1. Background
Traumatic injuries are a leading cause of visits to pediatric emergency departments (PEDs) in the United States, accounting for approximately one-third of all PED visits by children and adolescents (1).
Recent data indicate that pediatric trauma is also a significant public health issue in Europe, with road traffic accidents as the leading cause of injury and death among children. A study in Portugal revealed that over the past decade, the absolute number of major pediatric trauma cases has not decreased, with falls from height accounting for 19% of injuries and sports activities for 4%. Additionally, head and neck injuries were present in 73% of cases, underscoring the need for improved prevention strategies to address this persistent challenge (2).
Many of these visits involve minor trauma, often leading to imaging studies, particularly for limb injuries. Considering the lifetime fracture risk of 27 - 40% for girls and 42 - 64% for boys aged 0 - 16, early detection of bone injuries is critical (3). However, young children, especially toddlers, may find it difficult to localize their pain. They may adopt unusual postures or cry during examinations, regardless of the severity or location of the injury (4).
Diagnostic imaging, primarily X-rays, plays a key role in managing musculoskeletal trauma (5). While X-rays are commonly used, negative results sometimes necessitate additional views to definitively rule out fractures. Unnecessary radiation exposure in children poses significant risks, as they are more sensitive to ionizing radiation than adults. Studies show that even low doses of radiation can significantly increase the long-term risk of developing cancers such as leukemia and brain tumors. These risks are compounded by children's longer life expectancy and the potential for cumulative exposure from multiple imaging procedures (6).
Ultrasound provides a low-cost, non-invasive screening alternative that could transform pediatric fracture diagnosis, particularly in settings where pediatricians manage trauma with orthopedic support when bone injuries are suspected (1, 7, 8).
2. Objectives
This study aims to examine how emergency pediatricians manage musculoskeletal trauma in children. The objective is to reduce unnecessary radiation exposure, encourage the development of validated clinical rules for imaging, and evaluate the potential role of ultrasound in improving diagnostic accuracy.
3. Methods
We conducted a retrospective observational study involving 5,972 children aged 0 to 18 years who were admitted to the PED of the Fondazione Policlinico Universitario Agostino Gemelli IRCSS between January 1, 2017, and December 31, 2021, with a diagnosis of musculoskeletal trauma.
3.1. Inclusion Criteria
- Patients aged 0 - 18 years who presented to the Emergency Department between January 1, 2020, and December 31, 2021, with a primary diagnosis of acute musculoskeletal trauma (including fractures, sprains, strains, dislocations, or other injuries affecting the musculoskeletal system).
- Patients with complete medical records available in the electronic health record system.
3.2. Exclusion Criteria
- Patients with a concurrent diagnosis of traumatic brain injury.
- Patients with pre-existing musculoskeletal conditions that could significantly affect the outcome of the injury (e.g., osteoporosis, arthritis).
- Patients with incomplete data on age, gender, injury mechanism, or treatment.
- Patients who were transferred from another healthcare facility without complete medical records.
Data were collected by reviewing the hospital’s Electronic Medical Records, retrieved from the electronic system used in the PED (GIPSE, Dedalus S.p.A, Tuscany, Italy®). The data included information on age, gender, the location where the trauma occurred, the site of trauma, triage color code, imaging examinations, diagnosis of fracture, hospitalization rate, and destination ward.
Triage color codes were assigned to patients upon admission to the PED by the triage nurse based on the child’s general condition, symptoms, and vital signs. In our region, hospital triage is based on a system of five numerical codes (from 1 to 5) where: One represents “emergency,” 2 “urgency,” 3 “moderate urgency,” 4 “minor urgency,” and 5 “non-urgency”.
Patients were categorized into two groups: Fracture Yes or Fracture No, based on the radiologist’s review of the X-rays performed.
Data regarding radiological exams (X-rays) performed were grouped according to the site of trauma: Hand’s region (hand, wrist, hand’s fingers); upper limbs (arm, forearm, elbow, shoulder); foot’s district (ankle, heel, foot, toes); lower limbs (leg, thigh, femur, knees); and face’s district (face, nasal bones, chin, lips, cheekbone).
The study was conducted in accordance with the Helsinki Declaration. As per current legislation and the retrospective nature of the study, local ethics committee approval was not required. Informed consent was obtained verbally from the parents of the participants. Data were analyzed retrospectively while adhering to data protection policies.
3.3. Statistical Analysis
Continuous variables were reported as median [interquartile range] and were compared using the Mann-Whitney U test for two groups or the Kruskal-Wallis one-way ANOVA for three or more groups at univariate analysis. Categorical variables were expressed as absolute numbers (percentages) and were compared using the chi-square test or Fisher’s exact test when appropriate.
