1. Background
Bronchial asthma (BA) is a heterogeneous disease characterized primarily by chronic airway inflammation and airway hyperresponsiveness (AHR). Pathologically, inflammatory cells infiltrate the airway mucosa and release inflammatory mediators, leading to airway mucus hypersecretion and smooth muscle spasms (1). Clinically, BA typically manifests as recurrent chest tightness, wheezing, shortness of breath, and coughing, with symptoms often occurring or worsening at night or in the early morning (2). Statistics (3, 4) indicate that BA has a global incidence ranging from 0.3% to 17.0%. In China, BA is a common chronic respiratory disease in pediatric patients, with an incidence as high as 4.63% (5), which has been increasing year by year due to worsening air pollution. Data shows that approximately 300 million people worldwide suffer from BA, with one-third of them being children (6). The prevalence of asthma in urban children in China was 0.96% in 1990, 1.66% in 2000, and 2.38% in 2010 (7).
As a condition that is difficult to cure, BA hinders the healthy growth of pediatric patients due to recurrent symptoms and frequent relapses triggered by environmental stimuli, seriously affecting the physical and mental health of affected children. Given the significant impact of BA, researchers have shown a keen interest in the diagnosis and treatment of the disease. However, there is no universally accepted standard treatment for managing BA in pediatric patients. Ideally, treatment regimens for children with BA should aim to control symptoms and help patients resume normal activities, including learning.
Currently, step-up/down targeted therapy is the mainstay of BA treatment (7). The primary drugs used are bronchodilators and glucocorticoids, which aim to achieve and maintain effective symptom control, restore patients to their normal level of activity, maintain lung function, and prevent acute exacerbations and BA-related deaths. Evidence has shown that the onset and prognosis of BA are associated with the immune system and lung function, and the long-term use of glucocorticoids in BA treatment can impair immune function. Spleen aminopeptide (SA) is a clinically common immunomodulatory agent known for its immunosuppressive, immune function-enhancing, and anti-inflammatory properties. Previous studies have demonstrated that SA can effectively improve the overall treatment efficacy in children with BA and enhance their immune function. However, there have been no reports on the treatment of pediatric BA with the combination of SAs, budesonide (BUD), and salbutamol (8).
2. Objectives
The purpose of this research was to evaluate the clinical efficacy of a combined therapy consisting of SA, BUD, and levosalbutamol hydrochloride (LEV) in the treatment of pediatric BA and to assess its impact on immune function and inflammatory markers. The following sections provide a detailed report of the study.
3. Methods
3.1. General Information
This was a retrospective study. Sample Size Estimation: The study was divided into a combination group and a control group with a 1:1 ratio. The primary efficacy index, FEV1%pred, was calculated using the formula for estimating the mean sample size of two groups. The calculation was based on α = 0.05 and a power of 90%, considering the dropout rate. It was determined that the minimum sample size for each group was 35 cases. A total of 40 patients were collected for each group, resulting in 80 patients included in the study. The calculation formula used is as follows: n = 2 × (Zα + Zβ)² × σ²/δ².
Between June 2022 and June 2023, eighty children diagnosed with BA were selected from our medical facility and assigned to either the observation group or the control group according to the treatment method (n = 40 per group). The study received approval from the Institutional Ethics Committee of our hospital (No.: 2021-10; October 27, 2021), and prior to the research, written informed consent was obtained from the guardians of all participants.
Inclusion Criteria: (1) meeting the diagnostic criteria for BA (9); (2). aged 6 - 12 years; (3) good tolerance to the drugs used in this study and high treatment compliance; (4) informed consent provided and signed by the guardian. Exclusion Criteria: (1) concomitant severe liver or kidney dysfunction; (2) hypersensitivity; (3) interfering immune diseases or chronic inflammatory diseases; (4) recent use of oral immunosuppressants, steroids, or any other drugs that might affect the study results.
Treatment Protocol: Both groups received symptomatic treatment, including standard anti-infective therapy, oxygen therapy, spasmolysants, bronchodilators, and medication for fluid and electrolyte balance. In addition, the control group underwent inhalation therapy with nebulized BUD and LEV, three times a day for 15 minutes each session. The observation group received the same treatment as the control group, plus SA oral lyophilized powder (SAOLP) at a dosage of 2 mg daily, dissolved in 10 mL of cold water and taken orally once daily. Both groups were treated for 2 consecutive weeks, with dedicated guidance and supervision during medication application.
3.2. Efficacy Evaluation
Efficacy was evaluated for both groups on the last day of the 2-week treatment span using the following criteria: (1) complete response (CR), defined as the disappearance of all clinical symptoms, such as cough and wheezing, with noticeable improvement compared to the pre-treatment condition; (2) partial response (PR), defined as the disappearance of almost all clinical symptoms, fewer relapses during and after the treatment period, and some improvement compared to the pre-treatment condition; (3) no response (NR), defined as no remission of clinical symptoms, no improvement compared to the pre-treatment condition, or even worsening of symptoms after treatment.
