1. Background
Pneumonia is a common, frequently occurring disease and a leading cause of death in children. It is primarily caused by viruses, fungi, mycoplasma, and other pathogens, with multi-pathogen infections often leading to severe pneumonia (1). Children with pneumonia who develop severe respiratory and ventilatory dysfunction or a systemic inflammatory response may be diagnosed with severe pneumonia (2). Severe pneumonia is often associated with complications such as respiratory failure, lung abscess, pleural effusion, and pneumothorax, characterized by acute onset, numerous complications, and prolonged hospitalization (3). Currently, mortality rates from severe pneumonia remain high, accounting for a significant proportion of global deaths among children (4).
Current clinical treatments for severe pneumonia in the intensive care unit (ICU) primarily include anti-infection therapies, immune support, and nutritional supplementation, which, when combined with effective nursing care, can provide critical support. Routine care is typically administered following the physician’s instructions upon admission, with a focus on monitoring vital signs, conducting laboratory and imaging examinations. However, the psychological and daily needs of children are often overlooked (5). For young children, especially those experiencing separation anxiety, the limitations of routine care may contribute to poor psychological and emotional well-being, negatively affecting clinical outcomes.
To date, the scope and focus of nursing have expanded from traditional disease-centered care to include psychological, social, and family-centered approaches, encompassing not only patients but also their families and healthy individuals (6). Family-centered care compensates for the limitations of routine care and maximizes the efficient use of limited nursing resources. At its core, family-centered nursing prioritizes information exchange and open communication (7). This approach emphasizes detailed, humanistic care by strengthening collaboration between family members and the healthcare team, effectively alleviating children's pain and negative emotions, reducing parental anxiety and financial burden, and fostering a harmonious nurse-patient relationship (8). Additionally, family-centered care empowers family members to provide consistent support both in the hospital and post-discharge, promoting children's growth and intellectual development (9).
Currently, family-centered nursing has been shown to significantly improve children’s psychological well-being and enhance the overall quality of care (10). However, few studies have examined its effects specifically on children with severe pneumonia in the ICU, leaving it unclear whether this approach can improve their emotional well-being and quality of life (QOL).
2. Objectives
In response, this study aimed to investigate the effects of family-centered nursing on the emotional well-being and QOL of children with severe pneumonia in the ICU, seeking to provide valuable evidence for enhancing patient outcomes.
3. Methods
3.1. Subjects
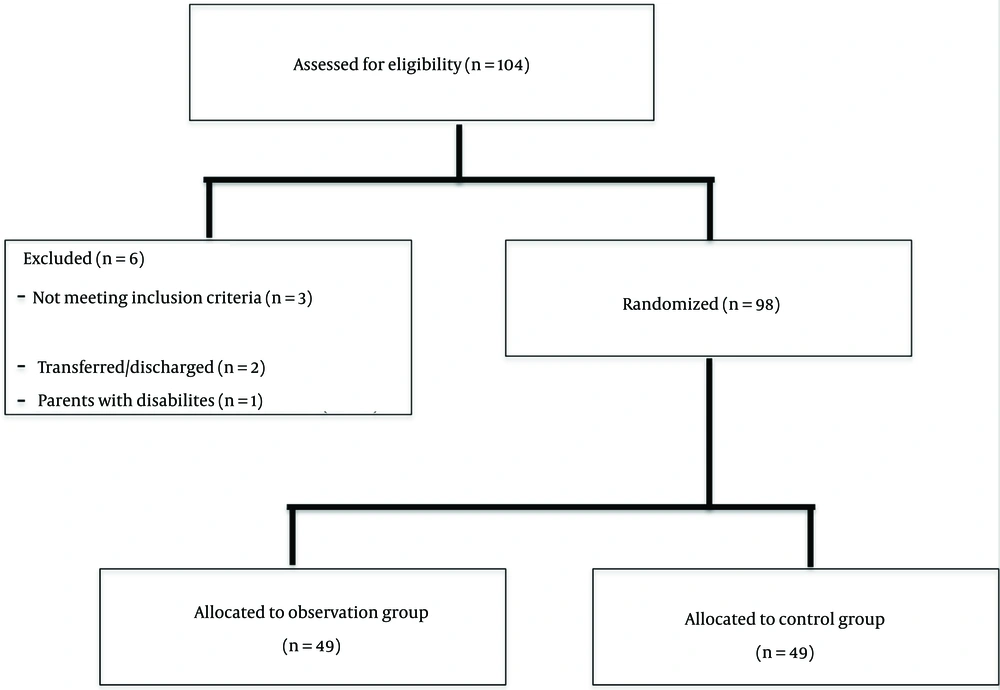
This study was approved by the hospital’s ethics committee, and written informed consent was obtained from the caregivers of all participating children. Sample size was determined based on pre-experimental results. A total of 98 children with severe pneumonia in the ICU, admitted from April 2021 to January 2023, were selected and sequentially numbered according to their admission number. They were divided into an observation group (n = 49) and a control group (n = 49) using a computer-generated random number table. The allocation sequence was concealed in sequentially numbered, sealed, opaque envelopes. Participants were not informed of their group assignment to reduce performance bias. The flow diagram of participant enrollment is shown in Figure 1.
