1. Background
Pain is one of the main concerns for patients after surgery. Inadequate pain control can lead to cardiovascular complications, decreased respiratory function, pulmonary issues, delayed return of bowel movements, ileus, impaired urination, and prolonged hospitalization (1-4). In the case of children and infants, the misconception that they do not feel or remember pain often results in insufficient pain management (4, 5). Acute post-surgical pain in children, like in adults, triggers respiratory, cardiovascular, neuroendocrine, digestive, immunological, and metabolic dysfunctions by activating intense physiological and biochemical stress responses. Painful surgical stimuli without sufficient analgesia can lead to long-term pain memory, chronic pain, and behavioral disorders in children (6-8).
Evaluating pain in children is particularly challenging due to factors like pain intensity, duration, threshold, and the emotional component of pain, which are more pronounced in children and infants (9-11). The perception of pain and the response to analgesics in children varies widely due to factors such as age, race, gender, anxiety, type of surgery, previous experience, and genetic factors (12). To manage acute pain after surgery in children, simple analgesics are typically used, though they are often insufficient, and in many cases, suboptimal doses are administered (13-16).
Selective use of regional anesthesia techniques during general anesthesia with long-acting local anesthetics offers the advantage of providing a pain-free recovery period and reducing the need for injectable narcotics or oral analgesics. Common regional anesthesia techniques include caudal block, peripheral nerve blocks (e.g., ilioinguinal and iliohypogastric nerve blocks), topical anesthesia (e.g., EMLA cream), and operative site blocks such as intra-wound infiltration (12). Delpizzo et al. demonstrated that regional anesthesia is frequently used in patients under 21 years old, especially for procedures such as knee arthroscopy, anterior cruciate ligament repair, and sports injury surgeries, to manage pain (17). Another study showed that regional anesthesia in children undergoing orthopedic surgery can be an effective and safe option for pain management (18). It has also been found that the use of regional anesthesia in children reduces the need for opioids during and after surgery (19).
Caudal anesthesia is the most commonly used regional anesthesia technique in children, especially for surgeries of the lower limbs and lower abdomen (20, 21). Peripheral nerve blocks and neuraxial techniques like the caudal block are often used in unilateral surgical procedures (22, 23).
The timing of caudal block administration is particularly important. When used before surgery, caudal block suppresses pain receptors in the spinal cord, nerve pathways, and neurons near the brain, delaying the onset of pain and improving patient management during and after surgery. Additionally, it reduces the patient’s need for pain-relieving drugs (24).
2. Objectives
In reviewing studies on children undergoing unilateral knee osteotomy surgery, limited research has been conducted on the effects of ultrasound-guided caudal block on intraoperative and postoperative pain management. Unilateral knee osteotomy is associated with severe pain and functional limitations, and caudal block is a widely used pain-relief technique in children that can be easily performed. Therefore, the aim of this study is to compare the effects of ultrasound-guided caudal block on pain management in children during and after unilateral knee osteotomy surgery.
