1. Background
Acute appendicitis is the most common cause of surgical acute abdominal pain worldwide, typically occurring between the ages of 10 and 20 years (1). This condition is characterized by an acute onset, rapid disease progression, and marked abdominal signs, with clinical manifestations that can vary over time, often necessitating urgent surgical intervention (2). A periappendiceal abscess is a complication that arises when acute appendicitis does not receive timely and effective therapeutic intervention, leading to the appendix becoming encased in greater omental adhesions, forming an inflammatory mass that may progress to gangrene, perforation, and severe peritonitis (3). This abscess, one of the known complications of appendicitis, accounts for approximately 9.7% of acute appendicitis cases in children (4). Although advancements in imaging and ultrasound have simplified the diagnosis of periappendiceal abscesses, the choice of treatment remains highly controversial (5).
Treatment options for appendiceal abscesses in children include surgical and conservative methods (6). Surgical treatment typically involves laparoscopic or open removal of the appendix and evacuation of pus from the abdominal cavity. This method can completely remove the primary lesion and eliminate the source of infection, potentially providing a one-time cure. It is also effective in reducing hospitalization time and costs to a certain extent (7, 8). However, surgical treatment carries risks, including surgical trauma and anesthesia-related complications, with a high likelihood of issues such as incision infection, blood seepage, residual infection in the abdominal cavity, postoperative intestinal adhesions, and intestinal obstruction (9).
In contrast, conservative treatment employs non-surgical methods such as antibiotics and intravenous fluids, which are generally safer than surgical interventions (10). Clinical practice has shown that early use of antibiotics can quickly reduce inflammation, aid in restoring the appendiceal structure and function, and effectively decrease the risk of complications such as incision infection and intestinal obstruction (11).
Within the conservative therapeutic paradigm, antibiotics are utilized across various clinical scenarios, including preoperative administration, concurrent with medical interventions, or as a sustained regimen throughout the treatment course. However, conservative treatment carries a certain probability of recurrence, potentially prolonging the duration of the illness and increasing the recurrence rate in children (12). Consequently, the necessity of an appendectomy in these cases remains unclear.
Studies have identified several factors associated with the recurrence of periappendiceal abscesses (13-16). Castello et al. determined that indications for interval appendectomy in children include persistent symptoms following abscess resolution, slow abscess resolution, a history of previous episodes of appendicitis, and ultrasound evidence of a fecalith (13). Chang et al. identified elevated C-reactive protein (CRP) levels as a risk factor for the recurrence of periappendiceal abscesses in children (14). The aim of the present study is to analyze the risk factors for the recurrence of periappendiceal abscesses in children following conservative treatment, utilizing hospital case data.
2. Objectives
This investigation aims to improve predictability and support clinicians and emergency departments in their decision-making process.
3. Methods
3.1. Participants
This retrospective study gathered case data of children admitted to the Department of Paediatric Surgery in our hospital with acute appendicitis-related periappendiceal abscesses between 1 January 2015 and 31 December 2021. After a 2-year outpatient follow-up, the study population was selected based on specific inclusion and exclusion criteria. Data were collected from children who underwent conservative treatment, including information on the child’s gender, age, duration of hospitalization, white blood cell (WBC) count, CRP levels, and imaging findings at admission and 1 day prior to discharge. The study received approval from the hospital’s ethical committee, and informed consent was obtained from the families at the time of follow-up.
The inclusion criteria were as follows: (1) patients with a history of right lower abdominal pain; (2) routine blood tests indicating elevated WBC count and increased CRP levels, with a diagnosis of appendicitis with a periappendiceal abscess confirmed by ultrasound or computed tomography (CT); and (3) clinical symptoms and test indicators returned to normal following conservative treatment with antibiotics. The exclusion criteria were: (1) children discharged with persistent clinical symptoms and test indicators not showing a decreasing trend and non-compliance with medical advice; (2) children initially diagnosed with a periappendiceal abscess but later diagnosed with other diseases; (3) children with a periappendiceal abscess co-existing with other immunodeficiency diseases; and (4) patients who underwent surgery or drainage for a periappendiceal abscess caused by acute appendicitis.