A two-sided P-value ≤ 0.05 was considered statistically significant for all analyses. Data were analyzed using SPSS v25® (IBM, Armonk, NY, USA).
4. Results
A retrospective, single-center study was conducted involving 5972 pediatric patients who accessed the emergency department of the “Fondazione Policlinico Universitario Agostino Gemelli, IRCSS” with a diagnosis of trauma. Of these patients, 2234 (37.4%) were female, and 3738 (62.6%) were male.
The age range of the patients was categorized into four groups: 0 - 2 years (9.4%), 2 - 5 years (14.4%), 6 - 11 years (35.7%), and 12 - 18 years (40.5%).
A comparison was made between patients with radiologically confirmed fractures (Fracture Yes group) and those without (Fracture No group). The Fracture Yes group included 2321 patients (38.8%), with a higher proportion of males (66%) and patients aged 6 - 11 years (40.5%). Conversely, the Fracture No group comprised 3651 patients (61.1%), with a larger proportion of patients aged 0 - 2 years (12.9%). The mean age of patients with fractures was 10.7 years, significantly higher than those without fractures (9.8 years). There was a statistically significant difference in sex and age distribution between the two groups (P < 0.05) (Table 1).
| Variables | Fracture No | Fracture Yes | Total | P-Value |
|---|---|---|---|---|
| Gender | ||||
| Male | 1444 (39.6) | 790 (34.0) | 2234 (37.4) | |
| Female | 2207 (60.4) | 1531 (66.0) | 3738 (62.6) | |
| Age (y) | ||||
| 0 - 2 | 472 (12.9) | 87 (3.7) | 559 (9.4) | |
| 3 - 5 | 566 (15.5) | 296 (12.8) | 862 (14.4) | |
| 6 - 11 | 1193 (32.7) | 940 (40.5) | 2133 (35.7) | |
| 12 - 18 | 1420 (38.9) | 998 (43.0) | 2418 (40.5) | |
| Total | 3651 (100) | 2321 (100) | 5972 (100) | < 0.005 |
| Triage color code | ||||
| Red | 318 (8.7) | 74 (3.2) | 392 (6.6) | |
| Orange | 333 (9.1) | 440 (19.0) | 773 (12.9) | |
| Light blue | 189 (5.2) | 168 (7.2) | 357 (6.0) | |
| Green | 2803 (76.8) | 1635 (70.4) | 4438 (74.3) | |
| White | 3 (0.1) | 3 (0.1) | 6 (0.1) | |
| Not evaluated | 5 (0.1) | 1 (0.0) | 6 (0.1) | |
| Total | 3651 (100) | 2321 (100) | 5972 (100) | < 0.005 |
Characteristics of Study Population and Triage Color Code Comparing Fracture Yes vs. Fracture No a
Upon admission, patients were categorized into different triage color codes based on the severity of their condition. A total of 392 patients (6.6%) were classified as "red," indicating the most urgent cases. Among these, 318 (8.7% of the total without fractures) did not have fractures, while 74 (3.2% of the total with a fracture) were diagnosed with a fracture.
For patients triaged as "orange," there were 773 individuals, of whom 440 (19% of the total with a fracture) had evidence of a fracture. Similarly, in the "light blue" group, comprising 357 patients, 168 (7.2% of the total with a fracture) were found to have a fracture.
Statistical analysis revealed a significant difference (P < 0.05) in the distribution of fractures across the different triage color codes (Table 1).
Analyzing the location of trauma occurrence, a significant proportion of injuries (23%) took place in domestic settings. Among these domestic accidents, 66% did not result in fractures. Sports-related injuries accounted for 19.9% of the cases. Interestingly, a significantly higher proportion of sports-related injuries (50%) resulted in fractures compared to domestic accidents (P < 0.05) (Table 2).