The diagnostic and inclusion criteria were as follows: (1) children meeting the diagnostic criteria for severe pneumonia (11), (2) children under 15 years old, and (3) those whose parents had the ability to communicate and read.
Exclusion criteria included: (1) children with other serious diseases, (2) those transferred to another hospital or discharged before recovery, and (3) those with parents who had mental or intellectual disabilities.
3.2. Nursing Methods
All children in both groups received nursing care from admission until transfer out of the ICU or discharge. Routine nursing was given for the control group, specifically as follows:
(1) Psychological counseling: The primary nurse assessed the psychological characteristics of the children, helping them adapt to the ICU environment as quickly as possible. Diagnosis, treatment, and nursing interventions were carried out in a gentle, compassionate manner. Nurses worked to stabilize the children’s emotions and distract their attention with encouraging and comforting words, facilitating the quick and accurate implementation of medical procedures and care measures.
(2) Condition monitoring: Regular monitoring of the children's conditions and vital signs was conducted to assess symptom improvement and lung function changes. Posture adjustments, back percussion for sputum aspiration, oxygen therapy, and aerosol inhalation were provided as needed. The ward bed was kept clean and dry, and a quiet environment for rest was ensured.
(3) Medication administration: Antibiotic, antiasthmatic, antitussive, and expectorant medications were administered as prescribed. Patients with indwelling gastric tubes received nasogastric feeding of enteral nutrition liquid, and adverse reactions to medications were observed. Family members were not involved in medical care.
Based on the treatment provided to the control group, family-centered nursing was implemented for the observation group, consisting of the following:
(1) Team establishment: A care team was formed, consisting of one pediatrician and three primary nurses. The pediatrician was responsible for physical examinations, diagnosis, and treatment, while the primary nurses provided information and guidance to parents, who were encouraged to actively participate in their child’s care alongside the medical staff.
(2) Individualized family guidance: Upon admission, medical staff gathered general information about the child and family and tailored guidance based on specific needs. Educational brochures and psychological support were provided, covering topics such as symptom recognition, correct medication administration, and precautions. Medical staff addressed parents' questions daily and engaged in ongoing communication. Collaborative family-participatory nursing included life and technical care, information sharing, and emotional support.
Life nursing: This included care for the child’s oral and respiratory hygiene, skin care, and temperature monitoring.
Technical nursing included the following aspects:
Physical cooling: Staff explained the purpose, correct methods, precautions, and key techniques for physical cooling methods (such as using an ice bag or warm water sponge bath) and involved parents in the process.
Pain management: Gentle psychological support was provided to distract children and reduce their pain sensitivity.
Respiratory care: Oxygen flow was adjusted based on blood gas analysis, and aerosol inhalation was provided as needed to manage sputum volume and viscosity. Disposable nebulizers and mechanical expectoration were used for inhalation therapy.
