1. Background
Choanal atresia is characterized by the complete obstruction or constriction of the opening between the posterior nasal cavity and the nasopharynx (1). It represents one of the most common craniofacial abnormalities observed in the nose and frequently requires multiple corrective surgeries or can lead to life-threatening airway obstruction (2, 3). It is generally considered that infants should breathe through their nose. Congenital or acquired conditions causing nasal obstruction can result in respiratory distress in neonates. These respiratory disturbances often become apparent during the initial attempts at oral feeding. The possibility or suspicion of a congenital nasal anomaly is a common reason for an emergency consultation with an otolaryngologist. Choanal atresia or synechia should be considered when difficulties arise during catheter placement from the nasal cavity into the pharynx (1). Although congenital nasal anomalies are rare, they have the potential to threaten life due to upper airway obstruction. Therefore, persistent nasal obstruction is an important clinical entity in terms of diagnosis and treatment.
Numerous surgical techniques have been suggested for the repair of congenital choanal atresia. In recent years, significant progress has been made in surgical techniques for treating choanal atresia with the acceptance of various approaches such as transnasal, transantral, transpalatal, and transseptal methods. The primary surgical complication remains restenosis, which has prompted efforts to reduce its occurrence through revision procedures aimed at preserving choanal patency (4).
However, there is no consensus on the optimal surgical technique. To prevent the risk of restenosis and the need for further surgeries, many researchers advocate for the use of mucosal flaps, often combined with postoperative stenting. Since the introduction of the first pharyngeal mucosal flap in a 1990 report, numerous studies have detailed diverse shapes and designs for mucosal flaps, such as the swinging door flap, mirrored L-shaped septonasal flap, nasal septal crossover flap, and folded-over flaps (5, 6). Many authors have shared endoscopic techniques without stenting, which involve sufficient posterior septoplasty, removal of excess lateral root, and combined separation of mucosal flaps. A device with vascularized endonasal mucosal flaps exposes the underlying blood, promotes the proliferation of granulation tissue, inhibits the growth of scar formation, and improves functional outcomes. However, there is no consensus supporting the technique and outcome of healing (7).
2. Objectives
In this study, we aimed to evaluate the long-term results of the endoscopic septonasal flap technique combined with silicone stents for the repair of congenital choanal atresia in neonates and infants, and to determine independent predictors of surgical success.
3. Methods
The prospective study was conducted at Harran University Hospital from February 2020 to December 2022, after approval from the Harran University Clinical Research Ethics Committee (Date: 02/10/2020 and 20.03.18 decision).
In this study, 40 patients with a diagnosis of choanal atresia who were brought to the otolaryngology outpatient clinic due to congenital nasal obstruction or followed in the neonatal intensive care unit were included. To ensure impartiality, patients were followed independently by two otolaryngologists and a pediatrician who maintained and controlled the treatment.
The study followed the principles outlined in the declaration of Helsinki. Age, gender, birth weight, gestational week of birth, duration of stay in the intensive care unit, nutritional status, unilateral and/or bilateral nasal obstruction, etiological comorbidities, associated comorbid conditions, accompanying syndromic disorders, diagnostic imaging, and follow-up of the patients were included in the study. Medical treatment and surgical interventions were applied, and recurrence rates were recorded. All patients underwent preoperative CT imaging.
3.1. Population and Sample of the Research
The minimum sample size required to detect a significant difference using this test should be at least 20 in each group (40 in total), considering a type I error (alpha) of 0.05, power (1-beta) of 0.8, effect size of 0.82, and two-sided alternative hypothesis (H1) (8). In this study, 40 patients diagnosed with choanal atresia were included.
3.2. Inclusion Criteria
Patients included in the study were aged 0 - 48 months, underwent flexible nasal and nasopharyngoscopic examinations with the diagnosis confirmed on computed tomography, and completed postoperative follow-up examinations at the 1st and 3rd weeks, 3rd and 6th months, and 1st year.
