1. Background
Despite the strong desire to initiate early enteral feeding in all neonates (1), there is still a significant need for long-term and safe vascular access to avoid multiple unsuccessful intravenous insertion attempts. These attempts can cause significant stress, pain, infections, and other complications for these patients. The insertion of peripherally inserted central catheters (PICCs) has made it possible for the sickest and most premature neonates (preemies) to survive (2). All PICC line placement methods involve estimating the appropriate insertion length to achieve optimal catheter tip position. According to the National Association of Neonatal Guidelines, the initial calculation of catheter insertion length in the upper extremities (UE) involves measuring the distance between the catheter insertion sites along the normal vein pathway to the right sternal border, aligned with the third intercostal space. If the PICC line is being inserted through a brachial vein, the arm should be positioned at a 90-degree angle for measurement, along the normal vein pathway, while the limb is in its most relaxed position. For lower extremity (LE) insertion, the distance between the catheter insertion site and the right of the umbilicus, aligned with the xiphoid, should be measured (3). Traditionally, the evaluation of the catheter tip position is performed using a chest X-ray.
The classification of catheter placement is as follows:
(1) Right placement: In the case of UE and head and neck (H&N) PICC lines, the catheter terminates in the superior vena cava (SVC) before the right atrium, aligned with T2-T4. For LE PICC lines, the catheter terminates in the inferior vena cava (IVC) at the diaphragmatic level, aligned with T10 (4).
(2) Peripheral placement: In UE PICC lines, the catheter tip is located in the subclavian and brachiocephalic veins. In H&N PICC lines, the catheter tips terminate in the jugular vein. In LE PICC lines, the catheters terminate in the iliac vein. Although the catheter tips are not placed in central lines, these placements are considered usable as peripheral catheters based on the protocols of each Neonatal Intensive Care Unit (NICU) (5).
(3) Malposition: Malposition occurs when the catheter tips in UE PICC lines are placed in the jugular vein or right ventricle. In LE PICC lines, malposition is classified when the catheter tips are placed in the renal and ascending lumbar veins or right atrium (3). Catheter malposition is always unpleasant, even for nurses. Many catheter complications are a result of malposition. There are several factors related to PICC malposition. Recognizing and addressing these factors can help reduce the incidence of catheter complications (6).
2. Objectives
The objective of this study was to compare the catheter tip position and the extent of catheter tip correction required in PICC lines placed in the H&N, UE, and LE in the NICU of Children's Medical Center. Additionally, we assessed the incidence of complications and the survival rate of PICC lines in these three groups. The findings of this study aim to offer a recommendation to the treatment team for selecting the appropriate insertion length of the PICC line for each patient. This knowledge can help minimize the adverse effects of this technique in various NICUs and enhance the understanding of staff and physicians regarding the complications associated with different types of PICC lines and their durability (survival rate).
3. Methods
This cross-sectional study was conducted in the NICU of the Children's Medical Center. The study population consisted of all neonates who were eligible for PICC line placement between 2020 and 2021. Detailed information about the study process was provided to the parents, and informed consent was obtained from them before their neonates were included in the study. The inclusion criteria for this study were as follows: All neonates admitted to the NICU who required PICC line placement for any reason, such as a birth weight less than 1500 grams, the need for hyperosmolar or non-physiologic pH medications, the requirement for IV therapy, total parenteral nutrition (TPN), antibiotic therapy, or oral feeding intolerance lasting more than 6 days.
- Neonates meeting any of the following criteria were excluded from the study:
(1) Presence of contraindications for PICC placement, such as burns, venous thrombosis vulnerability in neonates with coagulopathies, or local dermatitis or hematoma that hindered peripheral vein access, or in cases where the catheter position could not be confirmed with X-rays.
(2) Neonates with blood culture-positive sepsis before treatment (5, 7).