| Variables | Fracture No | Fracture Yes | Total | P-Values |
|---|---|---|---|---|
| Place | ||||
| Domestic | 916 (25.1) | 457 (19.7) | 1373 (23) | |
| Work | 8 (0.2) | 4 (0.2) | 12 (0.2) | |
| Sport | 586 (16.1) | 601 (25.9) | 1187 (19.9) | |
| School | 516 (14.1) | 244 (10.5) | 760 (12.7) | |
| Street | 722 (19.8) | 247 (10.6) | 969 (16.2) | |
| Others | 903 (24.7) | 767 (33.1) | 1670 (28.0) | |
| Total | 3651 (100) | 2321 (100) | 5972 (100) | < 0.005 |
| Regionb | ||||
| Hand | ||||
| 0 | 2995 (82.0) | 1704 (73.4) | 4699 (78.7) | < 0.005 |
| 1 | 656 (18.0) | 617 (26.6) | 1273 (21.3) | < 0.005 |
| Upper limb | ||||
| 0 | 3395 (93.0) | 1242 (53.5) | 4637 (77.7) | < 0.005 |
| 1 | 255 (7.0) | 1079 (46.5) | 1334 (22.3) | < 0.005 |
| Foot | ||||
| 0 | 3142 (86.1) | 2086 (89.9) | 5228 (87.5) | < 0.005 |
| 1 | 509 (13.9) | 235 (10.1) | 744 (12.5) | < 0.005 |
| Lower limb | ||||
| 0 | 3376 (92.5) | 2117 (91.2) | 5493 (91.0) | < 0.005 |
| 1 | 275 (7.5) | 204 (8.8) | 479 (8.0) | < 0.005 |
| Face | ||||
| 0 | 2611 (71.5) | 2180 (93.9) | 4791 (80.2) | < 0.005 |
| 1 | 1040 (28.5) | 141 (6.1) | 1181 (19.8) | < 0.005 |
| Total | 3651 (100) | 2321 (100) | 5972 (100) | < 0.005 |
Place of Trauma and Site of Trauma Comparing Fracture Yes vs. Fracture No a
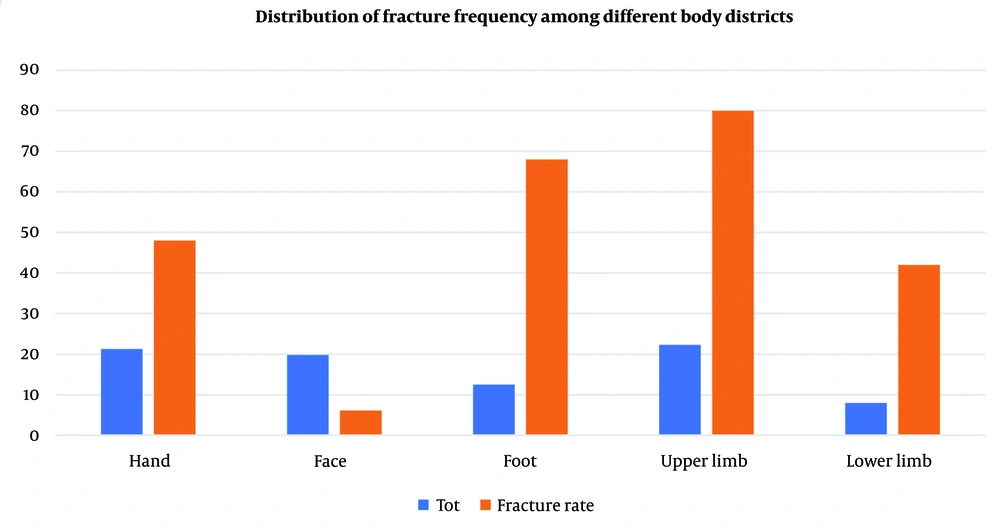
Regarding the outcomes, the majority of patients (44.8%) were discharged home, while 8.7% required hospitalization. Patients without fractures were significantly more likely to be discharged home (61.1%) compared to those with fractures (14.3%). To evaluate the appropriateness of radiological examinations, the study compared the frequency and diagnostic yield of X-rays in patients with and without fractures. The main findings revealed:
- Hand X-rays: Performed in 21.3% of patients, with 48% showing fractures.
- Face X-rays: Conducted in 19.8% of patients, with a lower fracture detection rate of 6.1%.
- Foot X-rays: Conducted in 12.5% of patients, with 68% yielding no fractures.
- Upper limb X-rays: Performed in 22.3% of patients, showing a high fracture rate of 80%.
- Lower limb X-rays: Conducted in 8% of patients, with 42% revealing fractures.
Overall, there was a significant difference in the frequency and diagnostic yield of X-rays across different body regions (P< 0.05) (Table 2 and Figure 1).
5. Discussion
For a long time, one of the biggest challenges for pediatricians has been ensuring radiation protection for young patients (9, 10). In tertiary emergency rooms, pediatricians are typically the first physicians to evaluate children with musculoskeletal trauma. Consequently, the decision to request an X-ray to rule out a fracture often lies with the pediatrician (11).
Over the years, numerous validated clinical decision rules have been developed to reduce unnecessary X-rays in children, particularly for wrist and ankle injuries. These include the low risk ankle rule (LRAR) and the Amsterdam Pediatric Wrist Rules, which are essential tools that all emergency pediatricians should be familiar with (12-14).