3.3. Exclusion Criteria
Patients were excluded from the study if they did not have CT imaging, had any lower respiratory tract disease or chromosomal anomalies, or did not attend follow-up examinations regularly.
3.4. CT Findings, Diagnostic Method
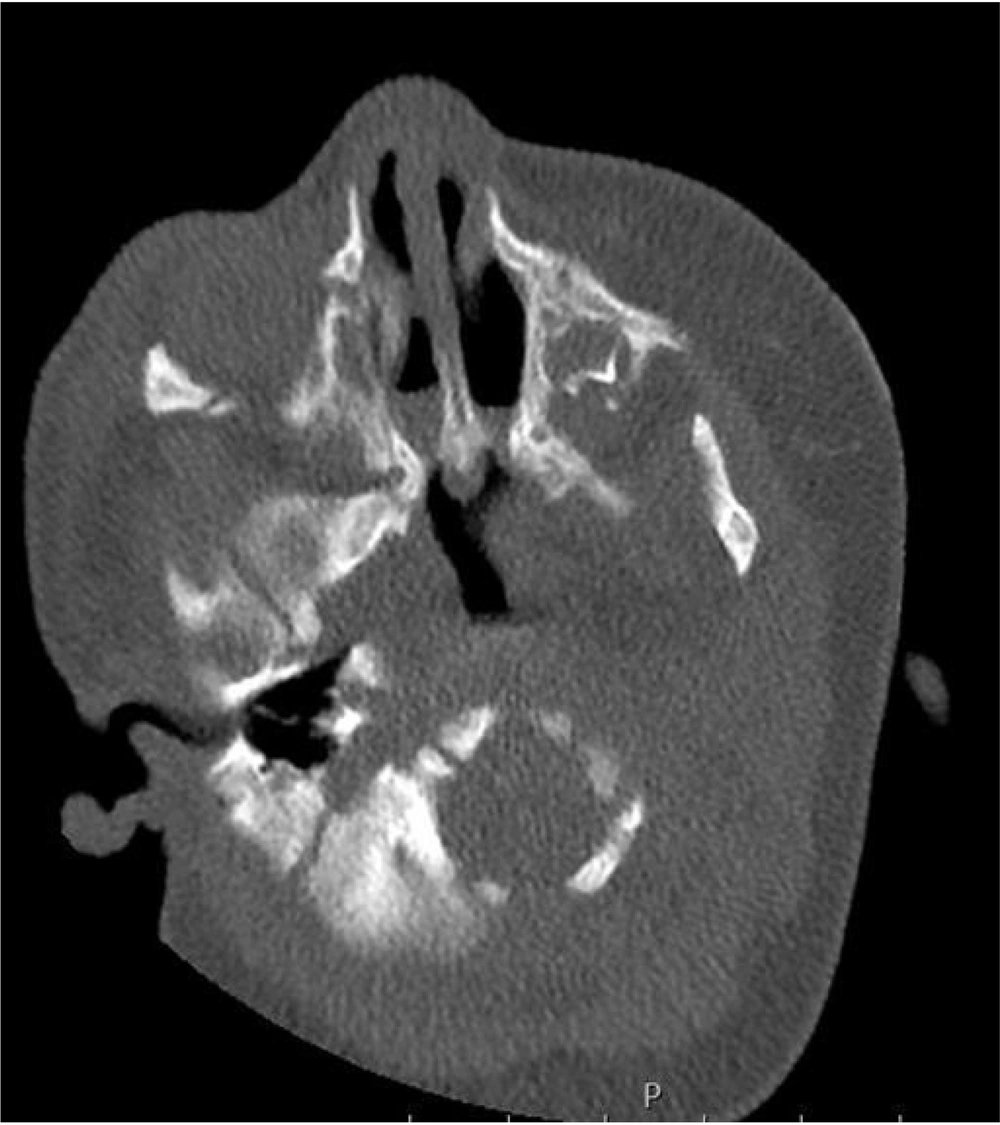
Non-contrast CT of the nasal cavity and nasopharynx was evaluated in all patients by taking 2 mm thick contiguous sections in the axial plane parallel to the hard palate. Before the examination, nasal passage aspiration and intranasal decongestant were applied to all patients to prevent errors caused by nasal secretions. To reduce motion artifacts, patients were either examined during sleep or administered intranasal midazolam (Dormicum) 0.2 mg/kg. In all patients, the examination was performed without contrast. The CT images were evaluated for the presence of choanal atresia, whether bilateral or unilateral type (bone, membranous, mixed), and middle nasal cavity stenosis (Figure 1). Craniofacial anomalies, if any, were also recorded on cranial CT. The medical information for accompanying syndromes was also reviewed (9).