3.2. Treatment Plans Selected
Two physicians will conduct a comprehensive clinical assessment, including evaluating symptoms, signs, inflammatory markers, and imaging findings. This approach helps determine the severity of the abscess and the patient’s overall health status. In this study, the patients did not present with severe symptoms such as high fever or intense abdominal pain, and the abscesses were relatively small, suggesting that treatment with oral antibiotics might be appropriate. Antibiotics are typically prescribed to control the infection and prevent the spread of abscesses. Imaging examinations, such as ultrasound, CT scans, or magnetic resonance imaging, are used to confirm the location, size, and morphology of the abscess, as well as to assess for appendicitis or other complications.
Deciding on the treatment approach for a periappendiceal abscess is a comprehensive process that involves assessing and balancing multiple factors. When formulating a treatment plan, physicians consider these factors holistically and work collaboratively with the patient to reach a consensus (17). In cases where the two physicians disagree, a third senior chief physician will make the final decision on which treatment measure to adopt.
3.3. Outcomes
The size of the patient’s abscess was defined by the largest diameter in centimeters as measured on ultrasound imaging (13). Before initiating the study, the children’s parents were contacted by phone to determine whether there had been any relapse following discharge. Ultrasound imaging was used as part of the criteria for defining "recurrence," which was characterized by the return of abdominal pain and signs of fixed right lower abdominal pressure and rebound pain in children, accompanied by ultrasound images showing hypoechoic or anechoic areas in the right lower abdomen. From the collected cases, children who were hospitalized two or more times due to recurrent periappendiceal abscesses were categorized into the recurrence group. All children who did not experience a recurrence of a periappendiceal abscess or acute appendicitis without an abscess during the study period were classified as non-recurrent and included in the non-recurrent group.
3.4. Data Analysis
Statistical analysis was conducted using SPSS 25.0 for Windows (SPSS Inc, Chicago, Illinois, USA). The Kolmogorov–Smirnov test was used to assess all continuous variables for normality. Data conforming to a normal distribution were presented as mean ± standard deviation (x̄ ± s) and analyzed using the t-test. Non-normally distributed data were described using the median (P25, P75) and compared using the Wilcoxon rank-sum test. Group comparisons of categorical data were made using the chi-square (χ²) test. When the conditions for the χ² test were not met, Fisher’s exact probability method was applied. Logistic regression analysis was performed on variables that showed statistically significant differences in the univariate analysis to identify independent predictors of recurrence. A P-value of < 0.05 was considered statistically significant.
4. Results
4.1. Treatment
Conservative treatment, using simple antibiotics, was adopted. This involved superficial upper extremity vein puncture, tube placement, and intravenous antibiotic infusion. The chosen antibiotic regimen (17), either a two-drug combination (cephalosporins with metronidazole or piperacillin with metronidazole) or a three-drug combination (cephalosporins and penicillin with metronidazole), was prescribed based on the child’s general condition and abdominal signs. The dosage for cephalosporin and piperacillin antibiotics was 50 mg/kg twice daily, while the metronidazole dose was 7.5 mg/kg every 8 hours.
The child’s condition was assessed daily for changes. Intravenous antibiotic treatment continued if there was a decrease in abdominal pain, reduced or absent pressure in the right lower abdomen, and improvement in clinical symptoms within the first 2 - 3 days of treatment. The total duration of antibiotic use did not exceed 14 days. Discharge criteria included being fever-free for 48 hours, improvement in abdominal signs and symptoms, and a decrease in WBC and CRP levels. Post-discharge, cefixime granules were prescribed as an oral antibiotic at a dose of 100 mg (for body weight ≥ 30 kg) or 1.5 - 3 mg/kg (for body weight ≤ 30 kg) twice daily for 1 week, following infectious disease recommendations. After 3 months of follow-up, the periappendiceal abscess had resolved, and the patient achieved full recovery.
4.2. Clinical Indicators of Children in Both Groups
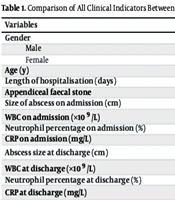
This study included a total of 65 children who successfully received their first conservative treatment. Among them, nine (13.85%) experienced a relapse and developed clinical manifestations of a periappendiceal abscess following discharge. Table 1 illustrates the differences in all descriptive indicators between the non-recurrent and recurrent groups.
