1. Background
Fever is frequently observed in the pediatric age group as the first sign of illness. It is a significant reason for hospital admissions and also causes anxiety in families. Decisions regarding hospital admissions, diagnostic tests, or treatment protocols often depend on the presence of fever (1, 2). Therefore, families must be able to determine body temperature practically and accurately.
Body temperature can be measured in various ways, traditionally using contact thermometers placed in the ear, armpit, or rectum (3). Although rectal thermometry has been the most reliable method, it is not preferred today due to mercury toxicity and difficulties in use (4, 5). Traditional thermometers have been replaced by more modern devices over time. Non-contact thermometers are easy to use and do not have the risk of infection as they measure without touching anybody surfaces (6). The main types of non-contact thermometers are non-contact infrared thermometers (NCITs), tympanic thermometers, and thermal scanners (3). The NCIT was approved in 2004 by the U.S. Food and Drug Administration (FDA). Non-contact forehead infrared thermometers use infrared technology to detect the heat radiated from the skin surface over the temporal artery, which receives blood from the carotid artery. This method reflects the core body temperature and offers advantages, including quick results, simple use, no risk of cross-infection, and no discomfort for children (7-9).
With technological developments, many tools that make our lives easier in different fields have become indispensable in daily use. Smartphones, widely used today, offer applications in many different fields apart from communication. One such application is an smart mobile phone thermometer (SMT), which works by attaching to a smartphone and is designed to measure body temperature from the forehead, offering practical ease of use. The thermometer can measure between 32 - 42°C, with the accuracy and precision of the device being within ±0.2°C (10).
There are debates in the literature about what value can be considered a fever in NCIT measurements, with significant differences reported between these devices (11, 12).
2. Objectives
In the present study, we aimed to compare the SMT with non-contact forehead infrared thermometer (NCFIT) and investigate whether we can recommend this device, which is easy to use and carry, to our pediatric patients for daily use. To our knowledge, this is the first study to evaluate SMT accuracy and performance in the literature.
3. Methods
Patients admitted to the Emergency Department of the University of Health Sciences, Zeynep Kamil Maternity and Children’s Hospital between June 2023 and July 2023 were included in this prospective study. Newborns, patients in the red triage group (those needing resuscitation, showing signs of shock, convulsions, respiratory failure, etc.), and children whose parents did not give consent were excluded. Measurements were not taken from patients who were sweaty or had been exposed to the sun for an extended period. Our hospital is one of the largest children's hospitals on the Anatolian side of Istanbul and is a tertiary center that provides specialist training in pediatrics. During the study period, the average number of pediatric emergency admissions in 24 hours was between 300 - 400 patients.
Based on the CDC guideline "general instructions: How to use an infrared thermometer," a temperature ≥ 38°C is considered a fever (6). Additionally, a cut-off value of ≥ 36.65°C from the study by Lai et al. and a cut-off value of ≥ 37.5°C were taken for comparison (11).
All measurements were made by the same nurse, who was trained for each instrument, in the same triage room repeatedly. All temperature measurements were done on the Celsius (°C) scale. Body temperature measurements were performed on the mid-forehead with an NCFIT (model: VZN FI03, measuring range 32.0°C - 42.9°C) and an SMT (model: USB K8 infrared smart mobile phone thermometer, measuring range 32.0°C - 42.0°C, Shenzhen, China) (Figure 1). Thermometers were used according to the manufacturer’s instructions. Non-contact forehead infrared thermometer was positioned 3 - 5 cm from the center of the forehead, while SMT was positioned approximately 2 and 8 cm from the center of the forehead. The measurement of the nurse's finger width, who made the measurement, was used as a reference for adjusting the distances since the same nurse performed the measurements. According to the manufacturer's instructions, the SMT can measure body temperature from a distance of 1 - 10 cm. Two different measurements were made to see if there was a change in the measurement when the distance changed. The body temperature, sex, and age of the children were recorded.
Approval for the study was obtained from the local ethics committee of the University of Health Sciences, Zeynep Kamil Maternity and Children’s Hospital (June 2023-94). All participants' parents provided written informed consent for their inclusion in the study.
