postoperative complications for mothers (1). Exclusive breastfeeding (EBF) for the first six months after birth can reduce the risk of developing chronic diseases later in life, such as diabetes, cardiovascular disease, obesity, and cancer. Breast milk provides all the necessary nutrition for optimal growth and development during the initial period (2). The failure to achieve EBF can increase the risk of infections, allergies, cognitive impairment, and a weakened immune system. These facts highlight the potential risks associated with not practicing EBF (3, 4).
Despite the numerous benefits of EBF, the worldwide trend of EBF is declining. In the United States, 65% of mothers breastfeed immediately after giving birth, but this rate drops to 25% by the sixth month postpartum. In Italy, the rate of breastfeeding after birth was initially 61%, which decreased to 49% by the third month postpartum (1, 2).
Various factors influence EBF. One of these factors is the method of delivery. The global rates of Caesarean section (C-section) have been steadily increasing, surpassing the World Health Organization's recommended range of 10-15%. For instance, the rate of C-sections in Turkey is as high as 52%, while in the USA, it stands at 30.2% (1, 5, 6). It has been found that C-sections have a negative impact on the duration and initiation of breastfeeding (1). The lower rates of EBF among mothers who undergo C-sections can be attributed to postpartum fatigue and pain, delayed initiation of breastfeeding, and an extended recovery time from anesthesia (5, 7).
Enhanced Recovery After Caesarean Surgery (ERACS) is a multimodal care pathway that begins preconception and includes antepartum optimization, intrapartum care, postpartum inpatient care, and outpatient support, all with the purpose of improving postoperative outcomes. It consists of 25 recommended procedures that define ERACS, further divided into preoperative, intraoperative, and postoperative stages. The preoperative stage comprises 5 recommended procedures: (1) Limiting fasting interval, allowing solid food up to 8 hours before delivery, and clear fluids up to 2 hours before delivery; (2) Providing nonparticulate liquid carbohydrate loading, such as 16 oz of clear apple juice up to 2 hours before delivery in non-diabetic women; (3) Educating patients regarding ERACS; (4) Providing breastfeeding preparation and education through prenatal classes; and (5) Optimizing hemoglobin levels by screening for anemia (8, 9).
The intraoperative stage consists of 9 elements: (1) Preventing spinal anesthesia-induced hypotension; (2) maintaining normothermia; (3) administering uterotonic agents optimally; (4) administering antibiotic prophylaxis before skin incision; (5) providing prophylaxis for intraoperative and postoperative nausea and vomiting (IONV/PONV); (6) initiating multimodal analgesia using neuraxial long-acting opioids, epidural morphine, and non-opioid analgesia; (7) promoting breastfeeding and maternal-infant bonding through skin-to-skin contact; (8) optimizing intravenous fluid administration; and (9) practicing delayed umbilical cord clamping (8).
The postoperative stage consists of the following procedures: (1) Early oral intake, including ice chips and/or water up to 60 minutes post-delivery and a regular diet within 4 hours post-delivery; (2) Early mobilization, starting from sitting on the bed, progressing to sitting in a chair, and eventually walking or engaging in activity out of bed within 24-48 hours after delivery; (3) promotion of resting periods; (4) Early removal of urinary catheter 6-12 hours after delivery; (5) prophylaxis for venous thromboembolism (VTE); (6) facilitation of early discharge; (7) Remediation of anemia; (8) support for breastfeeding, including education and consultation; (9) Implementation of multimodal analgesia; (10) glycemic control; and (11) promotion of the return of bowel function. ERACS has shown promising results in improving the outcomes of standard C-section procedures. It can reduce postpartum pain and fatigue, promote early mobilization of the mother, and initiate breastfeeding earlier (8, 9). Mothers who experience ERACS have higher rates of breastfeeding compared to those who undergo standard C-sections (10, 11). However, the number of studies investigating the relationship between ERACS, vaginal delivery, and standard C-sections remains limited, particularly in Indonesia. Therefore, the aim of this study is to examine the relationship between ERACS and non-ERACS, as well as their impact on EBF and the early initiation of breastfeeding.
2. Objectives
The aim of this study is to examine the relationship between ERACS and non-ERACS, as well as their impact on EBF and the early initiation of breastfeeding.
