1. Background
Enhanced recovery after surgery (ERAS) refers to the optimization of perioperative measures through multidisciplinary collaboration and evidence-based approaches to improve patient care during the perioperative period and promote early recovery for surgical patients. With the widespread application of ERAS principles in pediatric surgery, it has been found that ERAS can alleviate surgical stress responses in children, shorten recovery time and hospital stay, reduce postoperative complications, and increase parental satisfaction (1, 2). For example, a study implementing an ERAS protocol in pediatric colorectal surgery found that the average hospital stay was reduced from 8.3 to 5.7 days, and postoperative opioid use was significantly decreased (3). Currently, research on pediatric ERAS mainly focuses on exploring the application effects of the ERAS concept in various diseases (4). Globally, ERAS has been successfully applied in pediatric surgery with significant benefits. For instance, in a study on pediatric patients undergoing colostomy closure and Malone procedures, those under ERAS protocols had a shorter median length of hospital stay (3.0 days compared to 4.5 days) and reduced opioid use, although complication rates remained similar (5). Although guidelines and consensus on ERAS have been published, there are still many deficiencies in the service standards and management of pediatric ERAS (6, 7).
Quantitative data also underscore the benefits of ERAS in pediatric populations. For example, ERAS protocols in various pediatric surgeries have shown a reduction in hospital stay by an average of 2.1 days and a decrease in healthcare costs by 15% (8). In addition, there is a lack of relevant research on the specific implementation of ERAS in pediatric surgical institutions. This national survey is crucial at this time to systematically assess the current state of ERAS implementation in pediatric surgery across China, identify existing gaps, and provide data to inform the development, management, and formulation of relevant policies for pediatric ERAS. The survey results are now reported as follows.
2. Methods
2.1. Study Participants
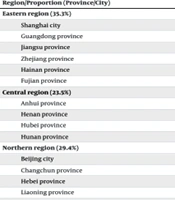
In April 2023, a total of 23 medical institutions from 17 provinces and cities in China were selected by the Alliance of Pediatric Surgery. This nursing alliance is led by the National Children's Medical Center, in collaboration with regional children's medical centers and large-scale tertiary pediatric specialty hospitals across various provinces and cities, including Shanghai, Zhejiang, Jiangsu, Guangdong, Beijing, Chongqing, Sichuan, Shaanxi, Hunan, Hubei, Anhui, Fujian, Henan, Hebei, Hainan, Jilin, and Liaoning. These institutions represent the current development status of pediatric surgery in China. All participating institutions have pediatric surgical departments, and all survey participants provided informed consent.
2.2. Survey Tools
The questionnaire for investigating the implementation status was developed by our research team based on a review of relevant literature and discussions among seven core members of the pediatric surgery group at the National Children's Medical Center. The questionnaire underwent a thorough development and validation process, including pre-testing and pilot testing to ensure clarity, logicality, and professionalism. The questionnaire's Cronbach's alpha value was 0.85, indicating high internal consistency. It consists of four parts as follows: (1) essential information: This section includes details about the hospitals, such as their location, level, and type; (2) surgical volume data: This section encompasses the total number of surgeries conducted in 2022, along with the number of grade III and IV surgeries; (3) nursing staff and bed capacity: This section provides comprehensive details about the nursing staff and bed capacity within hospitals, including the current count of employed general surgery nurses, the total number of beds in the hospital, the number of beds in surgical wards specifically, and the number of beds dedicated to general surgery (including neonatal surgery); (4) ERAS program implementation status: This section evaluates whether ERAS is currently implemented, the presence or absence of specialized ERAS nurses within departments that implement ERAS programs, the existence or non-existence of an ERAS team group, and previous execution of any conducted ERAS projects.
2.3. Data Collection and Quality Control
Researchers conducted an online questionnaire survey using the “Wenjuanxing” platform, wherein the questionnaire instructions explicitly stated the survey's purpose, completion methods, precautions, and confidentiality of results. Participants were able to complete the questionnaire using their mobile phones or computers. Researchers contacted nursing directors from various institutions and provided a detailed explanation of the survey's purpose, significance, and content. After obtaining informed consent, electronic questionnaires were distributed via WeChat. To enhance the accuracy of self-reported data, methods such as cross-verifying data with medical records were implemented, and follow-up interviews were conducted with a subset of respondents to validate responses. A total of 23 medical institutions within this alliance participated in the survey and provided valid responses. Following data collection, cross-checking was conducted on questionnaires with evident errors to ensure data accuracy.