In this study, single-lumen silicone PICCs (Vygon GmbH & Co. KG, Germany) with 1 or 2 French catheters were aseptically inserted by two skilled, trained, and experienced nurses using the Seldinger technique (8). The site of PICC line placement (H&N, UE, or LE) was documented for each participant. The initial insertion length of the PICC line catheter and the appropriate patient position for correct catheter insertion were determined based on the guidelines provided by the National Association of Neonatal Nurses (3). To confirm and evaluate the catheter tip position and its appropriate placement, radiography was performed and interpreted by a radiologist. The radiologists interpreting X-rays were blinded to the insertion site. If any catheter malposition was identified, the catheter was retracted to achieve the correct position. The amount of correction made to the insertion length was also recorded.
To assess inter-rater reliability for catheter position, we provided training to two nurses who evaluated catheter positions. This training focused on the standardized assessment protocol, criteria for determining catheter tip position, and any relevant imaging interpretation skills. We conducted a pilot test with a small group of healthcare providers to ensure that they understood and could apply the standardized assessment protocol consistently (3, 9).
Based on Elmekkavi's research data, study design, and sample size calculation formula (10), the initial sample size for this study was determined to be 328 neonates. However, during the study, the final sample size increased to 368 neonates, which were included in the analysis. Demographic characteristics of the neonates, including gestational age, weight, gender, and the etiology of their underlying diseases, were obtained by reviewing the neonates' medical records. This information was recorded in pre-prepared questionnaire forms. Additionally, the PICC line's information was collected. These include the initial insertion length of the catheter, site of catheter insertion, catheter tip position and location as reported in radiologic reports, the amount of correction needed for the inserted length of the catheter, duration of PICC line usage, the cause of catheter removal, and PICC line complications. The PICC line complications were the clinical signs of thrombosis, edema, leakage, phlebitis, occlusion, abrupt accidental catheter withdrawal, arrhythmia, pneumothorax, and pleural effusion. Sepsis-related data (if applicable): Laboratory data such as complete blood count, C-reactive protein, peripheral blood culture, catheter tip culture, and organisms isolated from cultures as study outcomes (11).
- The protocol for managing PICC troubleshooting was as follows
In cases of arrhythmia, leakage, pneumothorax, and pleural effusion, the catheters should be removed. If infection is suspected, cultures should be taken from blood periphery, directly from the catheters, and the PICC line tip. Antibiotic therapy should be started, and the PICC should be removed if necessary. If thrombosis is suspected, anticoagulation therapy should be considered, and the PICC should be removed three days after therapy is started if necessary. If occlusion is diagnosed, attempts should be made to clear the occlusion with gentle pressure and washing. The PICC should be removed if necessary. In cases of edema and phlebitis, the area should be warmed with a compress, and the catheter should be monitored. The PICC catheter should be removed if the symptoms are severe or persistent.
3.1. Statistical Analysis
Descriptive statistics, including parameters such as frequency, percentage, mean, and standard deviation, were used to report the results and evaluate quantitative variables in the study. To assess the correlation between two qualitative variables, the chi-square test and Fisher's exact test were utilized. The Analysis of Variance (ANOVA) test was employed to investigate the correlation between a quantitative variable and a qualitative variable. All statistical analyses were performed with a significance level of 0.05 using SPSS-26 software.
3.2. Ethics
Peripherally inserted central catheter line insertion was performed only when deemed necessary and based on the neonates' requirements and indications to ensure safe intravenous access for long-term use (5, 7). Detailed explanations regarding the procedure and its purpose were provided to the parents, and informed consent was obtained from them. Throughout the study, patient confidentiality was strictly maintained, and the principles outlined in the Helsinki Declaration were carefully followed. This study was approved by the ethics committee of Tehran University of Medical Sciences and received the code of ethics IR.TUMS.CHMC.REC.1401.001.