The study defined the overall response rate (ORR) as the proportion of patients who achieved either a partial or complete response to the therapy. Additionally, the study evaluated and compared the length of hospital stay (LoHS) and the time taken for symptom improvement between the two groups.
3.3. Inflammatory Markers and Immunological Parameters
(1) inflammatory Markers, each patient provided a 5 mL fasting venous blood sample, which was centrifuged at a radius of 5 cm and 4000 rpm for ten minutes to collect and store the serum at -80°C. The levels of interleukin-2 (IL-2), interleukin-6 (IL-6), and interleukin-4 (IL-4) were measured using flow cytometry (9), while the levels of C-reactive protein (CRP) and tumor necrosis factor-alpha (TNF-α) were determined using turbidimetric immunoassay; (2) immunological parameters, fasting blood (3 mL) was collected from each patient, centrifuged at 4000 rpm with a centrifugal radius of 5 cm for 10 minutes, to harvest plasma from the upper layer. Flow cytometry was used to analyze the peripheral blood T cell subsets, specifically CD4⁺, CD3⁺, and the CD4⁺/CD8⁺ ratio. Additionally, immunoglobulin G (IgG) levels were measured using turbidimetric immunoassay, while immunoglobulin M (IgM) (10) and immunoglobulin A (IgA) levels were also assessed.
Two researchers independently assessed the risk of bias in the included studies and cross-checked the results.
3.4. Statistical Analysis
Data analysis was conducted using SPSS 22.0 software. Mean and standard deviation (±) were used to express measurement data, and differences between the two groups were analyzed using the t-test. Within-group pre- and post-treatment data were represented by means, and differences before and after treatment within each group were analyzed using the paired t-test. Counts and percentages were compared using the chi-square test. Differences were considered statistically significant when P < 0.05.
4. Results
The observation group, consisting of 22 boys and 18 girls aged between 6 - 12 years, with a mean age of (8.63 ± 1.84) years, was compared to the control group, which included 24 boys and 16 girls, with a mean age of (8.48 ± 2.08) years and an age range of 6 - 12 years. The two groups were deemed comparable based on their general characteristics, as no significant differences were detected (all P > 0.05). Please refer to Table 1 for more details.
| Variables | Observation (n = 40) | Control (n = 40) | t/χ² | P‐Value |
|---|---|---|---|---|
| Age (y) | 8.63 ± 1.84 | 8.48 ± 2.08 | 0.342 | 0.733 a |
| Sex (n) | 0.205 | 0.651 b | ||
| Male | 22 (55.00) | 24 (60.00) | ||
| Female | 18 (45.00) | 16 (40.00) | ||
| Disease course (day) | 3.13 ± 1.67 | 2.9 5 ± 1.58 | 0.481 | 0.632 a |
| Disease severity [n (%)] | 0.282 | 0.868 b | ||
| Mild | 11 (27.50) | 9 (22.50) | ||
| Moderate | 21 (52.50) | 22 (55.00) | ||
| Severe | 8 (20.00) | 9 (22.50) |
General Information
Following therapy, the observation group demonstrated an ORR of 95.00%, while the control group showed an ORR of 80.00%. A statistically significant difference was observed between the two groups (χ² = 4.114, P = 0.043), as shown in Table 2.
Length of Hospital Stay and Time to Symptom Improvement: Both LoHS and time to symptom improvement were significantly shorter in the observation group compared to the control group (all P < 0.05). See Table 3 for details.
| Groups | n | LoHS | Time to Complete Remission of Cough | Time to Complete Remission of Suffocative Asthma | Time to Complete Remission of Wheezing |
|---|---|---|---|---|---|
| Observation | 40 | 6.20 ± 1.56 | 3.78 ± 0.83 | 2.28 ± 0.45 | 4.13 ± 0.97 |
| Control | 40 | 7.33 ± 1.31 | 4.35 ± 1.00 | 2.58 ± 0.75 | 4.65 ± 1.10 |
| t‐value | 3.500 | 2.794 | 2.172 | 2.270 | |
| P‐value b | 0.001 | 0.007 | 0.033 | 0.026 |
Clinical Efficacy a
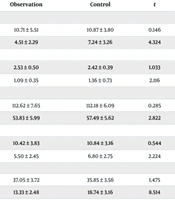
Initially, there were no significant differences in IL-8, IL-6, IL-2, IL-4, TNF-α levels, and CRP between the two groups before treatment (all P > 0.05). However, following treatment, both groups exhibited significant reductions in IL-6, IL-2, IL-8, IL-4, TNF-α levels, and CRP (all P < 0.05). The reduction was notably more pronounced in the observation group compared to the control group (all P < 0.05). For more information, please refer to Table 4.