3.5. Surgical Technique
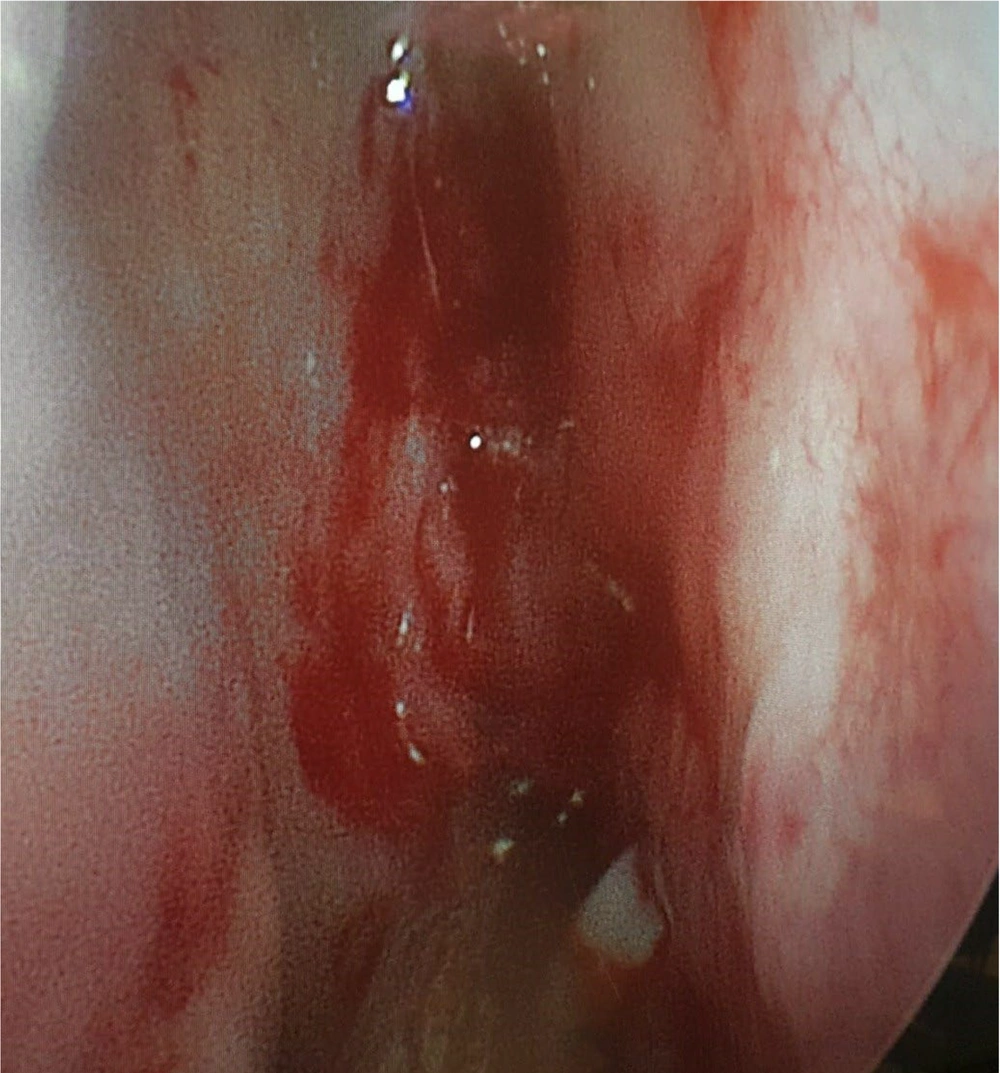
A vertical incision was made from top to bottom at the junction of the cartilage and bone, along the septal mucosa, approximately 5 - 10 mm in front of the atretic plate (Figure 2). The mucosal flap covering the nasal aspect of the thickened vomer and atretic plate was delicately lifted to safeguard the mucosa, ensuring the flap was collected intact. Following the excision of a portion of the pharyngeal aspect of the atresia plates, the thickened vomer and a segment of the lateral bone were carefully removed using pediatric back-biting forceps and a diamond burr. This procedure facilitated the connection of the neochoana to the midline. Upon achieving an appropriate expansion of the neochoana to 6 - 10 mm bilaterally, the preserved mucosal flap was shaped and fixed with a stent folded over the lateral and base raw bone regions.