4. Results
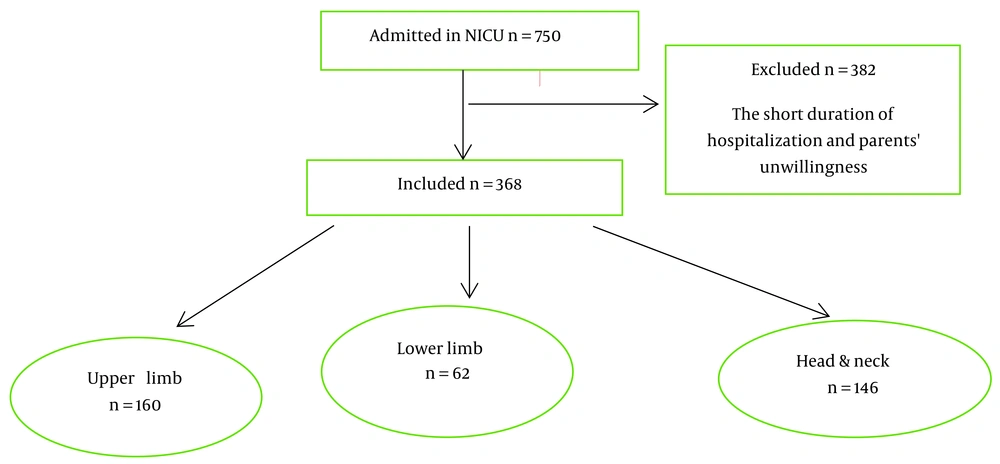
In this cross-sectional study, a total of 750 neonates were admitted to the NICU. However, 382 neonates were excluded from the study due to a short duration of hospitalization or parental unwillingness. Therefore, the final sample size for analysis included 368 neonates (Figure 1).
The mean gestational age of the studied neonates was 36.51 ± 3.26 weeks. The mean weight of the neonates was recorded as 2850.3784 ± 763.58 grams. In the majority of cases, the UEs were the preferred site for PICC line insertion, accounting for 43.5% of the cases, while the LEs were less commonly used, accounting for 16.8% of the cases. The three most frequent underlying diseases observed in the neonates were gastrointestinal, infectious, and neurological conditions. There was a significant difference in the mean gestational age among these three disease groups. The highest mean gestational age was observed in the UE group, while the lowest mean gestational age was observed in the H&N group and LE group (P-value = 0.008). However, there was no significant difference in terms of gender distribution among these three disease groups (P-value = 0.57). Table 1 presents the frequency of the anatomical site of PICC insertion and the type of veins used for catheter placement, as well as the positions and mean of pulling out the catheter to correct the PICC line.
| Variables | Frequency | Percent | Right Place | Peripherally | Malposition | Mean of Pulling out the Catheter (cm) |
|---|---|---|---|---|---|---|
| UE | ||||||
| Dorsal Hand | 53 | 33.1 | 21 (39.6) | 25 (47.2) | 7 (13.2) | 2 |
| Median | 9 | 5.6 | 3 (33.3) | 3 (33.3) | 3 (33.3) | 2 |
| Brachial | 52 | 32.5 | 25 (48.1) | 11 (21.2) | 16 (30.8) | 2.12 |
| Cephalic | 17 | 10.6 | 7 (41.2) | 5 (29.4) | 5 (29.4) | 2.8 |
| Axillary | 22 | 13.8 | 9 (40.9) | 6 (27.3) | 7 (31.8) | 1.7 |
| Basilic | 7 | 4.4 | 4 (57.1) | 1 (14.3) | 2 (28.6) | 1 |
| Total | 160 | 100.0 | 69 (43.1) | 51 (31.8) | 40 (25) | |
| LE | ||||||
| Saphenous | 58 | 93.5 | 47 (81) | 4 (6.9) | 7 (12.1) | 0.5 |
| Dorsal foot | 4 | 6.5 | 3 (75) | 1 (25) | 0 (0) | - |
| Total | 62 | 100.0 | 50 (80.6) | 5 (8.1) | 7 (11.3) | |
| H&N | ||||||
| Temporal | 117 | 80 | 58 (49.6) | 34 (29.1) | 25 (21.4) | 1.54 |
| Auricular | 13 | 9 | 6 (46.2) | 7 (53.8) | 0 (0) | - |
| Jugular | 16 | 11 | 8 (50) | 3 (18) | 5 (31) | 1.4 |
| Total | 146 | 100.0 | 72 (49.3) | 44 (30.1) | 30 (20.6) |
Abbreviations: UE, upper extremity; LE, lower extremity; H&N, head & neck.
a Values are presented as No. (%).