3.1. Statistical Analysis
Statistical analysis was performed using SPSS version 22 (IBM SPSS Statistics, Chicago, IL). Data were expressed as numbers, percentages, and mean ± standard deviation, as needed. The distribution of variables was examined using the Shapiro-Wilk normality test. Paired samples t-tests were used to compare continuous variables. Correlation analysis for continuous variables (e.g., measurements of thermometers) was conducted using Pearson’s analysis. The children with and without fever were examined using ROC and AUC. The sensitivity, specificity, and cut-off values for SMT were determined. For all analyses, results were evaluated at a significance level of P < 0.05.
4. Results
A total of 1116 children were included in this prospective study. The median age was 4 years (ranging from 32 days to 18 years), and 585 (52.4%) were male. The body temperatures of all patients were measured from a distance of 3 - 5 cm with the NCFIT and from a distance of 2 cm with the SMT. Additionally, the body temperature of 1067 patients was measured with the SMT from a distance of 8 cm.
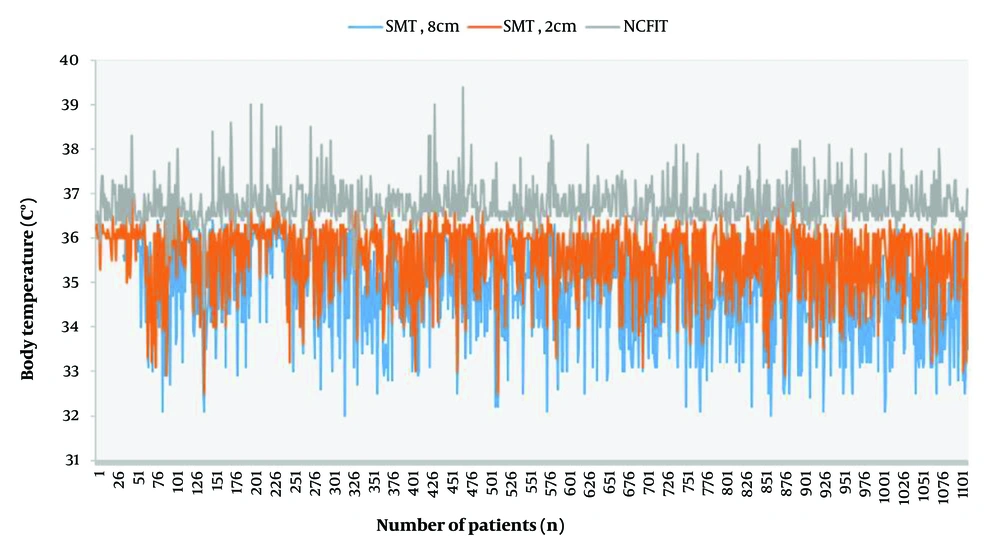
The measurements taken with the NCFIT were higher than those taken with the SMT at both 2 cm and 8 cm distances. The mean difference between the NCFIT and SMT (2 cm) measurements was 1.2°C. As the distance increased, the measurements decreased (Figure 2, Table 1).
| Variables | Minimum | Maximum | Mean ± Standard Deviation |
|---|---|---|---|
| NCFIT (n: 1116) | 34.4 | 39.4 | 36.7 ± 0.4 |
| SMT (2 cm) (n: 1116) | 32.5 | 37.6 | 35.5 ± 0.7 |
| SMT (8 cm) (n: 1067) | 32 | 37 | 34.8 ± 1 |
Abbreviations: NCFIT, non-contact forehead infrared thermometer; SMT, smart mobile phone thermometer.
The comparison of all the measurements was significantly different (Table 2) (P < 0.05). No difference in measurements was detected based on age or sex for all three methods. Although all three measurements were statistically significantly correlated, the correlation between the NCFIT and SMT readings at both 2 cm and 8 cm distances was weak, with r = 0.38 and r = 0.34, respectively (P < 0.01). The measurements of the SMT from distances of 2 cm and 8 cm were more strongly correlated with each other (r = 0.65, P < 0.01).
| Variables | t | 95% Confidence Interval of the Difference | P-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| NCFIT/SMT (2 cm) (n: 1116) | 52.7 | 1.12 | 1.21 | < 0.01 |
| NCFIT/SMT (8 cm) (n: 1067) | 63.5 | 1.89 | 2.01 | < 0.01 |
| SMT (2 cm /8 cm) (n: 1067) | -30.8 | -0.81 | -0.71 | < 0.01 |
Abbreviations: NCFIT, non-contact forehead infrared thermometer; SMT, smart mobile phone thermometer.