3. Methods
This cross-sectional study involved 96 subjects in each category of delivery method. The research group was divided into ERACS and non-ERACS groups, with the non-ERACS group further divided into two categories: Vaginal delivery and standard C-section. The sample size for each group was determined using the formula for a cross-sectional study design. A desired power of 80% (Z
The assessment of the delivery method, EBF and early initiation of breastfeeding (EIBF) status, and subjects’ characteristics such as education level, occupation, parity, age, Body Mass Index (BMI), participation in pregnancy classes, and the number of antenatal and postnatal care visits was based on patient records in hospitals and home visit interviews with a questionnaire. The inclusion criteria included infants with APGAR scores ranging from 7 to 10, infants who experienced rooming-in, and infants with normal birthweights ranging from 2500 to 4000 grams. However, infants born to mothers with breast cancer, confirmed CMV and HIV infections, severe labor complications, and premature infants were excluded from the study.
Ethical approval was obtained from the Health Research Ethics Committee of the Faculty of Medicine at Jenderal Soedirman University (reference no.: 005/KEPK/PE/IX/2022). All legal guardians of the subjects provided their consent for participation. The success of EBF at 0, 1, 3, and 6 months was evaluated using a dedicated questionnaire with a Cronbach's Alpha value of 0.931, ensuring a reliability threshold of ≥ 0.60.
The relationship between ERACS and non-ERACS delivery methods and EBF and EIBF was analyzed using bivariate analysis through the chi-square test with a significance level of P < 0.05, and it is presented as the p-value and RR with 95% confidence interval (CI). Univariate analysis was conducted on the characteristics of the subjects using descriptive analysis and presented as frequencies in the form of sums and percentages.
4. Results
Characteristics of the subjects are presented in Table 1. In the ERACS group, the majority of mothers (53.1%) had tertiary educational backgrounds, whereas in the vaginal delivery and standard C-section groups, the majority had secondary educational backgrounds (61.5% and 49%, respectively). Across all delivery methods, the mothers primarily worked as housewives. The ERACS group consisted mostly of primiparous mothers (55.2%), while the vaginal delivery and standard C-section groups were predominantly multiparous (53.1% and 52.1%, respectively). Among all delivery methods, the majority of mothers were aged between 20-35 years, had a pre-pregnancy Body Mass Index (BMI) within the normal range, attended pregnancy classes, and had at least six antenatal care visits. Breastfeeding initiation procedures were most commonly observed among mothers in the ERACS and vaginal delivery groups (78.1% and 74%, respectively), whereas a smaller proportion of mothers in the standard C-section group did not undergo breastfeeding initiation procedures (58.3%).
| Characteristics | Delivery Method | P-Value | ||
|---|---|---|---|---|
| ERACS | Vaginal Delivery | Standard C-section | ||
| Mother’s education level | 0.199 | |||
| Elementary | 3 (3.1) | 7 (7.3) | 6 (6.3) | |
| Secondary | 42 (43.8) | 59 (61.5) | 47 (49) | |
| Tertiary | 51 (53.1) | 30 (31.3) | 43 (44.8) | |
| Mother’s occupation | 0.418 | |||
| Housewives | 55 (57.3) | 72 (75) | 67 (69.8) | |
| Working | 41 (42.7) | 24 (25) | 29 (30.2) | |
| Mother’s parity | 0.456 | |||
| Primipara | 53 (55.2) | 45 (46.9) | 46 (47.9) | |
| Multipara | 43 (44.8) | 51 (53.1) | 50 (52.1) | |
| Mother’s age | 0.141 | |||
| < 20 years old | 0 (0) | 1 (1) | 1 (1) | |
| 20 - 35 years old | 84 (87.5) | 83 (86.5) | 81 (84.4) | |
| > 35 years old | 12 (12.5) | 12 (12.5) | 14 (14.6) | |
| Mother’s BMI | 0.239 | |||
| Underweight | 12 (15,7) | 12 (12.5) | 16 (16.7) | |
| Normal | 68 (49) | 58 (60.4) | 50 (52.1) | |
| Overweight | 13 (13.5) | 21 (21.9) | 27 (28.1) | |
| Obese class I | 2 (15,7) | 5 (5.2) | 3 (3.1) | |
| Obese class II | 1 (9,8) | 0 (0) | 0 (0) | |
| Pregnancy class | 0.723 | |||
| Yes | 52 (54.2) | 49 (51) | 56 (58.3) | |
| No | 44 (45.8) | 47 (49) | 40 (41.7) | |
| Antenatal care | 0.314 | |||
| 6 times | 65 (67.7) | 65 (67.7) | 67 (69.8) | |
| < 6 times | 31 (32.3) | 31 (32.3) | 29 (30.2) | |
| Postnatal care | 0.097 | |||
| ≥4 | 70 (72.9) | 27 (28.1) | 57 (59.4) | |
| < 4 | 26 (27.1) | 69 (71.9) | 39 (40.6) | |
| Breastfeeding initiation | 0.111 | |||
| Yes | 75 (78.1) | 71 (74) | 40 (41.7) | |
| No | 21 (21.9) | 25 (23) | 56 (58.3) | |
| EBF | ||||
| 0 | 9 (9.4) | 1 (1) | 6 (6.3) | |
| 1 | 6 (6.3) | 6 (10.5) | 13 (13.5) | |
| 3 | 13 (13.5) | 25 (26) | 20 (20.8) | |
| 6 | 68 (70.8) | 64 (62.5) | 57 (59.4) | |
Characteristics of Subjects Based on Delivery Method a
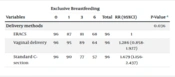
This study demonstrated a significant relationship between ERACS and non-ERACS deliveries and EBF at 0, 1, 3, and 6 months (P = 0.036). Compared to ERACS, vaginal delivery presented a RR of 1.286 (95% CI: 0.858 - 1.927) for not exclusively breastfeeding for 6 months, while standard C-section exhibited an RR of 1.679 (95% CI: 1.156 - 2.437) (Table 2).