In pre-term neonates, the incidence of malposition was significantly higher compared to full-term neonates (P-value = 0.000). However, on average, the amount of catheter pullout required for correction was slightly less in pre-term neonates (1.7 cm) compared to full-term neonates (1.9 cm). It is worth noting that the minimum amount of catheter pullout required was 1 cm, which was consistent across both pre-term and full-term neonates (Table 2). The average weight of neonates included in the study was 2850 grams. Among neonates with catheter malposition, the mean average weight was 2805 grams, which was slightly lower than the overall average weight. There was a significant relationship observed between low weight and catheter malposition, with a P-value of 0.000. Table 3 provides a summary of the technical characteristics of the PICC lines based on their different insertion sites, including H&N, UE, and LE. These characteristics include the primary calculated length of catheter insertion, the accuracy of catheter position, the need to pull out the catheter, the mean amount of catheter pullout, and the number of days the PICC line has been used.
| Variables | Values |
|---|---|
| < 37 weeks | |
| Malposition | 24.4% |
| Mean of pulling out the catheter | 1.7024 |
| Minimum of pulling out the catheter | 1.00 |
| ≥ 37 weeks | |
| Malposition | 22.7% |
| Mean of pulling out the catheter | 1.9667 |
| Minimum of pulling out the catheter | 1.00 |
| Variables | Study Population 368 Neonates | UE | LE | H&N | P-Value |
|---|---|---|---|---|---|
| PICC insertion length | 15.63 +/- 4.9 | 15.74 +/- 4.14 | 20.26 +/- 4.56 | 12.71 +/- 2.39 | 0.001 |
| Accuracy of PICC position | 0.004 | ||||
| Right place | 191 (52) | 69 (43.1) | 50 (80.6) | 72 (49.3) | |
| Peripheral | 100 (27.1) | 51 (31.8) | 5 (8.1) | 44 (30.1) | |
| Malposition | 77 (20.9) | 40 (25.1) | 7 (11.3) | 30 (20.6) | |
| catheter pull out | 0.325 | ||||
| Yes | 87 (23.6) | 40 (25) | 7 (11.3) | 30 (20.5) | |
| No | 281 (76.4) | 120 (75) | 55 (88.7) | 116 (79.5) | |
| Amount of catheter pull-out (cm) | 1.83 ± 0.85 | 2.05 ± 0.93 | 0.5 ± 0.25 | 1.51 ± 0.71 | 0.03 |
| PICC duration of use | 16.18 ±11.88 | 14.08 ± 10.10 | 19.25 ± 14.38 | 17.7 ± 12.20 | 0.006 |
Abbreviations: UE, upper extremity; LE, lower extremity; H&N, head & neck; PICCs, peripherally inserted central catheters.
a Values are presented as No. (%).
There were 14 patients with positive blood cultures. Out of these 14 positive blood cultures, only 4 PICC line tip cultures had also been obtained, and only one of them was positive for Candida albicans, which matched the blood culture result (Table 4). The frequency of different microorganisms isolated from the blood cultures was assessed, and no statistically significant difference was found between different catheter sites and types of microorganisms. Additionally, in this study, it was observed that catheter location and malposition did not have a significant relationship with sepsis (P-value = 0.950, P-value = 0.627).