| Outcome Measure (Time Point) | Observation | Control | t | P-Value b |
| IL‐2 (μg/L) | ||||
| Pre‐treatment | 10.71 ± 5.51 | 10.87 ± 3.80 | 0.146 | 0.884 |
| Post‐treatment | 4.51 ± 2.29 | 7.24 ± 3.26 | 4.324 | < 0.001 |
| IL‐4 (pg/mL) | ||||
| Pre‐treatment | 2.53 ± 0.50 | 2.42 ± 0.39 | 1.033 | 0.305 |
| Post‐treatment c | 1.09 ± 0.35 | 1.36 ± 0.73 | 2.116 | 0.038 |
| IL‐6 (ng/L) | ||||
| Pre‐treatment | 112.62 ± 7.65 | 112.18 ± 6.09 | 0.285 | 0.777 |
| Post‐treatment c | 53.83 ± 5.99 | 57.49 ± 5.62 | 2.822 | 0.006 |
| IL‐8 (ng/L) | ||||
| Pre‐treatment | 10.42 ± 3.83 | 10.84 ± 3.16 | 0.544 | 0.588 |
| Post‐treatment c | 5.50 ± 2.45 | 6.80 ± 2.75 | 2.224 | 0.029 |
| CRP (mg/L) | ||||
| Pre‐treatment | 37.05 ± 3.72 | 35.85 ± 3.56 | 1.475 | 0.144 |
| Post‐treatment c | 13.33 ± 2.48 | 18.74 ± 3.16 | 8.514 | < 0.001 |
| TNF‐α (ng/L) | ||||
| Pre‐treatment | 1.76 ± 0.18 | 1.73 ± 0.16 | 0.572 | 0.569 |
| Post‐treatment c | 1.10 ± 0.10 | 1.28 ± 0.07 | 9.051 | < 0.001 |
Pre‐ and Post‐Treatment Levels of Inflammatory Markers a
Similarly, there were no substantial differences in CD3⁺, CD4⁺, CD4⁺/CD8⁺, IgM, IgG, and IgA levels between the two groups before treatment (all P > 0.05). After treatment, both groups showed significant increases in CD3⁺, CD4⁺, CD4⁺/CD8⁺, IgM, IgG, and IgA levels compared to their pre-treatment levels (all P < 0.05). These increases were more pronounced in the observation group than in the control group (all P < 0.05). For more information, please refer to Table 5.
| Outcome Measure (Time Point) | Observation | Control | t | P-Value b |
|---|---|---|---|---|
| CD3⁺ (%) | ||||
| Before‐treatment | 42.64 ± 6.44 | 42.86 ± 6.19 | 0.154 | 0.878 |
| After‐treatment | 48.56 ± 6.36 | 43.30 ± 6.14 | 3.768 | < 0.001 |
| CD4⁺ (%) | ||||
| Before‐treatment | 27.31 ± 4.12 | 27.52 ± 3.83 | 0.239 | 0.812 |
| After‐treatment c | 38.27 ± 4.67 | 34.05 ± 4.83 | 3.971 | < 0.001 |
| CD4⁺/CD8⁺ (%) | ||||
| Before‐treatment | 1.28 ± 0.10 | 1.28 ± 0.07 | 0.206 | 0.837 |
| After‐treatment c | 1.76 ± 0.18 | 1.55 ± 0.16 | 5.276 | < 0.001 |
| IgM (g/L) | ||||
| Before‐treatment | 1.40 ± 0.65 | 1.39 ± 0.71 | 0.121 | 0.904 |
| After‐treatment c | 2.77 ± 0.64 | 2.42 ± 0.52 | 2.741 | 0.008 |
| IgG (g/L) | ||||
| Before‐treatment | 1.36 ± 0.27 | 1.33 ± 0.31 | 0.474 | 0.637 |
| After‐treatment c | 2.85 ± 0.76 | 2.32 ± 0.48 | 3.753 | < 0.001 |
| IgA (g/L) | ||||
| Before‐treatment | 1.35 ± 0.27 | 1.32 ± 0.31 | 0.464 | 0.644 |
| After‐treatment c | 2.83 ± 0.76 | 2.24 ± 0.42 | 4.254 | < 0.001 |
Pre‐ and Post‐Treatment Levels of Immunological Parameters a
Throughout the treatment period, adverse drug reactions (ADRs) were observed in both groups. In the observation group, there was one case of dizziness and two cases of nausea, resulting in an overall adverse reaction rate (OADRR) of 7.50%. In the control group, there were two cases of nausea and two cases of dizziness, leading to an OADRR of 10.00%. Notably, there was no significant difference in OADRR between the two groups (χ² = 0.157, P = 0.692).