| Variables | Exclusive Breastfeeding | Total | RR (95%CI) | P-Value a | |||
|---|---|---|---|---|---|---|---|
| Delivery methods | 0.036 | ||||||
| ERACS | 96 | 87 | 81 | 68 | 96 | 1 | |
| Vaginal delivery | 96 | 95 | 89 | 64 | 96 | 1.286 (0.858-1.927) | |
| Standard C-section | 96 | 90 | 77 | 57 | 96 | 1.679 (1.156-2.437) | |
Delivery Methods on Exclusive Breastfeeding (EIBF)
Additionally, the association between ERACS and non-ERACS deliveries and EIBF was statistically significant (P-value 0.000). Vaginal delivery had a RR of 1.190 (95% CI: 0.717 - 1.967) for not initiating breastfeeding within 1 hour of birth, while standard C-section had a higher RR of 2.667 (95% CI: 1.762 - 4.035) (Table 3).
| Variables | EIBF | Total | RR (95%CI) | P-Value a | |
|---|---|---|---|---|---|
| Delivery methods | 0.000 | ||||
| ERACS | 21 | 75 | 96 | 1 | |
| Vaginal Delivery | 25 | 71 | 96 | 1.190 (0.717-1.967) | |
| Standard C-section | 40 | 56 | 96 | 2.667 (1.762-4.035) | |
Delivery Methods on Exclusive Breastfeeding (EIBF)
5. Discussion
This study identified a significant association between ERACS and non-ERACS delivery methods with both EBF and EIBF. Mothers who underwent vaginal delivery were 1.286 times more likely to be at risk of not EBF for 6 months and 1.190 times more likely to be at risk of not EIBF compared to those who underwent ERACS. On the other hand, mothers who underwent a standard C-section had 1.679 times higher likelihood of not EBF for 6 months and 2.667 times higher likelihood of not EIBF compared to ERACS. These findings are consistent with a study conducted by Inano et al., which also reported a significant relationship between delivery method and exclusive breastfeeding (12). Similarly, Chiao et al. found that mothers who underwent ERACS had higher breastfeeding rates compared to those who had a standard C-section (11). Other studies conducted by Taha et al. and Finnie et al. reported lower rates of breastfeeding initiation in standard C-section compared to vaginal delivery (13, 14). It has been observed that a standard C-section can negatively impact long-term EBF due to disruptions in early breastfeeding behavior resulting from routine care after the surgery. C-section has been shown to delay breastfeeding initiation within the first hour after birth, as demonstrated by Zhang et al., who reported an average delay of 74.54 minutes (7). This aligns with the findings of this study that most mothers who underwent a C-section didn’t experience EIBF. One contributing factor to the negative association between a C-section and EBF is the extended recovery time experienced by mothers who undergo this procedure. The effects of anesthesia during a C-section can delay EIBF (5, 7). Additionally, post-surgical pain inhibits prolactin secretion due to the release of catecholamines, which further suppresses breast milk production. Fatigue, nausea, and vomiting following a C-section can also hinder EBF. Furthermore, C-sections can negatively impact maternal-infant bonding by delaying skin-to-skin contact (1, 5).
ERACS is an approach aimed at improving outcomes for standard C-sections. ERACS techniques reduce post-operative pain, shorten the recovery time from anesthesia, and increase maternal satisfaction (15). Pre-operative procedures in ERACS, such as providing education on early breastfeeding and managing breastfeeding-related concerns, better prepare mothers in the ERACS group for successful breastfeeding, thereby increasing the likelihood of EBF. Intra-operative measures, including the use of multimodal analgesics, facilitate post-operative pain reduction, breastfeeding initiation, and early skin-to-skin contact between mother and baby. These factors contribute to the formation of a strong bond between mother and baby and support the baby's adaptation to the outside world (15, 16).