A silicone splint was applied intraoperatively in all cases. Postoperative prophylactic antibiotic therapy, nasal saline solution, and intranasal antibiotic ointment were administered to all patients. Intranasal tampons were removed at the end of the 3rd week.
3.6. Postoperative Care and Evaluation
Families received instructions on nasal irrigation and scheduled follow-up appointments. The silicone stent remained in position for 3 weeks before being gently extracted from the nasal cavity under general anesthesia. Postoperative care consisted of saline irrigation, aspiration, and saline administration, as well as decongestant and corticosteroid nasal sprays. Routine widening of the stenosis was avoided to prevent the stimulation of granulation tissue formation. Patients were examined endoscopically when clinical symptoms of restenosis appeared. If the degree of stenosis was classified as C or D, nasal endoscopy was performed under general anesthesia, and granulation and scar tissue were removed. The narrowed neochoana was dilated or surgically re-expanded. All postoperative procedures performed under general anesthesia were considered revision procedures. Postoperative evaluations were made at the end of the 1st, 3rd, 6th, and 12th months after surgery.
3.7. Statistical Analysis
Statistical analyses were conducted using SPSS version 24.0 software (SPSS Inc.). G*Power v3.1.9.4 was employed for power analysis to determine sample size. Descriptive statistics, including numbers, percentages, medians (minimum-maximum range), means, and standard deviations (SD), were utilized. The normal distribution of variables was assessed through visual methods (histograms and probability plots) and the Kolmogorov-Smirnov test. Continuous variables were analyzed using either Student's t-test or Mann-Whitney U-test for two-group comparisons and the Kruskal-Wallis test for more than two-group comparisons, depending on the data's distribution and homogeneity. The Pearson chi-square test was applied for comparing categorical data. A significance level of P < 0.05 was considered statistically significant.
4. Results
A total of 40 patients were included in this study. Of these, 23 (57.5%) were female, and 17 (42.5%) were male, with a mean age of 90 days (range: 2 - 1650 days). The etiology of the cases was determined as bilateral choanal atresia in 57.5% (n = 23) and unilateral choanal atresia in 42.5% (n = 17) (Table 1). Among the cases with isolated choanal atresia, 14 had a pure bony atresia plate, 9 had a mixed type, and 17 had a membranous type. Revision surgery was required in 10% (n = 4) of the operated bilateral choanal atresia cases and in 7.5% (n = 3) of the unilateral cases. These revisions were due to restenosis caused by granulation tissue, with no other complications observed in the study.