2.4. Statistical Analysis
Data analysis was performed using SPSS version 26.0. Continuous variables that did not follow a normal distribution were summarized using the median and interquartile range (IQR). Categorical variables were expressed as frequencies and percentages. To assess differences between groups, appropriate statistical tests were employed. For continuous variables, the Mann-Whitney U test or Kruskal-Wallis test was used, depending on the number of groups compared. Categorical variables were analyzed using the chi-square test or Fisher's exact test where appropriate. Statistical significance was set at a P-value of < 0.05.
3. Results
3.1. Medical Institution
The distribution of the 23 medical institutions across 17 provinces/cities is presented in Table 1. Among these, there are 22 class A tertiary hospitals (95.7%), one class B tertiary hospital (4.3%), five comprehensive hospitals (21.7%), 15 pediatric specialty hospitals (65.2%), and three maternal and child health hospitals (13.0%).
| Region/Proportion (Province/City) | No. of Hospitals |
|---|---|
| Eastern region (35.3%) | |
| Shanghai city | 4 |
| Guangdong province | 2 |
| Jiangsu province | 2 |
| Zhejiang province | 2 |
| Hainan province | 1 |
| Fujian province | 1 |
| Central region (23.5%) | |
| Anhui province | 1 |
| Henan province | 1 |
| Hubei province | 1 |
| Hunan province | 1 |
| Northern region (29.4%) | |
| Beijing city | 1 |
| Changchun province | 1 |
| Hebei province | 1 |
| Liaoning province | 1 |
| Western region (11.8%) | |
| Sichuan province | 1 |
| Chongqing city | 1 |
| Shanxi province | 1 |
Distribution of Regions and Provinces/Cities Among 23 Medical Institutions (N = 23)
3.1.1. Surgery Volume, Number of Nurses, and Beds
The detailed results of the surgical volume, number of nursing staff, and bed capacity for the 23 participating hospitals in 2022 can be found in Table 2.
| Indicators | Range | Median |
|---|---|---|
| Total number of general surgeries | 886 - 45000 | 3338 (2356, 5171) |
| Total number of grade III surgeries | 300 - 3800 | 1350 (944, 2154) |
| Total number of grade IV surgeries | 80 - 1879 | 423 (220, 963) |
| Number of general surgical nurses | 12 - 86 | 33 (25, 50) |
| Total number of beds | 500 - 7000 | 1500 (970, 2200) |
| Number of beds in surgical wards | 44 - 843 | 252 (178, 600) |
| Number of general surgery beds | 45 - 209 | 80 (54, 132) |
Surgery Volume, Number of Nurses and Beds of 23 medical Institutions in 2022 (N = 23)
3.1.2. Implementation of ERAS
Of the 23 hospitals surveyed, 21 (91.3%) had implemented ERAS protocols. Among these 21 hospitals, ERAS teams/groups comprising doctors, nurses, nutritionists, rehabilitation therapists, and anesthesiologists were established in 15; specialized ERAS nurses were present in six (26.1%); and all 21 hospitals provided comprehensive ERAS training (Table 3). The departments with the highest adoption rates of ERAS were general surgery, urology, and orthopedics. The primary conditions targeted by ERAS included appendicitis, gallbladder cysts, and congenital megacolon. Key components frequently incorporated into the program encompassed early removal of postoperative tubes, effective management of postoperative pain, and prompt mobilization, whereas aspects such as optimization of discharge preparation readiness, anesthesia planning refinement, surgical approach selection, and postoperative catheter retention received comparatively less attention during implementation.
