1. Context
Anaphylactoid purpura, a skin condition commonly seen in children with allergic diseases, often presents with extensive inflammatory reactions in capillaries and arterioles, lymphocyte infiltration, non-thrombocytopenic purpura, skin purpura, fever, and other symptoms (1-3). The condition frequently extends to other organs, particularly the kidneys, leading to a form of renal involvement known as "anaphylactoid renal purpura" or IgA vasculitis nephritis (IgAVN) (4-6). IgA vasculitis nephritis predominantly affects preschool-aged children, with boys at a higher risk than girls (7-9). Although the disease is self-limiting, it has a tendency to recur, leading to progressive renal function impairment characterized by proteinuria, hematuria, and potentially chronic kidney disease (CKD), which poses a significant threat to the life and health of affected children (10-12).
Given the potential for severe outcomes, current clinical guidelines emphasize aggressive treatment of IgAVN to slow renal function deterioration and prevent chronic renal failure. However, the pathogenesis of IgAVN in children remains inadequately understood, highlighting a critical gap in the existing literature. Recent advancements in our understanding of immunological and inflammatory processes in IgAVN underscore the need for a comprehensive review of the disease's pathogenesis. This review aims to address this gap by discussing key biological markers implicated in the onset of IgAVN, such as galactose-deficient IgA1, complement components, and inflammatory cytokines, and by outlining the current clinical management strategies.
2. Evidence Acquisition
2.1. Child IgA Vasculitis Nephritis Pathogenesis
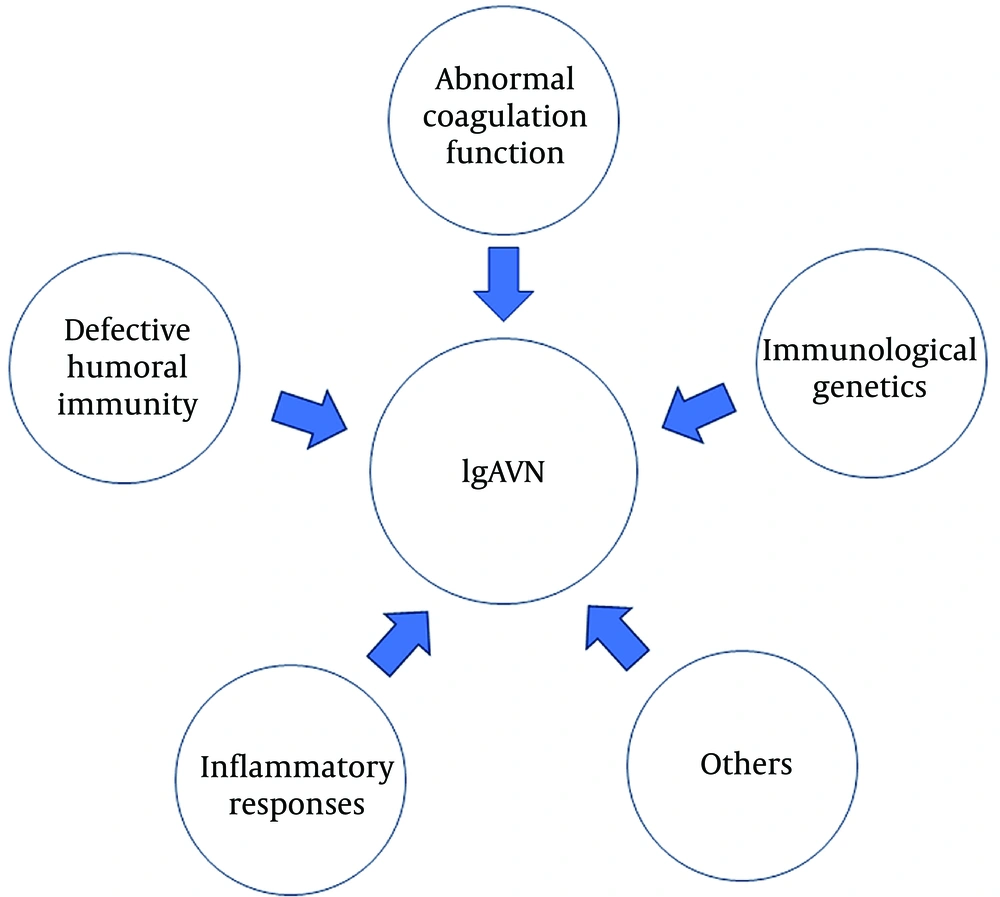
The exact cause of pediatric IgAVN remains unknown. However, several clinical studies support the hypothesis that defective humoral immunity, inflammatory responses, abnormal coagulation function, immunological genetics, and other factors contribute to its development (Figure 1).