3. Methods
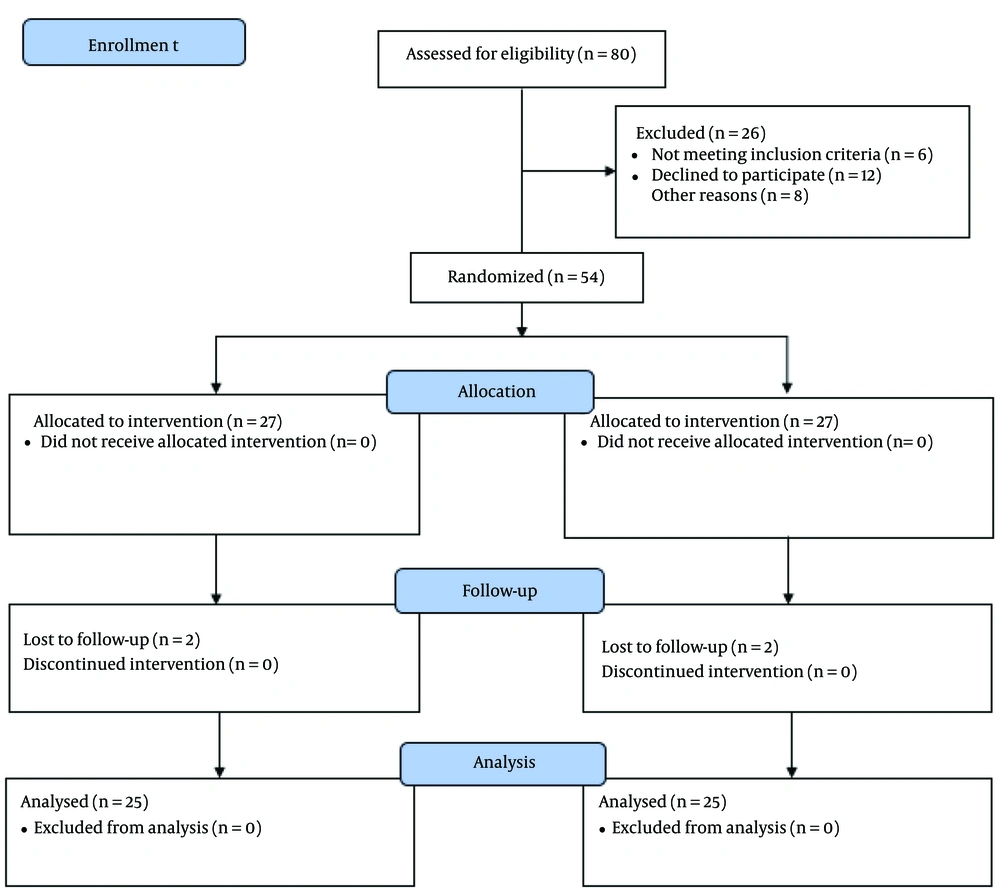
The present double-blinded clinical trial was conducted on a pediatric population scheduled for unilateral knee osteotomy surgery under general anesthesia with the total IV anesthesia (TIVA) technique. After receiving approval from the ethics committee (IR.IUMS.FMD.REC.1399.383) and obtaining a clinical trial code (IRCT20180723040570N6), as well as the written consent of parents, a total of 50 children aged 2 - 6 years of both sexes, with ASA class I or II, were included in the study (Figure 1). A restricted block randomization method was used. Inclusion criteria consisted of children who were candidates for unilateral knee osteotomy surgery, with no congenital knee disorders. Exclusion criteria included congenital spine abnormalities, history of sensitivity to the studied drugs, abnormal coccyx or spine anatomy, lumbar region infection, behavioral disorders, use of psychiatric drugs, lack of verbal communication with parents, and the use of sleeping pills upon entering the operating room.
The selection of children aged 2 - 6 years was based on the fact that caudal block is typically performed in this age group. Additionally, to avoid confounding factors and bias, similar scales were used for pain assessment. Since most of the patients at our center undergo unilateral knee osteotomy, this method was chosen for the study.
3.1. Randomization
To perform randomization, the block randomization method was used. First, blocks were prepared using combinations of English letters (AAABBB). In the next step, a number was assigned to each possible permutation of the blocks.
3.2. Blinding
The study was single-blinded. In this study, only the patients were unaware of the type of intervention and the drug used. However, the doctor and the researcher were aware of the type of drugs and interventions performed in the groups.
To maintain double-blinding in the study, the researchers who performed the block and evaluated the patients were unaware of the type of intervention.
Patients were subjected to standard monitoring, including electrocardiogram (ECG), pulse oximetry, Bispectral Index (BIS), and pain monitoring using the Analgesia Nociception Index (ANI) during surgery. The Propofol maintenance dose was adjusted based on the BIS. If BIS was < 50, the Propofol dose was increased by 20 µg/kg per hour. If BIS was >50, the Propofol dose was reduced by 20 µg/kg per hour from the maintenance dose. During the operation, the amount of Propofol, narcotics, BIS, and pain levels were measured using ANI and recorded in a checklist.
Analgesia Nociception Index measurement was as follows: Painful stimuli or nociception are detected by nerve fibers and transmitted to the brain and spinal cord, leading to sympathetic activation and parasympathetic inhibition. These changes affect heart rate, blood pressure, and pupil size. Monitors that measure pain during surgery display the patient's pain level quantitatively by analyzing these changes in heart rate and pupil size. Based on hemodynamic changes, the monitors show the degree of parasympathetic inhibition: A reading of 100 indicates no parasympathetic inhibition, meaning the patient is not in pain, while values below 50 indicate parasympathetic inhibition, sympathetic activation, and patient pain.
