1. Background
Pediatric feeding disorder is characterized by difficulties in age-appropriate oral intake due to medical, feeding skills, psychosocial, and nutritional factors (1). Swallowing disorder, or oropharyngeal dysphagia, a subset of feeding disorder, is defined as problems in the movement of food from the mouth to the stomach (2). Challenges in feeding and swallowing can lead to severe nutritional and developmental issues and even mortality (3). Successful swallowing requires proper skeletal-muscular tone, oral sensory-motor function, and a healthy swallowing process, all of which are influenced by psychosocial and cultural aspects (3). Therefore, children with neurological conditions such as cerebral palsy (CP) are at a high risk of developing feeding and swallowing disorders (4). Reports indicate a prevalence of 25% to 45% for these disorders in typically developing children, while children with CP have a higher prevalence ranging from 70% to 80% (5).
However, studies differ in their findings regarding the prevalence of feeding disorders. Variations in the prevalence of feeding disorders across studies can stem from diverse historical definitions (1), participant ages, assessment methods, and diagnostic tools. Cultural and psychosocial factors also impact results, such as the absence of chewable foods affecting later chewing problems (3).
Examining the prevalence of feeding and swallowing issues in children with CP in Iran, a developing country with its own cultural and socioeconomic context, can inform health policy and the provision of appropriate services for children with CP.
2. Objectives
This study aimed to assess these issues in Iranian CP children and explore links between swallowing severity, CP type, age, nutrition, gastroesophageal reflux disorder (GERD), intellectual disability, socioeconomic status, caregiver concerns, motor function limitations, and limb involvement.
3. Methods
In this analytical cross-sectional study, 111 children with an average age of 8 years participated through convenience sampling. These children were referred for occupational therapy at public and private centers in Tehran, Mashhad, and Semnan. The inclusion criteria were an age range of 3 - 18 years and a diagnosis of CP by a neurologist. Exclusion criteria were progressive neurological or muscular disorders and lack of cooperation. All participants had parental consent. The study occurred in autumn 2021. To reduce selection and information bias, we included various types and severities of CP and used formal assessments.
The primary caregiver provided demographic, medical, and developmental data, including issues related to GERD, interaction problems, food refusal/restriction, and common food textures. An occupational therapist categorized children's motor issues using the GMFCS, ranging from level 1 (balance and coordination limitations) to level 5 (severe restrictions in head, trunk, and limb movement).
A speech therapist assessed swallowing severity using the eating and drinking ability classification system (EDACS) after interviewing caregivers and conducting observations with the dysphagia disorder survey (DDS) (6). Eating and drinking ability classification system evaluates swallowing function based on efficiency and safety, ranging from level 1 (safe and efficient) to level 5 (high aspiration risk, potentially requiring tube feeding) (7). The Persian version of EDACS has shown good validity and reliability, with an α-Cronbach of 0.98 (8).
An expert physician used the Subjective Global Nutrition Assessment (SGNA) to evaluate undernourishment severity, scaling from 0 (no issue) to 2 (severe problem) (9). Subjective Global Nutrition Assessment is a reliable tool in CP (10) and is based on a patient's history and physical examinations to identify patients at risk of malnutrition. In Iran, SGNA showed moderate correlation with objective assessment (r = 0.37), offering quick and comprehensive screening (11). To test EDACS and SGNA reliability, a different examiner independently scored videos of 30 children in this study. Inter-rater reliability for EDACS and SGNA was strong, with r = 0.78 and r = 0.85, respectively (P ≤ 0.001). A psychologist evaluated participants' intelligence quotient (IQ) through assessment or school entrance IQ test results. Caregiver concerns were measured through the concern subtest of the Feeding/Swallowing Impact Survey (FS-IS), comprising seven Likert-Scale questions with scores ranging from 7 to 35 (12), showing strong validity and reliability in Persian, with an α-Cronbach of 0.95 (13).
Data were analyzed using IBM SPSS version 20. Descriptive statistics were utilized to present descriptive information. Chi-square and Spearman's correlation coefficient tests were employed to examine the relationship between the severity of swallowing disorders and the studied factors. The inter-rater reliability of SGNA and EDACS tests was evaluated using the Kendall correlation coefficient test. A significance level of P < 0.05 was set to determine statistical significance.