| Variables | Non-recurrence Group (n = 56) | Recurrent Group (n = 9) | χ2/t/Z | P-Values |
|---|---|---|---|---|
| Gender | 0.012 | 0.912 | ||
| Male | 30 | 5 | ||
| Female | 26 | 4 | ||
| Age (y) | 6.71 ± 3.48 | 7.22 ± 3.83 | -0.401 | 0.690 |
| Length of hospitalisation (days) | 11.18 ± 3.25 | 13.67 ± 7.94 | -0.928 | 0.379 |
| Appendiceal faecal stone | 20 (35.71%) | 5 (55.56%) | 1.290 | 0.256 |
| Size of abscess on admission (cm) | 21.80 (17.77, 34.45) | 22.80 (17.42, 35.73) | -0.199 | 0.842 |
| WBC on admission (×109 /L) | 18.88 (13.25, 22.53) | 15.99 (12.60, 21.73) | -0.636 | 0.525 |
| Neutrophil percentage on admission (%) | 77.60 (70.60, 80.30) | 75.80 (72.00, 79.60) | -0.418 | 0.676 |
| CRP on admission (mg/L) | 80.50 (51.30, 104.80) | 50.0 0 (29.00,122.50) | -0.836 | 0.403 |
| Abscess size at discharge (cm) | 2.80 (1.42,4.26) | 6.50 (2.00,8.56) | -2.298 | 0.022 a |
| WBC at discharge (×109 /L) | 6.98 (6.34,7.53) | 13.25 (6.50, 17.82) | -2.412 | 0.016 a |
| Neutrophil percentage at discharge (%) | 45.80 (45.30, 46.60) | 48.70 (43.80, 50.80) | -0.846 | 0.398 |
| CRP at discharge (mg/L) | 8.60 (8.30, 10.60) | 32.80 (16.10, 74.50) | -3.031 | 0.002 a |
Comparison of All Clinical Indicators Between the Two Groups
Upon admission, no significant difference was observed in the mean length of hospital stay between the non-recurrent and recurrent groups (11.18 ± 3.25 vs. 13.67 ± 7.94 days, P = 0.379). The number of children with appendiceal fecaliths was 20 (35.71%) in the non-recurrent group and five (55.56%) in the recurrent group (P = 0.256). However, no significant differences were found in the mean size of the abscesses (21.80 vs. 22.80 cm, P = 0.842), mean WBC count (18.88 × 109/L vs. 15.99 × 109/L, P = 0.525; normal value: 4 - 10 × 109/L), mean neutrophil percentage (77.6% vs. 75.80%, P = 0.676), and mean CRP levels (80.5 vs. 50 mg/L, P = 0.403; normal value: 0 - 10 mg/L).
Three days before discharge, significant differences were observed in the mean size of the abscess (2.80 vs. 6.50 cm, P = 0.022), mean WBC count (6.98 × 109/L vs. 13.25 × 109/L, P = 0.016), and mean CRP levels (8.60 vs. 32.80 mg/L, P = 0.002) between the non-recurrent and recurrent groups. However, there was no significant difference in the mean neutrophil percentage at discharge (45.80% vs. 48.70%, P = 0.398).
In summary, at the time of discharge, there were statistically significant differences between the two groups in terms of abscess size, WBC count, and CRP levels (P < 0.05); however, no significant differences were observed in other clinical indicators (P > 0.05). For more details, refer to Table 1.
4.3. Multifactorial Logistic Regression Analysis of Recurrence Following Resolution of Clinical Symptoms of Periappendiceal Abscesses in Children
This study evaluated the recurrence of periappendiceal abscesses in children following conservative treatment, using multifactorial logistic regression analysis. The recurrence status was treated as the dependent variable (coded as ‘0’ for non-recurrence and ‘1’ for recurrence). Independent variables included the size of the abscess, WBC count, and CRP levels at discharge, all of which showed significant differences between the groups.
The analysis revealed that WBC counts at discharge [odds ratio (OR) = 1.522, 95% CI = 1.096 - 2.114] and CRP levels at discharge (OR = 1.136, 95% CI = 1.023 - 1.262) were independently associated with the recurrence of periappendiceal abscesses. Specifically, higher WBC and CRP values at discharge were correlated with an increased likelihood of recurrence in children following the resolution of clinical symptoms. For more details, refer to Table 2.