5. Discussion
As a common chronic condition in childhood, BA is a heterogeneous disease primarily characterized by AHR and chronic inflammation, and it is associated with numerous factors (11). Reportedly, infection, allergen exposure, and vigorous exercise can trigger an acute onset of asthma (12). In China, the incidence of pediatric BA is on the rise, yet the overall management remains suboptimal. Generally, pediatric patients with BA are treated with anti-inflammatory agents, expectorants, and bronchodilators. Without effective management, symptoms can persist into adulthood, making BA a lifelong illness. Moreover, patients and their families bear significant physical, mental, and financial burdens due to long-term treatment and high drug doses (13). While inhalation therapy using nebulized medicines is a proven approach for ensuring efficacy and prompt symptom control, the choice of nebulized medicines should consider their adaptability and safety profiles (14).
This study demonstrated that, after treatment, the levels of T lymphocyte subsets (CD3⁺, CD4⁺, CD4⁺/CD8⁺) and immunoglobulins (IgM, IgG, IgA) were significantly higher in both groups of children compared to pre-treatment levels, with the observation group showing significantly higher levels than the control group (P < 0.05). The levels of inflammatory factors (IL-2, IL-4, IL-6, IL-8, CRP, and TNF-α) were significantly reduced compared to pre-treatment levels, and the reduction was more pronounced in the observation group than in the control group (P < 0.05). These findings are consistent with multiple other studies.
This suggests that SA s can effectively regulate the immune levels in children with BA, enhance their immune function, and inhibit inflammatory factors. The underlying mechanism is that SAs contain immune regulatory factors that act on regulatory T cells, promote helper T cell-mediated cellular immunity, inhibit helper T cell-mediated humoral immunity, regulate the Th1/Th2 balance, and modulate the release of inflammatory factors. This dual action helps in regulating immunity and suppressing inflammatory responses.
Spleen aminopeptide belongs to a complex of peptides and nucleotides and is considered a new type of immune enhancer (15). It contains various essential amino acids, trace elements, and immune regulatory factors vital for the human body. Spleen aminopeptides can promote lymphocyte activation, receptor regulation, and immune information transmission, improving immune suppression, enhancing the synergistic and proliferative effects of immune cells, increasing the activity of the monocyte-macrophage system, reducing local inflammatory reactions, and alleviating respiratory infections. Research has shown that SAs can improve the immune function of patients with BA (16, 17), activate and regulate T cell subsets, enhance the cytotoxic effects of T lymphocytes, stimulate cytokine secretion by immune cells, reduce IgE-mediated type I hypersensitivity reactions, and alleviate AHR. Furthermore, SAs promote immune information transmission, lymphocyte activation, and receptor regulation, enhance immune cell proliferation and synergistic effects, improve immune suppression caused by adrenal corticosteroids, boost monocyte-macrophage system activity, reduce respiratory infections and local inflammatory responses, and strengthen the overall immune function of somatic cells.
The results of this study showed that the total effective rate of treatment in the observation group was significantly higher than that in the control group after treatment (P < 0.05). However, there was no significant difference in the total incidence of ADRs between the two groups of children (χ² = 0.157, P = 0.692). These findings suggest that the combination of SAs with BUD and salbutamol can significantly reduce the inflammatory response in children, improve immune function, and provide good clinical efficacy with a high safety profile in the treatment of pediatric BA.
Budesonide, a non-halogenated adrenal glucocorticoid, can inhibit the production and release of inflammatory cytokines (18), combat allergies and infections, improve capillary permeability, inhibit and reduce IgE activity (19, 20), rapidly alleviate asthma symptoms in children, and improve lung function. Salbutamol, a β2 receptor agonist (21), can relax bronchial smooth muscle, enhance mucosal ciliary movement, and promote the discharge of airway secretions. Research has shown that salbutamol can inhibit the release of inflammatory factors (22, 23), reduce airway inflammation, exert anti-inflammatory effects, and improve clinical symptoms in children with BA.
5.1. Limitations
However, this study has some limitations, such as a small sample size and a short follow-up period. To further evaluate the clinical efficacy of this treatment, future studies should expand the sample size and extend the follow-up period. Currently, there is relatively little research on the treatment of BA using the combination of SAs, BUD, and salbutamol hydrochloride in clinical practice. There are no reports on major adverse reactions or the combined use of these three treatments, highlighting the need for further research in the future.
5.2. Conclusions
This study demonstrates that the combination of SAs, BUD, and LEV can significantly improve the immune function of children with BA, reduce the levels of inflammatory factors, and achieve excellent clinical outcomes. The combined therapy is more effective than the use of a single drug and does not increase the incidence of ADRs.