| Sepsis (Frequency) | Study Population (N = 368 Neonates) | UE (n = 160) | LE (n = 62) | H&N (n = 146) | P-Value |
|---|---|---|---|---|---|
| Culture positive sepsis | 14 (3.8) | 6 | 2 | 6 | 0.950 |
| P-value | 0.271 | 0.874 | 0.585 | ||
| Clinical sepsis | 44 (12) | 13 | 11 | 20 | 0.159 |
| P-value | 0.211 | 0.620 | 0.89 | ||
| Sepsis (Frequency) | Study Population (N = 368 Neonates) | UE, Malposition | LE, Malposition | H&N, Malposition | P-Value |
| Culture positive sepsis | 14 (3.8) | 2 | 0 | 0 | 0.627 |
| P-value | 0.854 | ||||
| Clinical sepsis | 44 (12) | 7 | 7 | 4 | 0.379 |
| P-value | 0.251 | 0.041 | 0.757 |
Abbreviations: UE, upper extremity; LE, lower extremity; H&N, head & neck.
a Values are presented as No. (%).
The frequency of other complications and the average duration of PICC maintenance (use) were compared among the three groups based on catheter insertion sites. The most frequent complications were catheter occlusion (22.7%), followed by accidental catheter withdrawal at 18.2%. The less common complications were related to thrombosis, arrhythmia, and pleural effusion. Overall, the prevalence of complications was higher in the LE group compared to the UE and H&N catheter groups (22.6%). However, there was no statistically significant difference in the incidence of these catheter-related complications among the three groups (P-value = 0.458).
The mean duration of PICC usage was the longest for LE catheters. The durability of the LE catheters was statistically higher than the other catheter sites (P-value = 0.042). The reason for catheter removal was reported in different catheter groups. However, the difference between the three groups was not statistically significant (P-value = 0.09). In all catheters, the most common reason for catheter removal was the patients' discharge from the hospital, while the least common cause of catheter removal in all three different insertion sites was infant death.
5. Discussion
In this cross-sectional study, 368 neonates admitted to the NICU who required a PICC line were included. The researchers calculated the appropriate length for catheter insertion and confirmed its placement. If necessary, adjustments to the catheter tip were made. The study also evaluated the accuracy of catheter length measurements, complications related to the catheter, and the duration of maintenance. Finally, the outcomes of catheter insertion in three different areas (UE, LE, and H&N) were compared.
The most common catheter placement in this study was in the UEs, with a percentage of 43.5%. The patients in this group had a higher mean gestational age and weight compared to those in other sites. These findings suggest that nurses prefer to choose the UEs for catheter insertion in most cases, but in difficult cases, alternative sites are selected. There are several reasons for this trend. Firstly, in the history of medicine, veins in the UEs have typically been the first choice for catheter placement. Additionally, there are more peripheral veins available in the UEs, such as the basilic, cephalic, and axillary veins. Furthermore, there may be a general stereotype or mindset that using veins in the LEs for PICC placement is associated with a higher risk of catheter-related complications. This preference for UE catheter placement is consistent with the findings of Santos-Costa et al. (12), where UE catheters were also utilized more frequently compared to other sites.
Among the PICC lines, the highest risk of malposition was observed among catheters placed in the UEs, with a malposition rate of 25% (P-value = 0.004). In cases where malposition occurred in the UEs, the catheter needed to be pulled out a minimum of 1 cm and a maximum of 2.8 cm to reach the appropriate placement. Out of the 40 UEs with malpositioned catheters, 13 cases (32.5%) had catheters located within the atrium or ventricle, which can potentially lead to cardiac arrhythmias due to cardiac stimulation by the PICC line (13, 14). Considering this risk, it is advisable to modify the formula used to calculate the length of the catheter inserted in the UEs. Instead of aligning the catheter with the third intercostal space (3), it would be more reasonable to align it with the second intercostal space, along the right sternal border.