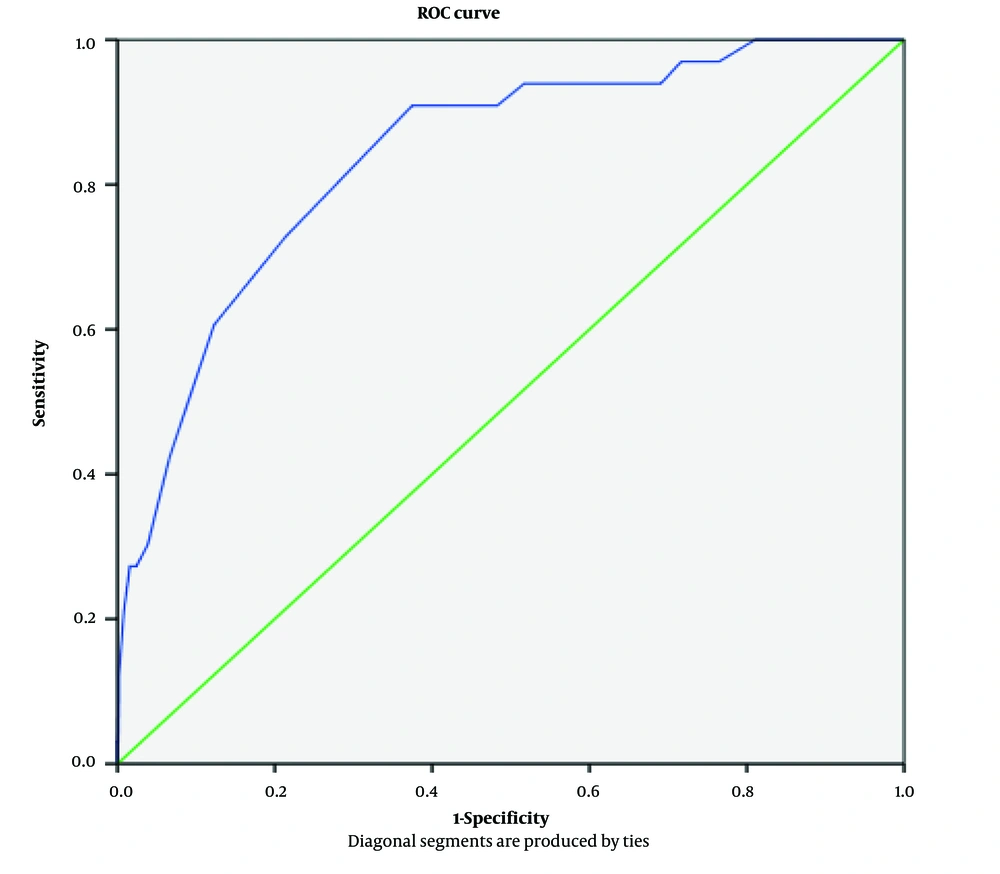
There were 33 children with fever, defined as a body temperature of ≥ 38°C measured by NCFIT. The mean measurements in these children with fever were 38.2 ± 0.3°C for NCFIT, 36.3 ± 0.5°C for SMT at 2 cm, and 35.8 ± 0.9°C for SMT at 8 cm (P < 0.01). The SMT was not able to detect any body temperature ≥ 38°C. The device's description of giving an alarm at 37.4°C could not be demonstrated. For fever detection, we set the value of 38°C as the limit for NCFIT and tried to determine a threshold for the SMT to be considered as fever. Based on these results, the cut-off value for SMT was calculated, and the area under the ROC curve was 0.84 (0.77 - 0.90), which was above the desired limit value of 0.70 (Figure 3). The cut-off value for SMT in patients with fever (body temperature ≥ 38°C by NCFIT) was determined to be 36.15°C, which had a sensitivity of 72% and a specificity of 78%. When the value for fever was taken as 36.65°C, NCFIT detected fever in 545 patients, while SMT detected fever in 26 patients. When the value was taken as 37.5°C, NCFIT detected fever in 68 patients, while SMT detected fever in only one patient (area under the ROC curve was 0.66). Additionally, the cut-off value for SMT to detect patients with body temperature ≥ 37.5°C by NCFIT was 35.95°C, with a sensitivity of 71.4% and a specificity of 51% (Table 3).