For sample size calculation, the formula n = Z2 × P (1-P)/d2 was utilized. With an expected prevalence of 0.53 based on previous studies (6) and a precision of 10%, the sample size was determined to be 99.
4. Results
Out of the 117 children initially invited, two did not meet the inclusion criteria, and four declined to participate. Therefore, 111 children with a median age of 7 (IQR: 5, 11) underwent evaluation for motor function, feeding/swallowing, and nutritional status. (Table 1 outlines participant characteristics). Swallowing disorders were prevalent in 78.38% (95% CI: 69.56, 85.63), with 87 cases identified. The prevalence of feeding disorders (79.28%, 95% CI: 70.55, 86.39) included one child with avoidant/restrictive food intake (ARFID) only. Severe swallowing issues involving the pharyngeal phase affected 45 children (40.54%, 95% CI: 31.32, 50.28), and 14 participants (12.61%, 95% CI: 7.07, 20.26) exhibited unsafe swallowing (EDACS = 4 and 5). However, only 3 children (2.7%, 95% CI: 0.5, 7.7) used tube feeding, with one being entirely dependent and two using it as a supplement.
| Variables | Mean (SD) | Min-Max |
|---|---|---|
| Age (y) | 8.3 (3.9) | 2 - 18 |
| Gestational age (mo.) | 8.4 (0.74) | 7 - 9 |
| FSIS (Caregiver’s concern score) | 16.13 (8.38) | 7 - 34 |
| Gender | ||
| Boy | 75 | 67.6 |
| Girl | 36 | 32.4 |
| GMFCS a | ||
| 1 | 10 | 9 |
| 2 | 20 | 18 |
| 3 | 45 | 40.5 |
| 4 | 24 | 21.6 |
| 5 | 12 | 10.9 |
| CP type | ||
| Spastic | 87 | 78.3 |
| Ataxic | 9 | 8.1 |
| Dyskinetic | 10 | 9 |
| Mixed | 5 | 4.6 |
| Concomitant problems | ||
| Drooling | 16 | 14.4 |
| Seizure | 19 | 17.1 |
| GERD b | 21 | 19 |
| ID c | 45 | 40.5 |
| EDACS d | ||
| 1 | 24 | 21.6 |
| 2 | 42 | 37.9 |
| 3 | 31 | 27.9 |
| 4 | 9 | 8.1 |
| 5 | 5 | 4.5 |
| Feeding | ||
| Oral | 108 | 97 |
| Tube | 1 | 1 |
| Tube and oral | 2 | 2 |
| Malnutrition (SGNA resulte) | ||
| Moderate | 47 | 42.3 |
| Severe | 19 | 17.1 |
| total | 66 | 59.4 |
Abbreviation: CP, cerebral palsy.
a Gross Motor Function Classification System.
b Gastrointestinal Reflux Disorder.
c Intellectual Disability.
d Eating and Drinking Ability Classification System.
e Subjective Global Nutrition Assessment.
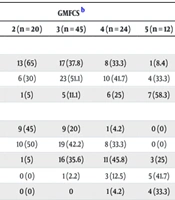
Table 2 demonstrates subgroup analysis findings: Prevalence of swallowing disorders was 82.3% (95% CI: 72.57, 89.77) in children with spastic CP (70 cases), 54.5% (95% CI: 23.38, 83.25) in those with ataxic CP (6 cases), 70% (95% CI: 34.75, 98.4) in those with hyperkinetic CP (7 cases), and 80% (95% CI: 28.36, 99.49) in those with mixed CP (4 cases). Swallowing disorder rates based on the GMFCS level were as follows: 100% (95% CI: 73.53, 100) at level 5, 95.8% (95% CI: 78.88, 99.89) at level 4, 80% (95% CI: 65.4, 90.42) at level 3, 55% (95% CI: 31.53, 76.94) at level 2, and 50% (95% CI: 18.71, 81.29) at level 1. Malnutrition (SGNA = 1 and 2) was present in 67 children (60.4%, 95% CI: 50.63, 69.52), with 26 participants (23.4%, 95% CI: 27.14, 51.5) receiving dietary supplements.