Monitoring severe condition changes: Medical staff educated parents on recognizing severe condition changes and demonstrated emergency response techniques.
Primary nurse involvement: The primary nurse participated in daily morning rounds and case discussions for critically ill children, ensuring that changes in the child’s condition informed timely adjustments to the nursing plan.
(3) Health education and online support: Parents received health guidance and access to online consultations through the 317 Nursing Education Platform.
(4) Post-ICU and Discharge Guidance: Individualized instructions were provided to parents covering infection prevention, home disinfection, daily hygiene, observation of symptoms, and medication management after the child’s transfer out of the ICU or discharge.
3.3. Observation of Clinical Manifestations
The length of ICU stay, the time to return to normal temperature (36 - 37.5°C), and the time to disappearance of lung moist rales (indicated by the absence of small and medium bubbling sounds in lung auscultation) were recorded for both groups.
3.4. Measurement of Blood Gas Analysis Indicators
Partial pressure of oxygen (PaO₂; normal range: 80 - 100 mmHg), partial pressure of carbon dioxide (PaCO₂; normal range: 35 - 45 mmHg), and oxygen saturation (SaO₂; normal range: 91 - 97.7%) were measured using a Cobas b 123 blood gas analyzer (Runda Medical Technology Co., Ltd., China) before and after the nursing interventions. The device was calibrated and maintained regularly by trained personnel.
3.5. Assessment of Psychological Emotion
Before and after nursing, the psychological status of the children was evaluated by family members and nurses using the Schedule for the Assessment of Insight (SAI) (12), adapted for pediatric use. Family members provided insight into the children’s recognition, awareness, and ability to describe their feelings or behaviors, tracking improvements or regressions over time. Nurses assessed these elements through professional judgment during interactions with the children, noting responses to interventions and communication about emotional states. Total scores ranged from 0 - 6, with higher scores indicating better psychological status.
To ensure privacy during assessments, evaluations were conducted in private settings within the ICU, allowing participants and family members to feel secure and comfortable. Access to these assessment areas was restricted to authorized personnel directly involved in the study, maintaining confidentiality. All data collected were anonymized, with each participant assigned a unique identification code, and no personal identifiers used in any records or analyses.
3.6. Evaluation of QOL
The children's QOL was assessed by family members and nurses before and after nursing interventions using the Short Form-36 Health Status Questionnaire (SF-36) (13). Three domains were selected: Physical function, social function, and emotional function. Each domain was scored out of 100 points, with higher scores indicating better QOL.
3.7. Assessment of Family Member Satisfaction
Following the nursing interventions, family members' satisfaction with the service and nursing process was evaluated using the Client Satisfaction Questionnaire-8 (CSQ-8, score range: 8 - 32 points) and the Measure of Processes of Care 20-item (MPOC-20, score range: 1 - 7 points) (14, 15). Higher scores indicated higher levels of satisfaction. One family member per child completed the survey.
3.8. Observation of Adverse Events
Possible adverse events among children and their family members, such as increased anxiety or stress, emotional distress, fatigue, and exhaustion, were monitored throughout the care process.
3.9. Statistical Analysis
Data analysis was performed using SPSS 26.0 software. Measurement data were tested for normality with the Shapiro-Wilk test. Normally distributed data were presented as "mean ± standard deviation (x̄ ± s)" and analyzed within groups using paired-samples t-tests, and between groups using independent-samples t-tests. Count data (ratios) were presented as "[n (%)]" and analyzed using the χ² test. Statistical significance was set at P < 0.05.
4. Results
4.1. General Data
No statistically significant differences were observed in baseline characteristics between the two groups (P > 0.05) (Table 1).
| Group | Case (n = 49) | Control (n = 49) | t or χ2 Value | P-Value |
|---|---|---|---|---|
| Age (y) | 2.35 ± 0.16 | 2.29 ± 0.18 | t = 1.744 | 0.084 |
| Gender (M/F) | 23/26 | 25/24 | χ2 = 0.163 | 0.686 |
| Duration of pneumonia (mo) | 2.29 ± 0.11 | 2.31 ± 0.09 | t = 0.985 | 0.327 |
| Only child | 45 (91.84) | 44 (89.80) | χ2 = 0.000 | 1.000 |
| Age of family member (y) | 28.35 ± 4.76 | 27.82 ± 4.33 | t = 0.577 | 0.566 |
| Gender of family member (M/F) | 19/30 | 17/32 | χ2 = 0.176 | 0.675 |
a Values are expressed as mean ± SD or No. (%).