| Variables | Bilateral Choanal Atresia (n = 23) | Unilateral Choanal Atresia (n = 17) | P-Value |
|---|---|---|---|
| Age (day) | 90 (720 - 30) | 60 (1650 - 2) | 0.72 b |
| Gender | 0.74 c | ||
| Male | 9 (39.1) | 8 (47.1) | |
| Female | 14 (60.9) | 9 (52.9) | |
| Gestational age (week) | 37.91 ± 1.92 | 37.23 ± 2,70 | 0.36 d |
| Birth Weight (gr) | 2836.52 ± 601.17 | 2978.23 ± 521,64 | 0.44 d |
| Duration of stay in inpatient service | 15 (90-1) | 2(15 - 1) | 0.001 b |
| Intensive care stay duration | 0 - 360 (30) | 0 - 45 (3) | 0.001 b |
| O2 need | |||
| Yes | 22 (87) | 8 (47.1) | 0.001c |
| No | 1 (13) | 9 (52.9) | |
| Malnutrition | 0.001 c | ||
| Yes | 20 (87) | 5 (29.4) | |
| No | 3 (13) | 12 (70.6) |
Demographic Data, Ward Stay, Intensive Care Stay, Oxygen Need and Nutritional Disorders Table a
In patients diagnosed with bilateral choanal atresia, oxygen dependency, malnutrition, length of intensive care unit (ICU) stay, and ward follow-up time were significantly prolonged (P < 0.05). The two groups (unilateral and bilateral) showed no significant differences in age, gender, gestational age, birth weight, or atresia type (P > 0.05) (Table 1). A subgroup analysis revealed no statistically significant differences in the duration of hospital stay based on the type of atresia (bony, mixed, or membranous) (P > 0.381). Patients whose hospital stays exceeded 30 days also had additional conditions, such as prematurity, low birth weight, and bronchopulmonary dysplasia.
For this study, a logistic regression model was developed to predict the log-odds of restenosis:
Indicating a linear relationship between the log-odds of restenosis and ICU stay, atresia type, gender, nutrition, and oxygen need. However, the analysis revealed no significant relationship between restenosis and any of these factors (Table 2).
| Variables | Coefficient | SE | P-Value a | Odds Ratio | 95% CI for Population Odds Ratio |
|---|---|---|---|---|---|
| Intensive care stay duration | -0.002 | 0.007 | 0.82 | 0.998 | 0.99 - 1.01 |
| Atresia Type (Reference Category ‘Mix’) | |||||
| Atresia type ‘bone’ | 0.54 | 1.30 | 0.68 | 1.72 | 0.13 - 22.06 |
| Atresia type ‘membranous’ | 1.55 | 1.40 | 0.27 | 4.73 | 0.31 - 73.05 |
| Sex (reference category ‘female’) | 0.95 | 0.99 | 0.33 | 2.60 | 0.38 - 17.95 |
| Nutrition (1) | 1.89 | 1.15 | 0.10 | 6.60 | 0.69 - 62.94 |
| O2 (1) | -1.40 | 1.36 | 0.30 | 0.25 | 0.02 - 3.52 |
A Logistic Regression Model for Log-odds of Recurrence
5. Discussion
Choanal atresia is a congenital anatomic anomaly with high mortality rates in newborns when emergency intervention is not made, and it is a clinical condition that can result in death due to recurrences, or even after surgery (10). This study is one of the few studies in the literature showing that the use of the Septonasal flap technique in cases of choanal atresia reduces recurrences. Ekşioğlu et al. reported that 57% of their cases had bilateral choanal atresia and 43% had unilateral choanal atresia (11). Similarly, the current study found that 57.5% of the cases had bilateral choanal atresia and 42.5% had unilateral choanal atresia.
Although various techniques and approaches for correcting congenital choanal atresia have been extensively documented, a consensus on the recommended surgical techniques has not been reached, as most studies rely on case series with limited sample sizes or consensus recommendations (12, 13).