During surgery, if ANI was less than 50, indicating pain, Fentanyl was administered at a dose of 1 µg/kg. Postoperative pain was assessed at 2, 4, 6, 12, and 24 hours using the face, legs, activity, cry, and Consolability (FLACC) Scale (25). All patients received intravenous pain control via a pump containing paracetamol at a rate of 15 mg/kg with a flow of 6 cc/kg. If FLACC was < 5, Meperidine 0.5 mg/kg was administered intravenously. If Meperidine did not adequately control the pain, it was repeated. Side effects related to the caudal block, such as nausea, vomiting, and hypotension, as well as treatments with atropine, ephedrine, and ondansetron, were documented.
For the ultrasound-guided technique: First, a transverse image was used to locate the sacral hiatus between the two cornua. This image showed the upper hyperechoic line (the sacrococcygeal ligament) and the lower hyperechoic line, representing the posterior surface of the pelvis or sacrum. The probe was then rotated to obtain a longitudinal section (paramedian line in older children). The sacrococcygeal membrane, a relatively thick hyperechoic line toward the caudal side, was identified. The needle was inserted under direct visualization; the longitudinal view was optimal for observing the length of the needle. After inserting the needle, the transverse view was used to confirm the expansion of the local anesthetic in the caudal space.
3.3. Determination of Sample Size and Statistical Analysis
To analyze the data, SPSS version 28 statistical software was used. Frequency and percentage were reported for qualitative variables, while mean and standard deviation were reported for quantitative variables. Median and interquartile range were used for qualitative variables where applicable. The significance level for the statistical tests was set at 0.05.
Considering a confidence level of 95% and a power of 80%, the prevalence of pain in the first and second groups was 8.7% and 40.9%, respectively, based on Hasani et al.'s study (26). The minimum required sample size was determined to be 25 participants per group.
The sample size calculation formula is as follows:
4. Results
4.1. Demographical Information
Demographic data is shown in the table below. The average weight and the amount of narcotics used during recovery at different time points were higher in the first group compared to the second group (P = 0.96 for weight and P = 0.30 for narcotic use during recovery at different time points), while the average drug consumption was higher in the second group (P = 0.13). However, these differences were not statistically significant (P > 0.05) (Table 1).
| Variables | Groups | P-Value | |
|---|---|---|---|
| 1 | 2 | ||
| Weight (kg) | 23.28 ± 8.19 | 23.17 ± 9.14 | 0.96 |
| Drug consumption (µg/kg) | 22.5 ± 21 | 25 ± 23 | 0.13 |
| The amount of narcotic used in recovery at different hours | 12.93 ± 4.86 | 11.42 ± 5.37 | 0.30 |
a Values are expressed as mean ± SD.
4.2. Evaluation of Average Intraoperative Pain in 60 and 120 Minutes in the two Groups
The analysis showed that the average pain at 60 and 120 minutes was lower in the first group compared to the second group, and this difference was statistically significant (P < 0.001 for 60 minutes and P = 0.006 for 120 minutes) (Table 2).
| Variables | Groups Median (IQR) | P-Value | |
|---|---|---|---|
| 1 | 2 | ||
| Patient's pain during operation 60 minutes | 84.0 (16.0) | 92.0 (6.0) | < 0.001 |
| Patient's pain during operation 120 minutes | 85.0 (8.0) | 89.0 (5.0) | 0.006 |
| Changes rate | -2.00 (8.5) | -5.0 (3.5) | 0.010 |
4.3. Bispectral Index Mean Evaluation at 60 and 120 Minutes in the Two Groups
The results showed that the median BIS at 60 minutes was higher in the second group compared to the first, and this difference was statistically significant (P = 0.003). However, no significant difference was observed in the median BIS at 120 minutes (P = 0.896) (Table 3).
| Variables | Groups Median (IQR) | P-Value | |
|---|---|---|---|
| 1 | 2 | ||
| BIS during operation 60 minutes | 45.0 (5.0) | 50.5 (7.0) | 0.003 |
| BIS during operation 120 minutes | 50.0 (8.0) | 52.0 (12.0) | 0.896 |
| Changes rate | 4.0 (5.0) | 1.5 (8.0) | 0.041 |
Abbreviation: BIS, Bispectral Index.