Further analysis revealed no significant difference in swallowing disorder severity by EDACS (P = 0.45) or malnutrition by SGNA (P = 0.22) across different types of CP. However, there was a significant association between GMFCS-based mobility limitations and malnutrition (P = 0.001), with higher levels of movement severity correlating with increased rates of malnutrition. Additionally, a significant correlation was found between the severity of swallowing disorders and mobility limitations, with greater mobility issues being linked to more severe swallowing problems (P ≤ 0.001).
| Variables | CP type | GMFCS b | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Spastic (n = 85) | Ataxic (n = 11) | Hyper-kinetic (n = 10) | Mixed (n = 5) | 1 (n = 10) | 2 (n = 20) | 3 (n = 45) | 4 (n = 24) | 5 (n = 12) | |
| SGNA b | |||||||||
| 0 | 32 (37.7) | 7 (63.3) | 5 (50) | 0 (0) | 5 (50) | 13 (65) | 17 (37.8) | 8 (33.3) | 1 (8.4) |
| 1 | 37 (43.5) | 4 (36.7) | 4 (40) | 3 | 5 (50) | 6 (30) | 23 (51.1) | 10 (41.7) | 4 (33.3) |
| 2 | 16 (18.8) | 0 (0) | 1 (10) | 2 | 0 (0) | 1 (5) | 5 (11.1) | 6 (25) | 7 (58.3) |
| EDACS c | |||||||||
| 1 | 15 (17.6) | 5 (45.5) | 3 (30) | 1 | 5 (50) | 9 (45) | 9 (20) | 1 (4.2) | 0 (0) |
| 2 | 32 (37.7) | 4 (36.7) | 5 (50) | 1 | 5 (50) | 10 (50) | 19 (42.2) | 8 (33.3) | 0 (0) |
| 3 | 25 (29.4) | 2 (18.8) | 2 | 2 | 0 (0) | 1 (5) | 16 (35.6) | 11 (45.8) | 3 (25) |
| 4 | 9 (10.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2.2) | 3 (12.5) | 5 (41.7) |
| 5 | 4 (4.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 | 1 (4.2) | 4 (33.3) |
Abbreviations: CP, cerebral palsy.
a Gross Motor Function Classification System.
b Eating and drinking ability classification system.
c Subjective global nutrition assessment.
Examining the correlation between swallowing disorder severity and various factors revealed no significant difference across CP types (P = 0.45) or based on the presence of intellectual disability (P = 0.1). However, children with GERD exhibited significantly more severe swallowing issues (P = 0.007). Table 3 outlines the correlation between swallowing disorder severity and the investigated variables. A notable positive correlation was found between EDACS and caregiver concern (r = 0.77). Additionally, EDACS displayed moderate positive correlations with GMFCS (r = 0.65), the number of limbs affected in spastic CP (r = 0.55), and malnutrition (r = 0.5). No significant link, however, emerged between EDACS and the child's age.
a Gross Motor Function Classification System.
b Subjective Global Nutrition Assessment.
c Socioeconomic Status.
5. Discussion
In this study, the prevalence of feeding and swallowing disorders in children with CP was estimated at approximately 79% and 78%, respectively, which is higher than previously reported rates. Erkin et al. reported lower prevalence rates of 19.2% for swallowing difficulties and 21.7% for feeding issues (14), while Garcia Ron et al. found a 43% prevalence of swallowing problems (15). Costa et al. and Calis et al. reported higher prevalence rates of swallowing disorders in school-age children (100%) and those with severe CP (99%), respectively (16, 17). Speyer et al.'s systematic review estimated prevalence rates of 50.4% for swallowing disorders and 53.5% for feeding disorders (18), but noted discrepancies based on parental reports. Excluding parental reports, prevalence was higher at 68.4% in the remaining studies (18). Furthermore, all studies under review in their study were conducted in developed countries. Benfer et al. reported a higher prevalence of 85% for these disorders in their participants aged 18-36 months (4). The high prevalence of swallowing disorders in younger children could be related to developmental delays and incomplete feeding skills in children up to 3 years old (3).