4.2. Clinical Manifestations
During care, the recovery time for clinical symptoms in the observation group was shorter than that of the control group (P < 0.05) (Table 2).
| Group | Case (n = 49) | Control (n = 49) | t | P-Value |
|---|---|---|---|---|
| Length of ICU stay/d | 6.12 ± 2.07 b | 8.69 ± 2.72 | 5.263 | < 0.001 |
| Time of temperature returning to normal/d | 3.35 ± 0.49 b | 4.01 ± 0.42 | 7.159 | < 0.001 |
| Disappearance time of lung moist rales/d | 5.17 ± 1.75 b | 6.48 ± 1.83 | 3.622 | 0.001 |
| PaO 2 /mmHg | ||||
| Before care | 69.54 ± 5.23 | 69.41 ± 5.20 | 0.123 | 0.902 |
| After care | 91.55 ± 4.28 c | 80.67 ± 5.79 c | 10.578 | < 0.001 |
| PaCO 2 /mmHg | ||||
| Before care | 45.97 ± 2.88 | 46.01 ± 3.08 | 0.066 | 0.947 |
| After care | 36.32 ± 2.94 c | 42.26 ± 2.37 c | 11.011 | < 0.001 |
| SaO 2 /% | ||||
| Before care | 79.81 ± 5.12 | 79.33 ± 4.95 | 0.472 | 0.638 |
| After care | 92.20 ± 6.51 c | 84.09 ± 12.81 c | 3.951 | < 0.001 |
a Values are expressed as mean ± SD.
b P < 0.05 vs. the control group.
c P < 0.05 vs. before care.
4.3. Blood Gas Analysis Indicators
After nursing interventions, blood gas analysis indicators improved in both groups, with significantly greater improvements in the observation group compared to the control group (P < 0.05) (Table 2).
4.4. Psychological Emotion
Post-intervention, the psychological status scores in the observation group were significantly higher than those in the control group (P < 0.05) (Table 3).
| Group | Case (n = 49) | Control (n = 49) | t | P-Value |
|---|---|---|---|---|
| Psychological emotion | ||||
| Before care | 1.51 ± 0.09 | 1.48 ± 0.13 | 1.328 | 0.187 |
| After care | 5.23 ± 0.31 b | 4.68 ± 0.32 b | 8.641 | < 0.001 |
| Physical function | ||||
| Before care | 52.33 ± 9.88 | 53.16 ± 9.54 | 0.423 | 0.673 |
| After care | 76.12 ± 10.07 c | 67.09 ± 9.82 | 4.490 | < 0.001 |
| Social function | ||||
| Before care | 50.73 ± 10.29 | 49.87 ± 10.82 | 0.403 | 0.688 |
| After care | 79.25 ± 12.89 c | 70.37 ± 12.02 | 3.527 | 0.001 |
| Emotional function | ||||
| Before care | 53.45 ± 11.06 | 51.93 ± 11.79 | 0.658 | 0.512 |
| After care | 75.17 ± 13.10 c | 65.30 ± 12.44 | 3.824 | < 0.001 |
a Values are expressed as mean ± SD.
b P < 0.05 vs. before care.
c P < 0.05 vs. the control group.
4.5. Quality of Life
Following care, the observation group scored higher in QOL domains compared to the control group (P < 0.05) (Table 3).
4.6. Family Satisfaction
After nursing interventions, family member satisfaction was significantly higher in the observation group than in the control group (P < 0.05) (Table 4).
4.7. Adverse Events
No adverse events were observed among children or their family members, including anxiety, stress from the modified care routines or family presence, emotional distress from increased care demands, or fatigue from additional engagement in family-centered care.