| Indicators | No. of Hospitals (%) |
|---|---|
| Preoperative fasting | 20 (95.2) |
| Preoperative rehabilitation health education | 20 (95.2) |
| Temperature management during surgery | 20 (95.2) |
| Optimizing anesthesia plan | 17 (81.0) |
| Fluid management during and after surgery | 20 (95.2) |
| Surgical procedure | 17 (81.0) |
| Postoperative catheter placement | 17 (81.0) |
| Early postoperative extubation | 21 (100.0) |
| Postoperative pain management | 21 (100.0) |
| Early postoperative feeding and hydration | 20 (95.2) |
| Early postoperative activity | 21 (100.0) |
| Discharge readiness | 15 (71.4) |
The Implementation of ERAS (N = 21)
3.2. Analysis by Hospital Type and Region
The statistical analysis by hospital type (Table 4) and region (Table 5) reveals significant variations in ERAS implementation. Pediatric hospitals had the highest mean number of total surgeries (5022.34 ± 1995.89), compared to general hospitals (3010.45 ± 1490.67) and maternity & child health hospitals (2005.12 ± 1005.56). The number of nurses was similar between general hospitals (35.23 ± 10.78) and pediatric hospitals (33.78 ± 15.45), while maternity & child health hospitals had fewer nurses (20.45 ± 10.56). The total number of beds was highest in pediatric hospitals (1623.45 ± 700.12), followed by general hospitals (1500.67 ± 500.89) and maternity & child health hospitals (1000.34 ± 400.78). These differences were statistically significant (p-values of 0.012 and 0.021, respectively).
| Variables | General Hospital | Pediatric Hospital | Maternity and Child Health Hospital | t | P |
|---|---|---|---|---|---|
| Total surgeries | 3010.45 ± 1490.67 | 5022.34 ± 1995.89 | 2005.12 ± 1005.56 | 2.56 | 0.012 |
| Nurses | 35.23 ± 10.78 | 33.78 ± 15.45 | 20.45 ± 10.56 | 1.78 | 0.085 |
| Total beds | 1500.67 ± 500.89 | 1623.45 ± 700.12 | 1000.34 ± 400.78 | 2.34 | 0.021 |
Statistical Results by Hospital Type
| Variables | Eastern Region | Central Region | Northern Region | Western Region | t | P |
|---|---|---|---|---|---|---|
| Total surgeries | 5012.34 ± 1990.89 | 3338.23 ± 1502.45 | 3000.78 ± 1301.34 | 4000.00 ± 1895.67 | 3.67 | 0.025 |
| Nurses | 33.78 ± 15.34 | 35.23 ± 10.89 | 28.67 ± 10.12 | 29.45 ± 10.23 | 2.45 | 0.049 |
| Total beds | 1500.67 ± 700.89 | 1742.34 ± 600.78 | 1000.34 ± 500.12 | 1400.00 ± 500.56 | 3.12 | 0.034 |
Statistical Results by Region
Regional analysis showed that the mean number of total surgeries was highest in the Eastern region (5012.34 ± 1990.89), followed by the Western (4000.00 ± 1895.67), Central (3338.23 ± 1502.45), and Northern regions (3000.78 ± 1301.34) (P-value of 0.025). The number of nurses was highest in the Central region (35.23 ± 10.89), followed by the Eastern (33.78 ± 15.34), Western (29.45 ± 10.23), and Northern regions (28.67 ± 10.12) (P-value of 0.049). The total number of beds was also highest in the Central region (1742.34 ± 600.78), followed by the Eastern (1500.67 ± 700.89), Western (1400.00 ± 500.56), and Northern regions (1000.34 ± 500.12) (P-value of 0.034).
3.3. Difficulties and Obstacles in Implementing the Enhanced Recovery After Surgery Project
In the multiple-choice question regarding the main difficulties and obstacles faced in implementing the ERAS program, the responses were as follows: Twelve individuals (52.2%) chose "Insufficient promotion and popularization of the concept of ERAS."; 13 individuals (56.5%) chose "The safety and effectiveness of ERAS need to be proven."; 20 individuals (87.0%) chose "Lack of specific clinical practice guidelines for various diseases under ERAS."; 14 individuals (60.9%) chose "Hospitals lack corresponding policy support."; 15 individuals (65.2%) chose "Medical staff lacks in-depth learning and understanding of the content of ERAS."; 12 individuals (52.2%) chose "Hospitals lack multidisciplinary collaboration teams composed of surgeons, anesthesiologists, and nurses."; 8 individuals (34.8%) chose "Patients and/or their families cannot effectively understand and cooperate with the implementation of fast-track surgery."; 17 individuals (73.9%) chose "Hospitals lack a unified quality control plan."