4.4. Evaluation of Pain After Surgery in Different Recovery Hours in Two Groups
The table below presents the average pain levels at different hours of recovery (first, 2, 4, 6, 12, and 24 hours) for both groups. The analysis revealed that the average pain was lower in the second group across all time points compared to the first group. A statistically significant difference was observed between the two groups (P < 0.001 for initial recovery, 2, 4, 6, and 24 hours, and P = 0.007 for 12 hours) (Table 4).
| Variables | Groups Median (IQR) | P-Value | |
|---|---|---|---|
| 1 | 2 | ||
| The patient's pain during the initial recovery | 6.0 (1.0) | 4.0 (2.0) | < 0.001 |
| The patient's pain in the next 2 hours | 6.0 (1.0) | 4.0 (1.0) | < 0.001 |
| The patient's pain in the next 4 hours | 6.0 (1.0) | 4.0 (1.0) | < 0.001 |
| The patient's pain in the next 6 hours | 5.0 (1.0) | 3.0 (2.0) | < 0.001 |
| The patient's pain in the next 12 hours | 4.0 (0.0) | 3.0 (1.0) | 0.007 |
| The patient's pain in the next 24 hours | 3.0 (1.0) | 2.5 (1.0) | < 0.001 |
5. Discussion
Fifty children aged 2 - 6 years with ASA class I or II participated in this study. The results showed that the amount of Fentanyl used before extubation increased compared to the pre-surgery period. Additionally, the average pain at 60 and 120 minutes in the second group was higher than in the first group (92 ± 6 vs. 84 ± 16 for 60 minutes and 89 ± 5 vs. 85 ± 8 for 120 minutes). The average BIS was also higher in the second group compared to the first group (50.5 ± 7 vs. 45 ± 5 for 60 minutes and 52 ± 12 vs. 50 ± 8 for 120 minutes). Furthermore, the average post-surgical pain was lower in the group that received the caudal block after surgery and before extubation.
Benka et al. conducted a study to evaluate the effect of caudal block in children undergoing surgery. Their results showed that the amount of Propofol used when the caudal block was applied (7.83 mg/kg) was lower than when general anesthesia was used alone (11.33 mg/kg). Although these results differ from the present study, both studies confirmed reduced Propofol consumption when using the caudal block (27). Villalobos et al. demonstrated that oral Morphine consumption during and after surgery was reduced in children who underwent surgery with caudal epidural anesthesia compared to those who received lumbar plexus blockade. These findings are consistent with the present study (28)
Using a caudal block in patients results in pain reduction at different time points (2, 4, 6, 12, and 24 hours) after recovery. The exact mechanism of the caudal block has not been fully determined; however, it is known that the caudal block can alter ion channel and neuron function. Specifically, it has been shown that the caudal block increases the sensitivity of sodium channels and vanilloid receptors to stimulation signals and regulates the function of inhibitory neurons (29).
Ipek et al. found that using quadratus lumborum block, compared to caudal block, reduced postoperative pain. Additionally, they observed that the caudal block increased the duration of hospitalization. These results are not consistent with the present study, likely due to the comparison of different pain control methods (30). Another study demonstrated that the use of caudal epidural block in children undergoing infraumbilical surgery reduced pain during and after surgery compared to Transversus Abdominis Plane Block (31). Bumer et al. showed that using both caudal epidural block and popliteal nerve block can effectively manage and reduce pain in children undergoing elective foot surgery; however, the caudal epidural block is easier to administer compared to other methods (32).
In general, the results of this study suggest that administering the caudal block after surgery and before extubation can lead to reduced postoperative pain in patients. The study also demonstrated that the average BIS at 60 minutes was significantly lower in the group that received a caudal block before surgery compared to the group that received it after surgery. In a previous study, a significant difference in BIS was observed in children who underwent a caudal block during surgery compared to a control group (33).
Therefore, it can be concluded that administering the caudal block after surgery and before extubation, compared to administering it after induction, may increase the average BIS in patients.
5.1. Limitations
Since this study in children was based on FLACC criteria, the pain assessments were less reliable compared to those in adults. Additionally, confounding factors such as hunger and restlessness during pain measurement may have influenced the results.
5.2. Recommendation
This block was used for lower limb surgeries, and it is necessary to re-examine the findings of this study in future research with a larger sample size and different concentrations of anesthetic.