Comparing the prevalence of swallowing disorders between Australia, a developed country, and Bangladesh, a developing one, Benfer et al. found higher rates in Bangladesh (68.1%) compared to Australia (58.5%), which they attributed to more severe motor impairments in developing countries. After adjusting for the GMFCS of participants, the proportion was equal in both countries (19). Therefore, the higher prevalence of swallowing disorders in low-resource countries compared to developed countries may be attributed to more severe motor impairments. Our study also observed limited participants with mild motor issues, which may be related to sampling during the COVID-19 pandemic. The fear of the disease and economic factors could have contributed to the limited referral of children with mild motor problems to clinics, affecting the study's prevalence findings.
The influence of economic, educational, and cultural factors on feeding and swallowing disorder prevalence is crucial. In developing countries, limited experts in the field of feeding and swallowing disorders can cause delays in accessing treatment, affecting disorder severity. Research on these disorders in developing countries is limited. Chidomere's African study reported a 39.1% prevalence of feeding issues in children with CP (20), possibly due to reliance on parental reports. Parents might underestimate issues in severe CP cases due to adaptation or lower expectations for those with severe CP. Another study in Africa estimated a 55% prevalence of swallowing disorders in children (21). An Indian study found feeding problems in all 100 children aged 1 - 9 (22). In Turkey, a study with a more similar culture and comparable age range to ours, reported a 73.8% prevalence of swallowing disorders in children with CP (23), consistent with the findings of our study.
In our study, 40.54% of participants had issues in the pharyngeal phase of swallowing, which is lower than the 61.7% reported by Benfer et al., possibly due to their younger participants and the age-related decrease in problems (24). All children with GMFCS level 5 had swallowing disorders, with prevalence decreasing as motor issues became less severe, aligning with the findings of Benfer et al. (4). No significant difference in oral-pharyngeal swallowing disorders among CP types was found, similar to the findings of Benfer et al. (4). Children with GERD tended to show more severe swallowing problems, despite limited evidence linking GERD with pediatric feeding disorders (1).
Another objective of this research was to examine the relationship between the severity of swallowing difficulties and certain variables. Swallowing problem severity increased with motor problem severity, which is consistent with previous studies (4, 15, 17, 20, 25, 26), possibly due to the role of trunk and neck muscle stability in safe swallowing (27). A moderate positive correlation existed between swallowing disorder severity and malnutrition, consistent with previous findings (15, 28, 29) and contrary to the results of studies conducted by Chidomere et al. and Calis et al. (17, 20). Caregiver concern and swallowing disorder severity showed a moderate positive correlation, which differs from Benfer et al.'s discovery of no correlation (24). Nevertheless, inappropriate feeding is a major concern for caregivers, impacting parents' anxiety and quality of life (13, 30-33).
In our study, malnutrition affected over half of the children, which is higher than the estimated 40% prevalence (34). Only one-third of the participants used dietary supplements, and a small percentage used tube feeding. In comparison, Calis et al. reported that 32.5% of cases used tube feeding (17). Dahlseng et al. found varying tube feeding rates across European countries, with Sweden having the highest at 22% and Portugal the lowest at 3% (35). Benfer et al. noted that 12.3% of Australian children with CP were on tube feeding, while no children in Bangladesh were tube fed, potentially contributing to higher underweight rates there (19). Prolonged gastric tube use is linked to weight gain (35). In Iran, 48% of children with CP were underweight, with 64% not receiving enough calories and supplements (36). Socioeconomic status can impact nutritional deficiencies (34). Therefore, raising awareness among Iranian caregivers about the importance of weight gain, alongside financial support, can enhance the utilization of supplements and tube feeding.
This study, involving a large sample size of both genders from private and public clinics, has limitations, such as convenience sampling and the absence of a typical children control group, affecting external validity. Thus, cautious interpretation of the findings is necessary, highlighting the need to address these limitations in future research.
5.1. Conclusions
Feeding and swallowing issues, along with malnutrition, are prevalent in Iranian children with CP. While the severity of swallowing problems correlates with malnutrition, the use of supplements and tube feeding remains limited. Early multidisciplinary referral for feeding and swallowing issues is critical for optimal care.