4. Discussion
Our study demonstrates that 91.3% of the surveyed hospitals have implemented ERAS protocols, which aligns with the national push for enhanced recovery practices. The significant advantages of ERAS in reducing hospital stays, enhancing patient recovery, and decreasing complications are well-documented internationally. For instance, studies found that ERAS protocols significantly reduce postoperative complications and improve recovery times in pediatric surgeries in Europe and North America (9-11). These benefits underscore the global relevance and effectiveness of ERAS in pediatric surgical care.
4.1. The Shortage of Enhanced Recovery After Surgery Specialized Nurses
The shortage of specialized ERAS nurses is a critical issue. The training and development of these nurses require substantial time and financial resources, posing a burden on many institutions (12). Additionally, unclear career progression paths and inadequate incentives deter nurses from pursuing specialization. To address this, increasing investment in training, establishing clear career pathways, and enhancing institutional support are essential. These measures can attract and retain specialized nursing staff, thereby improving ERAS implementation.
The shortage of ERAS specialized nurses can be attributed to several factors. Firstly, the training and development of specialized nurses require significant time and financial resources, which many medical institutions may struggle to bear. Training specialized nurses involves extensive clinical experience and formal education, which poses a substantial burden on both human and financial resources of medical institutions (13). Secondly, the career development pathways for specialized nurses are often unclear, leading to a lack of motivation among nurses to pursue further training. Without clear career progression and incentives, many nurses may be reluctant to invest additional time and effort into specialized training (14). Additionally, the lack of emphasis on specialized nursing in hospital management and policy contributes to the shortage (15). Many hospitals do not adequately recognize the importance of specialized nursing in their human resource strategies, resulting in insufficient support and incentives for specialized nurses.
To address these issues, potential solutions include increasing investment in the training of specialized nurses through joint funding by the government and hospitals to alleviate the financial burden. Establishing clear career development pathways and incentive mechanisms for specialized nurses can attract more nurses to participate in specialized training. Enhancing the recognition of specialized nursing in hospital management and policy, with more support and resource allocation, can also mitigate the shortage of specialized nurses.
4.2. Regional Variations in Enhanced Recovery After Surgery Implementation
This study demonstrates that the implementation of ERAS varies significantly across different regions. Hospitals in the Eastern region show higher adoption rates and more comprehensive ERAS protocols compared to those in the Central and Western regions. These differences can be attributed to several factors, including economic disparities, differing levels of policy support, and access to specialized healthcare professionals.
Eastern regions generally have better economic conditions, allowing for more investment in healthcare infrastructure and training programs. Additionally, some regions may have stronger policy support and incentives for ERAS implementation, influencing the rate and extent of adoption. Variations in access to specialized healthcare professionals and training programs can also impact the implementation of ERAS protocols.
4.3. Need for Specific Clinical Practice Guidelines
Despite the existence of national guidelines, there is a lack of specific clinical practice guidelines for various pediatric surgical conditions (2). This gap hinders the effective implementation of ERAS across different medical conditions. Developing targeted and specific guidelines for diverse pediatric surgeries is imperative for standardizing ERAS practices and improving outcomes.
4.4. Lack of Unified Quality Control Standards
The absence of a unified quality control plan in hospitals has impeded the development and promotion of ERAS. Currently, ERAS is still at the stage of implementing concepts and formulating processes, facing challenges such as lack of standards, non-standardization, and difficulties in achieving homogenization. The "Notice on Accelerating Rehabilitation Surgery Orthopedic Pilot Work" issued by the National Health Commission in 2020 proposed the establishment of a supervision and management mechanism along with a quality control evaluation system, indicating that further maturity is required for the application of ERAS (16).
It is imperative to integrate ERAS into standardized clinical pathways, introduce quality management systems, and establish comprehensive ERAS quality control standards for its continuous development. This approach also ensures efficiency and quality while achieving standardization, normalization, and homogenization in ERAS medical care.