| Cut-off Value °C for SMT | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Fever set at ≥ 38°C with NCFIT | ||
| 36.06 | 90.9 | 62.5 |
| 36.15 | 72.7 | 78.7 |
| Fever set at ≥ 37.5°C with NCFIT | ||
| 35.75 | 85.7 | 44 |
| 35.85 | 78.6 | 48 |
| 35.95 | 71.4 | 51 |
| 36 | 64 | 62 |
Abbreviations: NCFIT, non-contact forehead infrared thermometer; SMT, smart mobile phone thermometer.
5. Discussion
Smartphones are being increasingly used for medical information documentation due to their multifunctionality (13). The SMT is designed to provide ease of use and portability. In our study, we aimed to compare body temperature measurements between the SMT and the NCFIT to determine whether the SMT can be used accurately in children. We found that the mean body temperatures obtained from the NCFIT were significantly higher than those from the SMT when compared using the paired t-test. The mean difference between the NCFIT and SMT (2 cm near) measurements was 1.2°C. As the distance increased, the measurements decreased, and the difference became 1.5°C. According to our study, the mean difference between the NCFIT and SMT was greater than 1°C. This exceeds the commonly accepted limits of agreement of ±0.5°C (7, 9). Infrared thermometers tend to have decreasing accuracy as the distance increases. Factors that may contribute to this include the angular field of the infrared thermal imager, the difference between body temperature and ambient temperature, and atmospheric transmittance (14, 15).
Using non-contact thermometers is one of the most common methods today, as we do in our daily practice in the emergency room. Although NCITs are frequently used and gained popularity during the COVID-19 pandemic due to their lack of infection risk and rapid scanning capability, clinical studies have reported varying results regarding their accuracy (9, 16). During the pandemic, Chen et al. performed a prospective observational study comparing the accuracy of forehead and wrist temperature measurements with tympanic temperature, defining fever as a tympanic temperature of ≥ 37.3°C. The mean difference in forehead measurements ranged from -1.72 to -0.56°C. The cut-off value for the forehead measurement for detecting a tympanic temperature of ≥ 37.3°C was 36.2°C, with 93.2% sensitivity and 60.0% specificity (16). In our study, there were 33 children with fever, but none were detected by the SMT. The cut-off value for SMT in patients with fever (≥ 38°C by NCFIT) was determined to be 36.15°C, which had a sensitivity of 72% and a specificity of 78%.
In the literature, previous studies show that NCFITs record temperatures lower than those recorded using infrared tympanic thermometers (IRTTs) (8). In a study by Kim et al., the temperature measured using the NCFIT was 0.14°C lower than that using the IRTT in children aged under 18 years (8). In the Hamilton et al. study, which included 205 pediatric patients, NCFIT febrile measurements were compared to a reference oral or rectal reading. The mean NCFIT measurements were 0.42°C lower than the reference value (17). Another study involving 1113 adults compared six NCFITs with a reference thermometer, and the majority of the differences ranged from -2 to +1°C, while in extreme cases, the error ranged from -3 to +2°C, which is outside the laboratory accuracy zone of ±0.3°C. Nearly half of the clinical measurements fell outside of the manufacturer’s accuracy claim for all models, and the difference between the reference temperature and NCIT temperature was statistically significant (12). In our study, the mean difference between the NCFIT and SMT (2 cm near) measurements was 1.2°C.