Multifactorial Logistic Regression Analysis of Recurrence After Successful Conservative Treatment of Periappendiceal Abscess in Children
4.4. The Clinical Data of Nine Patients in the Recurrence Group
The clinical characteristics of patients in the recurrence group were analyzed. Table 3 presents the demographic and clinical data of the nine patients who experienced recurrence following conservative treatment for periappendiceal abscess. Among the patients in the recurrence group, ages ranged from 37 to 156 months, with a median age of 71 months. The recurrence interval varied widely, from 15 to 260 days, with a median recurrence interval of 100 days. Most patients underwent surgical intervention, either alone or in combination with conservative treatment, for their recurrence. The time from symptom onset to hospital admission ranged from 3 to 14.5 days, with a median of 5 days. Hospitalization durations varied from 5 to 29 days, with a median hospital stay of 12 days. The size of the abscesses ranged from 4.94 to 57 mm, with a median size of 22.8 mm. White blood cell counts at discharge ranged from 7.12 × 10⁹/L to 28.96 × 10⁹/L. Additionally, CRP levels, a marker of inflammation, were measured, with values ranging from 30 to 134 mg/L. These findings provide insight into the clinical characteristics of pediatric patients experiencing recurrence following conservative treatment for a periappendiceal abscess.
| Gender | Age (mon) | Recurrence Interval (Days) | Post Treatment of Recurrence | Time from Onset to Admission (Days) | Hospitalization Time (Days) | Size of Abscess (mm) | White Blood Cell Count | Recurrent White Blood Cell Count | CRP |
|---|---|---|---|---|---|---|---|---|---|
| F | 147 | 75 | Conservative + surgical | 7 | 9 | 57 | 28.96 | 10.69 | 88 |
| F | 132 | 124 | Surgical | 3 | 9 | 20.9 | 12.49 | 15.36 | 30 |
| M | 64 | 34 | Conservative | 6 | 29 | 38.35 | 12.62 | 10.54 | 134 |
| M | 37 | 100 | Conservative | 5 | 25 | 22.8 | 23.76 | 20.26 | 45 |
| M | 37 | 128 | Conservative | 3.5 | 12 | 33 | 17.58 | 13.9 | 111 |
| F | 71 | 102 | Surgical | 5 | 12 | 14 | 15.99 | 20.53 | 50 |
| F | 89 | 260 | Surgical | 14.5 | 5 | 29.25 | 21.95 | 14.04 | 64 |
| M | 63 | 20 | Conservative + surgical | 9 | 12 | 4.94 | 18.6 | 19.72 | 89 |
| M | 156 | 15 | Surgical | 5 | 10 | 22.4 | 7.12 | 17.37 | 103 |
Clinical Characteristics of Patients in the Recurrence Group
5. Discussion
A periappendiceal abscess refers to an abscess or inflammation that forms around the appendix in cases of acute appendicitis. This condition can result from the spread of appendiceal inflammation to surrounding tissues or from the formation of fibrous adhesions and macroscopic omental encapsulation around the appendix, which is a reaction of the body’s defense mechanism. Periappendiceal abscesses are predominantly managed with conservative treatment, which is considered both safe and effective (3, 18). The preference for conservative treatment may be attributed to the observation that surgical intervention during the peak of the inflammatory process in appendicitis can lead to over-activation of the cytokine cascade, a response linked to various postoperative complications. In contrast, conservative treatment can limit the inflammatory response and allow time for intestinal recovery (19, 20).
The present study reported a recurrence rate of 13.85% in children following the resolution of clinical symptoms of periappendiceal abscesses, a figure higher than previously reported in studies focusing on non-surgical treatment (5% - 13.6%) (14, 21). This increased rate may be associated with the fact that our study population consisted of children, who typically have an immature immune system and comparatively weaker resistance (22). Appendiceal fecal stones have been identified as an independent risk factor for the recurrence of periappendiceal abscesses (13, 23). Castello et al. analyzed the case data of 41 children diagnosed with a periappendiceal abscess and treated conservatively. The authors found that 13 children experienced recurrence and concluded that the presence of appendiceal fecal stones in children with periappendiceal abscesses substantially increases the likelihood of recurrence (13). Tanaka et al. demonstrated that children with periappendiceal abscesses and appendiceal fecal stones were more likely to require surgical intervention or readmission to the hospital compared with those without such stones, indicating that appendiceal fecal stones are also a broader predictor of recurrence in periappendiceal abscesses (23). However, the present study did not find a significant difference in the presence of appendiceal fecal stones between the two groups (35.71% vs. 55.56%, P = 0.256). This discrepancy could be due to individual differences, and it has been suggested that fecal stones may dissolve and be absorbed following the resolution of the clinical symptoms of periappendiceal abscesses.