In our study, we found a significantly higher incidence of PICC malposition in preterm or low-weight neonates compared to full-term or high-weight neonates (P-value = 0.000, P-value = 0.000). Therefore, it is even more crucial to adjust the formula for calculating the length of the catheter in preterm or low-weight neonates. Additionally, it is worth noting that in 20 cases (50%) of UE malposition, the catheters entered the jugular veins, which was also reported as the most common site of malposition in a study by Trerotola et al. (15). To reduce this malposition, Song et al. recommended a slow and careful insertion of the catheter, ensuring that it follows the blood flow to the vena cava and eventually to the heart (16). Zheng’s study suggests that one way to reduce the incidence of catheter tip malposition during UE PICC placement is to block the internal jugular vein (17). Additionally, narrowing the jugular angle by turning the head towards the intended shoulder has been suggested to reduce misplacement of the PICC during insertion (9, 16).
Zheng et al., in their meta-analysis study, mentioned that the position of the patient may affect the UE PICC placement. They found that the prevalence of misplaced catheters is higher in the UE than in the LE, so nurses should pay attention to this position when inserting the catheter (17).
Central line-associated bloodstream infection (CLABSI) was found in 14 cases. Although the rate was higher in the H&N area, this difference was not statistically significant (P-value = 0.950). Among the infectious etiologies, Klebsiella pneumoniae was the most common microorganism in our study, while in other studies, coagulase-negative Staphylococcus epidermidis was the most common microorganism (10, 18). Out of the 14 positive cultures, only 4 PICC line tip cultures were obtained, and one of them was positive for Candida albicans, which matched the positive blood culture result. A limitation of our study was the use of small PICC lines (1 or 2 French), which prevented us from taking blood cultures directly from the catheters. Therefore, it is possible that our positive blood cultures were a result of a nosocomial NICU infection and not directly linked to the catheters (19).
Regarding other catheter-related complications, catheter occlusion was the most common complication at 22.7%, followed by abrupt accidental catheter withdrawal at 18.2%. Less common complications included thrombosis, arrhythmia, and pleural effusion. The LE experienced more complications than the UE and H&N, with no statistically significant difference. Wu et al. conducted a 3-year review and found that LE issues could be attributed to the longer length of LE catheters, which caused more mechanical stimulation and its associated complications (20). In a meta-analysis by Chen et al., they compared the PICC complications between UE and LE. They mention that LE PICC increases the risk of thrombosis in cases of abdominal surgery (21, 22). We reported only one case of thrombosis in the lower extremity PICC site, which was not statistically significant compared to other PICC sites (P-value = 0.47). This may be because, according to our NICU's protocol, LE PICCs are not placed in cases of abdominal surgery.
In our study, the most common reason for catheter removal was the completion of treatment, accounting for 84% of cases, while complications accounted for only 16% of catheter removals. However, in Elmekkawi et al.'s study, complications accounted for 32% of catheter removals (10), and in Song and Li (16) and Bashir et al. (23) studies, complications were reported as the most common reason for catheter removal. These variations in catheter placement and nursing care of PICC line catheters across different centers using different protocols could explain the discrepancy in the frequency of complications observed.
The longest duration of PICC usage was observed with LE and H&N PICC catheters. Considering that the most common reason for catheter removal was the end of the treatment period, this suggests that babies with LE and H&N catheters had more complex conditions and required a longer treatment period. It also indicates that nurses prefer to use LE and H&N catheter insertion for challenging cases.
5.1. Limitations
A limitation of our study was the use of small PICC lines (1 or 2 French), which prevented us from taking blood cultures directly from the catheters. Therefore, it is possible that our positive blood cultures were a result of a nosocomial NICU infection and not directly linked to the catheters. Another limitation of our study is the small number of each group, and more studies with different gestational ages and weights will help to better study results.
5.2. Conclusions
The lengths of the catheters should be adjusted based on regional studies that take into account factors such as race, age, and weight of the patients, in addition to following general guidelines. This study suggests that the formula for calculating the length of the catheter in the upper extremities should be adjusted to align with the second intercostal space at the right sternal border, rather than the third intercostal space, for more precise catheter insertion.