The establishment of ERAS quality control standards can be based on a comprehensive and holistic concept of quality control within the framework of national medical quality management controls (17). Its content may include essential criteria (which should exceed more than half as recommended by consensus or guidelines), implementation qualities for each measure (such as developing preoperative education forms executed by medical staff who assess compliance rates among patients/parents), patient/parent compliance rates, etc., with the aim of gradually achieving uniformity, accessibility, effectiveness, and safety while maintaining deviations within an acceptable range through regulation of factors influencing the overall impact of nursing care on service delivery.
4.5. Enhancing Awareness Among Medical Staff
According to the ERAS concept, surgical treatment and nursing necessitate medical personnel to analyze patients' overall disease characteristics, as well as their treatment and care requirements. It is essential for medical staff to possess relevant knowledge of treatment and perioperative care to deliver optimal diagnostic and nursing services for patients (18). However, this study revealed that there is room for improvement in the level of awareness among medical personnel regarding ERAS, which aligns with previous findings from domestic research. Overall, there is a need for further enhancement of medical staff's knowledge on ERAS, highlighting the necessity for managers to strengthen standardized training programs aimed at reducing their lack of understanding and preventing passive implementation of pediatric ERAS measures (19).
The "Notice on Further Promoting Accelerated Rehabilitation Surgery" issued by the National Health Commission also emphasizes the importance of improving healthcare institutions' and medical personnel's comprehension of accelerated rehabilitation surgery concepts and models to facilitate a transformation in medical models and concepts. However, this study also revealed that out of the 23 surveyed hospitals, only 20 had implemented ERAS-related training programs (16). This finding suggests that existing ERAS training programs may encounter challenges in terms of content design, instructional methods, or evaluation efficacy.
When conducting ERAS training initiatives, it is imperative to develop evidence-based content aligned with guidelines and consensus while incorporating a diverse range of instructional formats. Moreover, establishing robust assessment criteria can significantly enhance medical staff's awareness and understanding of ERAS.
4.6. Policy Support for Enhanced Recovery After Surgery Implementation
During the implementation of ERAS, interdisciplinary collaboration is a prominent feature. This study also revealed that out of the 21 participating units, 15 had established dedicated ERAS teams or groups. The distinctiveness of this approach underscores the significance of policy support from hospital administrative departments for the successful implementation of ERAS protocols. It was found in this study that a lack of corresponding policy support impeded the development and dissemination of ERAS, which aligns with previous research conducted by Schwenk, who identified hospital administrative promotion as a pivotal driving force behind ERAS implementation (20). Therefore, it is imperative for hospital administrators to address this issue by developing and implementing supportive policies that facilitate the formation and functioning of ERAS teams, provide necessary resources, and ensure ongoing training and development opportunities for all involved staff. This can enhance the overall effectiveness and sustainability of ERAS programs.
4.7. Limitations
This study has several limitations that should be acknowledged. First, the cross-sectional design limits our ability to assess trends over time or establish causal relationships. This design captures a snapshot of the current implementation of ERAS protocols but does not provide insight into how these practices may change or develop over time. Second, there is a potential for selection bias as institutions were selected through convenience sampling, which may not represent the broader population of medical institutions in China. Third, the reliance on self-reported data from nursing directors introduces the risk of bias, as responses may be influenced by personal perceptions or recall inaccuracies. Finally, the study provides limited detail on the specific ERAS protocols being implemented at each institution, making it challenging to evaluate the consistency and effectiveness of these protocols across different settings.
4.8. Conclusions
The present study examined the current status of pediatric ERAS implementation in 23 medical institutions across 17 provinces and cities nationwide. It revealed that while ERAS enjoys relative popularity, its promotion remains uneven. Healthcare professionals possess limited understanding of ERAS, and there is a shortage of specialized nurses trained in ERAS protocols. Numerous obstacles still hinder the development of pediatric accelerated recovery surgery. Future research should focus on developing disease-specific clinical practice guidelines for ERAS and establishing standardized quality control measures. Hospital administrators ought to provide corresponding policy support based on departmental implementation of ERAS to foster its advancement.