In addition, the necessity of interval appendectomy following conservative treatment of a periappendiceal abscess remains a topic of substantial discussion. In recent years, there has been ongoing debate regarding interval appendectomy, with some studies suggesting that it may not always be necessary after the successful nonoperative management of a periappendiceal abscess (24). However, the decision to perform an interval appendectomy should take into account various factors, including the patient’s clinical condition, the risk of recurrence, and potential complications associated with appendectomy (25).
The results of the present study indicated no significant difference in WBC count between the two groups of children upon admission. However, a significant difference in WBC count at discharge was observed. In this study, WBC count at discharge was identified as an independent factor influencing the recurrence of periappendiceal abscesses. This finding aligns with the results of Nazarey et al. (26), who reported that a WBC level of > 15 × 10⁹/L is associated with a higher risk of recurrence. Similarly, Lou et al. (27) identified a WBC count of > 8 × 10⁹/L at discharge as an independent risk factor for recurrence. Lee et al. (28) highlighted that children with a poorly defined and large periappendiceal abscess face a substantially increased risk of recurrence.
In the present study, while a significant difference in abscess size at discharge was noted between the two groups of children, the logistic regression analysis did not identify abscess size at discharge as an independent factor influencing recurrence. This could be due to bias from other interfering factors in the univariate analysis or errors related to the small sample size. Therefore, further studies are needed to confirm the relationship between abscess size and the recurrence of periappendiceal abscesses.
Furthermore, the present study revealed no substantial difference in CRP levels at admission; however, a marked difference was noted in CRP levels at discharge between the two groups of children. Logistic regression analysis indicated that CRP level at discharge is an independent predictor of periappendiceal abscess recurrence. Miyauchi et al. found that CRP is a significant indicator of appendicitis severity, with a CRP level ≥ 34.6 mg/L increasing the likelihood of appendiceal perforation (29). Similarly, Chang et al. (14) analyzed the medical records of 70 children with periappendiceal abscesses and determined that a CRP level ≥103 mg/L substantially elevates the risk of recurrence. Zhou et al. also concluded that CRP is a more precise predictor of complicated appendicitis, noting that CRP levels escalate as the severity of appendicitis intensifies (30).
Therefore, for children presenting with high CRP and WBC levels without evidence of complications such as a periappendiceal abscess or generalized peritonitis, initial treatment with antibiotics may be advisable. This approach involves administering antibiotics to control the infection, coupled with close monitoring for clinical improvement. If the patient exhibits a favorable response to antibiotic therapy and shows signs of improvement, surgery may be avoidable. However, if there are indications of worsening infection, the development of complications, or a lack of improvement with antibiotic therapy, surgical intervention might become necessary. In these situations, an appendectomy could be recommended to remove the inflamed appendix and prevent further complications.
Following discharge, maintaining close patient follow-up is critical, with vigilant monitoring of WBC counts (≥ 13 × 10⁹/L) and CRP levels (≥ 32 mg/L). Ideally, this should be done through ultrasound examinations to assess the resolution of the abscess. If these biomarkers do not normalize or if the abscess does not resolve within the prescribed 2-week antibiotic course, readmission for further treatment is advisable to mitigate the risk of abscess recurrence. Emergency medicine providers can expedite treatment decisions based on the patient’s past medical history and inflammation indicators from the last discharge, thereby saving valuable treatment time.
This study has several limitations. First, it was a single-center retrospective study with a small sample size. The number of children in the recurrence group was particularly limited, due to both the small number of participants and the inherently low risk of recurrence of periappendiceal abscesses. Therefore, future research should involve a multi-center prospective study with a larger sample size for verification. Second, there is potential for unavoidable bias in measuring abscess size due to variations among different sonographers. Additionally, as one of the potential risk factors, the microbiological profile and antibiotic resistance patterns were not considered in this study. Finally, imaging findings should be included in future research to provide valuable insights into the factors influencing recurrence risk.
5.1. Conclusions
In this study, the recurrence rate of periappendiceal abscesses in children following the resolution of clinical symptoms was found to be 13.85%. Additionally, both WBC and CRP levels at discharge were independently associated with the recurrence of periappendiceal abscesses. Therefore, in clinical practice, it is recommended that patients should not be discharged until their WBC and CRP levels have decreased to normal values (or are sufficiently low). If a patient must be discharged due to financial constraints or other pressing reasons, heightened attention should be given to the risk of recurrence in pediatric patients with elevated WBC and CRP levels at discharge. It is also crucial to provide comprehensive return precautions and educate parents about the importance of promptly returning to the emergency department if acute abdominal pain recurs.