2.2. The Relationship of Abnormal Humoral Immunity and Pediatric IgA Vasculitis Nephritis
2.2.1. Effects of Immunoglobulin A on the Pathophysiology of Pediatric IgA Vasculitis Nephritis
Pathological alterations in the kidneys of children with IgAVN closely resemble those found in IgA nephropathy, often classified histologically as immunoglobulin A nephropathy (13). Immunoglobulin A is a globulin with antibody function, consisting of two identical light chains and two identical heavy chains linked by disulfide bonds, which form a tetrapeptide chain structure. As an immunoreactive molecule, immunoglobulin A can bind with antigens to exert cellular immune effects, activate humoral immune responses, and regulate immune responses both positively and negatively.
Immunoglobulin A is synthesized and secreted primarily by secretory epithelial cells, and its expression is linked to abnormal humoral immunity. It is classified into two types: (1) immunoglobulin A1 (IgA1) and (2) immunoglobulin A2 (IgA2). Immunoglobulin A1 accounts for approximately 90% of total immunoglobulin A, while IgA2 constitutes about 10%. Immunoglobulin A contains two light chains and two heavy chains. The Fc region of IgA binds to Fc receptors on cell surfaces, while the Fab region binds to antigens.
Unlike IgA2, the two heavy chains in IgA1 are connected by a special hinge region composed of three amino acids, which can attach to O-chain glycans containing N-acetylgalactosamine. In galactose-deficient IgA1, the residues of N-acetylgalactosamine become exposed, allowing them to be recognized by autoantibodies targeting N-acetylgalactosamine. This immune response forms immune complexes that subsequently deposit in the glomerular mesangial area, leading to kidney damage characteristic of IgAVN (14).
The transferrin receptor and soluble Fc receptor can both bind to IgA1. The transferrin receptor is a transmembrane glycoprotein that binds to the transferrin-iron complex and plays a crucial role in facilitating the interaction between galactose-deficient IgA1 and mesangial cells. This receptor is vital in intracellular iron ion transport. When galactose-deficient IgA1 binds to mesangial cells, it promotes the deposition of immune complexes in the mesangial region of the glomerulus. Over time, this feedback loop can result in prolonged immune complex deposition, leading to damage and impaired renal function in patients with IgAVN.
The soluble Fc receptors, which are also transmembrane receptors, are primarily located in medullary cells. These receptors effectively bind to IgA1, enabling the recognition and binding of autoantibodies against galactose-deficient IgA1. The accumulation of macromolecular immune complexes, which are not metabolized by the liver, exacerbates renal impairment in children with IgAVN as these complexes accumulate in the mesangial region of the glomerulus (15).
Berthelot et al. compared patients with IgAVN to those with anaphylactoid purpura who did not have kidney damage (9, 16). They found that the concentrations of galactose-deficient immunoglobulin A1, IL-1, IL-6, interleukin-8 (IL-8), and interleukin-10 (IL-10) in the blood and urine of patients with IgAVN were higher than those of patients with anaphylactoid purpura without nephritis. This suggests that testing for immunoglobulin A expression in urine may serve as a prognostic marker, as IgAVN patients with elevated immunoglobulin A may have a worse prognosis.