Additionally, the potential overuse of X-rays in pediatric trauma has significant cost implications for healthcare systems. For instance, Ramasubbu et al. conducted a study in 2015, concluding that implementing LRAR at their institution could reduce ankle X-rays by 64%. Considering the cost of an ankle X-ray and interpretation was estimated at €47 ($65), with more than 800 performed annually, a potential yearly saving of €25,000 ($34,500) was projected (15).
The primary objective of presenting our data was to evaluate pediatricians' approach to musculoskeletal injuries in children and to explore whether some routine radiographs could be avoided in favor of radiation-saving techniques, such as ultrasound. Our findings align with previous research, showing that males are more likely to sustain fractures than females (16). Moreover, we observed a higher incidence of fractures among children aged 6 - 11 and 12 - 18 years, likely due to increased physical activity during these developmental stages. As Randsborg PH stated in 2013, most pediatric fractures occur outdoors. Younger children are particularly at risk of sustaining fractures on playgrounds, while older children tend to sustain fractures during recreational and organized sports (17).
Our analysis of injury sites revealed that while domestic accidents were the most common cause of injury, sports-related accidents were associated with a higher incidence of fractures. Interestingly, according to current literature, a significant proportion of patients involved in domestic accidents who underwent X-rays did not have fractures (16, 18-20).
When considering the triage color code used upon admission, we found that patients with more severe injuries (red code) underwent a more comprehensive radiological workup compared to those with less severe injuries (orange or light blue code). This suggests that the decision to perform additional imaging was influenced by the severity of the injury rather than the presence or absence of a fracture, as highlighted in the most recent review regarding the management of the polytraumatized child by Ciorba and Maegele in 2024 (21).
Moreover, hospitalized children were more likely to have a fracture due to the severity of their condition and the associated treatment. When comparing the body regions where X-rays were performed, we found that the hands and upper limbs were the most common sites, and these regions also had a higher prevalence of fractures, consistent with previous studies (22, 23).
Our data suggests that a pediatrician's decision to perform an X-ray on the upper limb is often associated with a positive finding of a fracture. Conversely, while fewer radiographs were performed on the foot, a substantial proportion of these were negative for fractures. These findings align with previous literature but underscore the need to educate emergency pediatricians on the use of validated clinical scores to safely and effectively reduce the rate of radiography, especially in ankle injuries, without missing clinically significant fractures (24-26).
Most of the radiographs performed were negative for fractures. Specifically, we could have saved 656 X-rays of the hand region (51% of the total hand X-rays), 509 in the foot region (68% of the total in the foot region), 255 in the upper limb area (19%), and 275 in the lower limb area (57% of the total lower limb X-rays).
Based on our findings, we estimate that a significant number of unnecessary X-rays could have been avoided, particularly in the hand, foot, and lower limb regions. This highlights the potential of musculoskeletal ultrasound as an alternative imaging modality to reduce radiation exposure in pediatric patients. Alternatively, a "wait-and-see" approach, combined with close clinical monitoring, may be considered for patients with low-risk injuries.
Musculoskeletal ultrasonography (US) is gaining increasing prominence in pediatric imaging, enabling dynamic visualization of anatomical structures and facilitating minimally invasive procedures (1, 27). While radiography remains the gold standard for evaluating traumatic injuries, musculoskeletal US offers unique advantages in assessing various conditions, including the alignment of unossified structures, physeal fractures, occult fractures, joint separations, intra-articular bodies, ligamentous injuries, and periosteal reactions (28).
The portability, cost-effectiveness, radiation-free nature, and lack of contraindications make ultrasound an attractive modality for pediatric orthopedic applications (29-31).
5.1. Conclusions
In conclusion, our findings reveal a significant number of negative radiographs for pediatric musculoskeletal injuries, particularly in the lower limb district. These results underscore the need for alternative imaging modalities to reduce unnecessary radiation exposure. Musculoskeletal ultrasound emerges as a promising candidate, given its ability to provide valuable diagnostic information without the risks associated with ionizing radiation. To fully realize the potential of ultrasound in pediatric orthopedics, comprehensive training programs should be implemented to equip emergency department pediatricians and radiologists with the necessary skills.
A limitation of this study is its retrospective design, which can be subject to recall bias and selection bias. Additionally, the study was conducted at a single institution, limiting the generalizability of the findings to other healthcare settings. Furthermore, the retrospective nature of the data may have resulted in incomplete or missing information for some variables. While the study provides valuable insights into the management of musculoskeletal injuries in pediatric patients, further prospective studies with larger sample sizes or studies directly comparing X-ray and ultrasound are needed to confirm these findings and explore additional factors that may influence outcomes.