Breastfeeding initiation within 1 hour of birth is particularly crucial for the success of EBF. The post-operative stage of the ERACS procedure further enhances the possibility of EBF. Early mobilization during this stage allows mothers to move more comfortably and facilitates breastfeeding. Additionally, breastfeeding support is provided throughout the hospital stay (8, 12).
There was no significant relationship found in this study between the mother's education level and exclusive breastfeeding. Cultural factors can influence EBF. Certain regions in Indonesia have cultural practices of introducing foods or beverages, like honey and mineral water, to infants from just a few days or weeks old (17).
A previous study conducted by Alzaheb reported a relationship between a mother's employment status and EBF, indicating that working mothers are less likely to exclusively breastfeed for up to 6 months. This can be attributed to the limited time working mothers have to spend with their babies and engage in breastfeeding, as they often have only a two-month maternity leave (18). However, in contrast to the findings of that study, the present study did not find a significant relationship between a mother's employment status and EBF.
Working mothers face challenges in maintaining their milk supply. The absence of breastfeeding support in the workplace, such as a private lactation space and dedicated break time for lactation, can further decrease the duration of EBF (19). However, an alternative solution for working mothers to sustain EBF is to express and store their milk. Chhetri et al. demonstrated that mothers who express and store their milk are more likely to maintain exclusive breastfeeding (20). Having knowledge about the importance of EBF and understanding proper techniques for expressing and storing breast milk can motivate working mothers to continue practicing EBF even while employed (21).
Most mothers practicing EBF were multiparous in this study, although it wasn’t statistically significant. The previous experience of breastfeeding can enhance confidence in multiparous mothers (22, 23). However, the association with EBF is influenced by other covariates, particularly in primiparous mothers, such as age, level of education, and breastfeeding-related information (20). Kitano et al. discovered that mothers under the age of 35 were more likely to succeed in EBF at discharge and at 1 month, regardless of whether they were primiparous or multiparous (24). This finding contrasts with research conducted by Silva et al., which suggested that older mothers were more likely to breastfeed due to their prior breastfeeding experience, while younger mothers faced insecurities regarding breastfeeding (25).
In this study, no significant relationship was found between maternal pre-pregnancy BMI and EBF. However, a study reported that as BMI increases, the risk of EBF failure also increases due to various factors associated with BMI. These factors include hormonal states that can cause delays in lactation, a diminished response of prolactin, and insecurities related to body image. The study found that women across all obesity classes were more likely to use formula compared to women with a normal pre-pregnancy BMI, and obese mothers had a 2.86 times greater risk of breastfeeding initiation failure (26).
A study conducted by Tseng et al. made a comparison between mothers who received an intervention in the form of an integrated breastfeeding class and mothers who did not receive any intervention. It revealed that the intervention group had a higher rate of EBF for 6 months (EBF-6) and were 2.82 times more likely to have EBF for the full duration. The mothers who received interactive education about breastfeeding exhibited a positive attitude towards breastfeeding and increased confidence in their ability to breastfeed, leading to a higher success rate of EBF (27). These results align with the findings of the present study, which also demonstrated that mothers who attended pregnancy classes had a higher rate of EBF-6 compared to mothers who did not attend such classes.
Antenatal care (ANC) visits have been identified as a significant factor influencing the success of EBF. Inadequate ANC visits have been associated with a higher likelihood of EBF failure (28). Research indicates that having ANC visits at least 4 times increases the chances of achieving EBF by 1.9 times compared to those with fewer than 4 ANC visits (29). Moreover, another study revealed that mothers who attended at least 1 ANC visit were 70% more likely to initiate breastfeeding within 1 hour after birth and 2.24 times more likely to exclusively breastfeed compared to those with no ANC visits.
Postnatal care (PNC) also plays a crucial role in promoting EBF. Mothers who attended at least 1 PNC visit were 86% more likely to breastfeed. Education provided during ANC and PNC visits contributes to developing positive attitudes, beliefs, and decisions regarding EBF. PNC visits further assist in addressing potential breastfeeding issues and facilitate increased family support for EBF (29).
5.1. Conclusions
In conclusion, this study demonstrates a significant relationship between ERACS and non-ERACS delivery methods with EBF and EIBF, with ERACS promoting better rates compared to vaginal delivery and standard C-section. We suggest implementing ERACS, especially in mothers planning for C-sections. However, this study is not without limitations, and further research is recommended using a cohort study design, as this preliminary study employs a cross-sectional design.