5. Discussion
This study found that ICU stay duration, time to temperature normalization, and time to disappearance of lung moist rales were significantly shorter in the observation group compared to the control group, indicating that family-centered care can greatly improve clinical outcomes for children with severe pneumonia in the ICU. This is likely because the individualized care content and structured scheduling in family-centered care allow nurses to readily consult guidelines, inquire about specific needs, and adhere to their assigned responsibilities, thereby enhancing care effectiveness and promoting faster symptom resolution in children (16). Similarly, research by Pitch et al. has demonstrated the benefits of family-centered care in enhancing clinical outcomes for pediatric patients (17).
The blood gas indicators—partial pressure of oxygen (PaO₂), partial pressure of carbon dioxide (PaCO₂), and oxygen saturation (SaO₂)—are critical markers in assessing respiratory function in children with pneumonia. PaO₂ reflects the pressure exerted by oxygen molecules in the blood, thus indicating external respiratory function. PaCO₂ measures the pressure of CO₂ in plasma, serving as a key marker of potential respiratory failure, while SaO₂ gauges the blood's oxygen-carrying and -delivering capacity. Together, these indicators provide a direct reflection of blood gas status in pediatric pneumonia (18). This study observed that both groups showed improvements in blood gas indicators following care, with the observation group exhibiting significantly better improvements than the control group. This suggests that family-centered care can markedly enhance blood gas levels in children with severe pneumonia in the ICU. This effect may be due to the individualized approaches of family-centered care, which shift nurses’ focus to personalized needs and promote better treatment adherence, thereby optimizing care outcomes (19). Moreover, individualized care based on symptom severity and routine monitoring of lung function can help improve ventilation and blood gas levels. In alignment, the study by Gafni-Lachter and Ben-Sasson demonstrated that regular lung function monitoring and care adjustments significantly improved both ventilation and blood gas levels, aiding in effective management of severe respiratory conditions (20).
Additionally, family-centered care proves to be more effective in calming children, as children who are consistently accompanied by their families are more likely to cooperate actively with treatments without causing added anxiety for medical staff or delays in medical procedures. This approach achieves a notably better overall effect than education and comfort provided by medical staff alone (21). Moreover, family-involved collaborative care allows parents to gain valuable information and emotional support, thereby increasing their confidence in managing responsibilities, giving them a greater sense of control over their child’s hospitalization, reducing their own anxiety, and providing emotional reassurance for their children (22). Family-centered care also enhances children’s QOL. Through active support from family members, caregivers can address relevant issues promptly, identify and alleviate families' negative emotions, and provide health education, all of which help engage families more fully in care. This, in turn, increases children’s compliance with treatments and care, ultimately improving both their condition and QOL (23). Similarly, family-centered care has been associated with better symptom management and significant improvements in the health and well-being of children with severe respiratory conditions (24).
This study also examined family member satisfaction and found that satisfaction was significantly higher in the observation group, suggesting that families of children with severe pneumonia in the ICU are more likely to respond positively to family-centered care. This approach meets parents' needs for respect, informed choice, and participation in medical decisions by providing multi-channel and multi-format information support. As a result, parents feel they can meaningfully participate in the family care system, reducing feelings of helplessness during hospitalization and improving their overall satisfaction with nursing services (25).
However, this study has certain limitations. It did not include a long-term follow-up, potential confounding factors were not discussed, and some subjective outcome measures may introduce bias. Consequently, these factors may influence the findings.
In conclusion, family-centered care significantly improves the clinical manifestations, blood gas levels, psychological well-being, and QOL of children with severe pneumonia in the ICU. Additionally, individualized care measures and information guidance effectively enhance parental satisfaction and contribute to the timely improvement of children’s conditions. Although this study specifically focuses on children with severe pneumonia in the ICU, the principles and protocols of family-centered care are broadly applicable across pediatric ICU settings. We believe these findings can be generalized following further research aimed at replicating these results in different hospitals and diverse populations.