In the current study, endoscopic choanal atresia surgery was performed on all patients using the Septonasal flap technique. In this technique, a wider choanal opening was obtained by performing partial resection of the posterior nasal septum together with the removal of the atretic plate. Silicone stents were placed in all patients and left for an average of 3 weeks. Restenosis was observed in 4 of 23 cases with isolated bilateral choanal atresia, one of which was a revision case. In these cases, the success rate was 82.7%. We think that the low restenosis rates in our case are related to the protection of the mucosa due to the Septonasal flap technique that we used. In 17 cases with unilateral choanal atresia, the success rate was 82.4%. Similar to our study, in a study by Wang et al. (14), the procedure involved the utilization of the endoscopic Septonasal flap technique along with the application of bioabsorbable steroid-eluting stents for repairing congenital choanal atresia. In this study, a restenosis rate of 9.1% in patients with silicone stent implantation was reported, while various complications such as granulation, columella damage, and posterior septal injury were observed in 13.6%. The mucosa was preserved using the Septonasal flap technique that we applied. Additionally, the prolonged presence of the silicone stents prevented secondary granulation and inflammation from closing the new choanal opening in the nasal passage. As a result, we found that restenosis rates were significantly reduced compared to other techniques.
Diverse studies have observed a prevalence ranging from 12% to 54.7% of cases necessitating secondary surgical intervention, primarily due to the persistence of restenosis following surgery, a frequent complication of endoscopic congenital choanal atresia repair (15). Factors associated with an increased risk of restenosis include age, weight, bilateral choanal atresia, failure to achieve smooth nasal patency, and excessive granulation tissue growth on denuded bone (16).
At the end of the procedure, the preservation of the mucosa in the form of a flap placed over the exposed bony walls of the neochoana helps prevent restenosis. According to Strychowsky et al.'s meta-analysis, the success rate of transnasal endoscopic choanoplasty, determined based on the presence of restenosis or the need for revision, is 65% (17). Possible risk factors for restenosis include associated congenital abnormalities, reflux of gastric contents into the nasopharynx, and the neonate's age being less than 10 days, as younger age is associated with more unfavorable anatomical conditions that limit the visibility and extent of resection (18). The reduction of restenosis rates following surgery in these patients remains a topic of discussion. Two major controversies in the surgical correction of congenital choanal atresia concern the utilization of stenting post-surgery and the utilization of flaps to cover peeled bone. Each technique has its own set of advantages and disadvantages, yet consensus on the optimal approach remains elusive. Postoperative restenosis continues to be a common complication of endoscopic repair for congenital choanal atresia (14). In the surgical approach to the treatment of choanal atresia, the use of transnasal, trans-septal, and transpalatal techniques, each with its own advantages and disadvantages, should always be applied, taking into account the patient's age and the complexity of the associated malformation (19). Various authors have noted that endoscopic transnasal (ETN) repair is safe and efficient, yielding favorable outcomes with or without stenting (20). Strychowsky et al. (17) reported surgical success rates ranging from 67% to 88% for the ETN approach. In the study by De Freitas et al. (21), a meta-analysis comprising 20 studies showed that the ETN approach had an average success rate of 85.3% (22). In a study by De Vincentiis et al., involving 17 cases of bilateral and 29 cases of unilateral choanal atresia, transnasal endoscopic surgery with mucosal flaps followed by balloon dilation was performed, and no stents were used in any of the patients. It was stated that 82% of bilateral cases and 93% of unilateral cases did not require restenosis and repeat surgery. It was concluded that the utilization of stents should be avoided and the use of balloon dilatation reduced relapse (19). In a study by Gülşen et al., 48 patients underwent endoscopic choanal atresia surgery. After the 6-month follow-up period, the success rate stood at 70.8% (23). Eladl and Khafagy (24) investigated 112 cases of bilateral choanal atresia that underwent transnasal endoscopic repair and noted a restenosis rate of 42%, providing a success rate of 58%. In this study, the incision is prolonged to the atretic plate of atresia, followed by the excision of the mucosa covering it. In that study, there was also no difference in the 1st revision surgery rates between unilateral and bilateral choanal atresia cases, but the 2nd (P = 0.004) and 3rd (P < 0.001) revision surgery rates for bilateral choanal atresia were statistically significantly higher. Likewise, Kinis et al. (25) noted the success ratio of the ETN procedure in 33 cases with choanal atresia, revealing a restenosis rate of 53.8% for bilateral cases of choanal atresia and 23.1% for unilateral cases. In this study, mucoperiosteal flaps were not formally elevated.