Non-contact forehead infrared thermometer measurements show variability between studies. Several factors affect the accuracy of the temperature measured by NCFITs. Firstly, the inaccuracy of the sensor may lead to different measurements. Secondly, NCFITs measure body temperature by detecting infrared radiant energy from the forehead skin surface, which is lower than the reference body sites. Manufacturers use specific algorithms and hardware to compensate for this difference. Software errors in the device can also cause inaccuracy. Lastly, user errors (incorrect distance or angle) and unsuitable skin surfaces (sweating, exposure to the sun) may cause inconsistent results (8, 12). In our study, although the measurement was made by the same nurse from a distance of 2 - 8 cm with a smartphone, which is in accordance with the user's manual of the device, results were significantly different from the measurements made with NCFIT, which is frequently used in our emergency department. Additionally, no child with fever was detected with SMT. The fact that the environmental conditions were the same and the measurements were performed by the same trained person suggests that the difference in the measurements between the two devices was due to sensor error or software algorithm failure.
Body temperature measurements vary depending on the location; a difference of 0.4°C exists between rectal and oral readings, while a difference of 0.7°C exists between rectal and axillary readings. The Canadian Pediatric Society has stated that a normal temperature range for a rectal reading is between 36.6°C and 37.9°C, while a normal temperature range for an armpit reading is between 36.5°C and 37.5°C. Any temperature above this range is considered a fever (18). Additionally, the American Academy of Pediatrics (AAP) defines fever as a rectal temperature of ≥ 38°C. There is no authoritative data for the cut-off point for fever obtained using NCFITs (11). According to the CDC guideline "general instructions: How to use an infrared thermometer," a temperature ≥ 38°C is considered a fever (6). The Hong Kong Government’s threshold level for fever is 36.0°C for NCFITs (19). The Canadian Pediatric Society does not specify any range for forehead measurement and there are no recommendations regarding measurement here (18). Lai et al. suggested that the optimal fever diagnostic threshold for forehead temperature is 36.65°C (11). Yazar and Türe stated that the best threshold for NCFIT was > 37.3°C for determining a tympanic temperature of > 38°C (20). In our study, different cut-off values were used and it was observed that when the cut-off value for fever was lowered, the devices detected more febrile pediatric patients. Health authorities opine that NCFITs should only be used for screening purposes and not for accurate evaluation (19).
The most important limitation of our study is that the measurements were not compared with a reference method as we did not have a true measure of core body temperature. The most reliable temperature measurement is obtained by invasive methods, but this is not practical in daily practice. The fact that the study was conducted in a single center and included only pediatric patients means the results cannot be attributed to the general population. No comments can be made regarding the use of the device in adults. The cut-off value for fever was taken as 38°C; if this value were taken lower in line with recommendations from other studies, it would be seen that the device would be more effective in detecting fever. However, it does not change the fact that there is a statistical difference in the measurements between the two devices. Another limitation of the study is that the ambient temperature and humidity levels were not included in the study, but the measurements of both devices were made in the same room and immediately after each other, suggesting that the difference between the two devices cannot be attributed to these factors. Additionally, another influencing factor, circadian rhythm, was not included in the study design.
While using NCFIT, the device should point directly at the center of the person’s forehead and not at an angle. Especially in infancy, it is possible that the patient may move during the measurement, which can affect the accuracy of the readings.
Everyone has a smartphone, and measuring body temperature with equipment compatible with the device will provide convenience. Additionally, tracking these measurements via phone applications will facilitate patient follow-up because many families cannot provide accurate fever-related anamnesis in pediatric clinics. However, our study data show that any measurement obtained from SMT should be viewed with suspicion. Each device should have its own cut-off value and be used accordingly; it is not appropriate to take a standard measurement. Nevertheless, the fact that the measurements in the SMT device are consistent within themselves raises the possibility of using this device in clinical settings for families to detect deviations in their children's baseline measurements, follow-up for antipyretic usage, and monitoring different fever levels.
To our knowledge, this is the first study on temperature measurement via SMT in pediatric patients. Our study had a large population, as data was collected at one of the largest children’s hospitals in İstanbul. The results demonstrated that the SMT has low sensitivity and specificity in detecting fever and is not a good option for use in pediatric patients.