In the study by Ferlito et al., 38 cases of choanal atresia were analyzed. Normal postoperative recovery was observed in 18 (47.36%) cases, moderate restenosis in 8 (21.05%) cases, and severe (>50%) stenosis requiring surgery was reported in 12 (31%) cases (26). Restenosis may occur due to excessive proliferation of granulation tissue and the formation of fibrotic scars, particularly as a result of aggressive drilling. To prevent that possibility, ensuring maximal coverage of the raw bone with healthy epithelium and avoiding significant injury to the mucosa can aid in preserving the openness of a posterior congenital choanal atresia reparation. Preserving the mucosa for use as flaps is important to prevent restenosis (14).
In choanal atresia cases, 4 of the cases that developed postoperative recurrence were bone atresia, 2 were membranous atresia, and 1 was mixed-type atresia. It was observed that there was no relationship between restenosis and atresia type.
While numerous studies advocate for stenting, some authors argue that stenting can result in complications like stenosis, columellar ulceration, septal perforation, stent occlusion secondary to granulation, and bacterial resistance development due to prolonged use of antibiotics.
These authors have expressed dissenting views regarding the use of stents following transnasal endoscopic stenosis repair; hence, stenting is considered to be a significant contributor to granulation formation (12). A study conducted by Cedin et al. (27) demonstrated that an expedited improvement period resulted in decreased granulation tissue formation, and a decrease in stenosis was observed in patients who did not receive stenting. Another study by Gosepath et al. (28) concluded that the primary factor contributing to stenosis is the development of granulation tissue following stent placement. They reported a stenosis ratio of 35% in the stented group, compared to 11% in the nonstenting group.
In the current study, we used stents in all the cases we operated on. No stent-related infections were observed. Restenosis developed due to granulation tissue in 7 cases (17.5%). Among the 40 patients included in our study, stents were used in all of them. In the postoperative period, stenosis developed in 7 out of 40 patients with choanal atresia (17.5%). The surgical success rate achieved was 82.5%, which is comparable to the rates reported in the literature. We used stents in all our cases. When we look at our cases that developed recurrence, it was found that most of them had bone atresia. Wang et al. reported various complications such as granulation, columella damage, and posterior septal injury were observed in 13.6% (14).
We also advocate for the utilization of endoscopic approaches whenever feasible. These methods facilitate the re-establishment of nasal openness by utilizing the natural airway, thereby minimizing the need for detachment of the palatal fibromucosa. This approach consequently reduces the risks associated with lesions located on the palatal pedicle and complications related to wound healing. Additionally, optical magnification of the surgical site enables complete excision of the atretic plate. Endoscopic techniques result in shorter surgical durations, minimal bleeding, early feeding post-surgery, and shorter hospital stays (6).
We acknowledge that a limitation of our study is the small sample size. Nevertheless, in this paper, we aim to demonstrate the results of endoscopic repair of bilateral congenital choanal atresia utilizing a mucoperiosteal flap with stenting. There is a necessity for additional studies involving larger patient populations and longer follow-up durations to make more substantial contributions to the existing literature. Since only the Septonasal flap technique with stent is applied in our clinic, a comparison could not be made with examinations without stent.
5.1. Limitations
The limitations of our study are that it is single-center, lacks a control/comparison group (e.g., different surgical techniques), and has a relatively short follow-up period for some patients.
5.2. Conclusions
Silicone stents can help prevent potential complications or restenosis by providing an opportunity for the treatment and aspiration of secretions. When used appropriately, they can reduce the likelihood of restenosis or complications in patients. Opening the atresia by applying the Septonasal flap technique together with silicone stent application in surgery reduces the rate of restenosis in the long term. Nevertheless, there is a need for further studies with larger numbers of patients with longer follow-up periods to be able to contribute more to the literature. Multi-center studies, comparison group (e.g., different surgical techniques) studies, and relatively long follow-up period studies have been suggested for further research.