Li et al. conducted a comparative study on kidney samples from patients with IgAVN and immunoglobulin A nephropathy, finding that patients with immunoglobulin A nephropathy exhibited glomerular mesangial hyperplasia (17). In contrast, patients with IgAVN displayed sclerotic glomeruli and more apparent signs of nephropathy, indicating significant pathological differences between immunoglobulin A nephropathy and IgAVN. These findings highlight the distinct pathological manifestations between the two conditions.
2.2.2. In Children, Advisement Deficiency Causes IgA Vasculitis Nephritis
Defects in C3 and C4 complement components are commonly observed in children with IgAVN. The immune complexes and immunoglobulin A in their bodies activate complement via the alternative pathway, leading to immune-mediated pathological damage (18).
2.2.3. IgA Vasculitis Nephritis in Children: T-Cell Malfunction and Disease Progression
T-cell subset dysfunction plays a crucial role in the etiology of IgAVN in children. CD4 and CD8 are common markers of T-cell subsets, which regulate immune functions by inducing and restricting each other. Under normal conditions, the CD4/CD8 ratio remains stable, maintaining a dynamic balance of immune responses. However, in children with IgAVN, immune dysfunction leads to disruptions in this balance, impairing the regulation of immune functions. T-cells are also vital for the development and specialization of B-cells, further contributing to the progression of the disease (19, 20).
2.3. Inflammatory Reactions
2.3.1. Renal Interstitial Inflammatory Cell Infiltration
IgA vasculitis is characterized by leukocyte infiltration within vascular walls, along with IgA deposits, making leukocyte infiltration a key feature in the pathogenesis of IgAVN (21). In children with IgAVN, monocytes and macrophages infiltrate the glomerulus and interstitium, and in severe cases, even polynuclear cells may infiltrate the tissue. Macrophages that enter the glomerulus form crescents, and the infiltrating cells release inflammatory mediators that induce inflammatory responses within the glomeruli and interstitium. Clinical pathology often reveals swollen endothelial cells with inflammatory cells infiltrating the perivascular space. In moderate to severe cases, electron microscopy shows extensive infiltration of leukocytes in the tissue (22). This suggests that leukocyte infiltration plays a significant role in the pathological progression of IgAVN. The molecular mechanism behind this augmented infiltration may be linked to the increased expression of vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) by interstitial cells, which facilitates the transmigration of leukocytes across the vascular endothelium to sites of inflammation (23).
2.3.2. Inflammatory Cytokines
Inflammatory cells and intrinsic kidney cells release various inflammatory cytokines that cause damage to kidney tissue, playing a significant role in the pathophysiology of IgAVN. Although the full mechanism of IgAVN is not entirely understood, it is believed that these cytokines contribute to disease progression. Yuan et al. (24) analyzed blood samples from individuals diagnosed with IgAVN and found significantly higher levels of TNF (tumor necrosis factor), IL-8, and IL-10 in these patients compared to a healthy control group. These patients also exhibited higher levels of urine protein, serum IL-8, and IL-10. Additionally, TNF levels in the serum were significantly elevated (P < 0.05). The study further revealed that the serum levels of TNF, IL-8, and IL-10 were higher in the acute nephritis group than in the chronic nephritis group and the nephrotic syndrome group. Correlation analysis demonstrated that IL-8 and IL-10 levels were positively correlated with the amount of urine protein in patients. Therefore, this study suggests that serum TNF, IL-8, and IL-10 are closely associated with the onset and progression of IgAVN, and measuring these cytokines could be used as an auxiliary indicator to assess the severity of IgAVN. Through retrospective analysis, Kataoka et al. (25) showed that increased production of C-reactive protein (CRP) and IL-5 (interleukin-5) occurred before the onset of purpura, indicating that these markers may serve as early warning signs of the condition’s development. Similarly, Ou et al. (26) conducted a meta-analysis exploring the association between purpura and IL-10. Their findings revealed that polymorphisms in IL-10 were closely linked to the risk of developing purpura in affected patients.
2.4. Abnormal Coagulation Function
Following the onset of IgAVN, patients' blood profiles often show abnormalities, suggesting that abnormal coagulation function may play a significant role in the development of the disease (27). Dang et al. found that blood tests in IgAVN patients indicated a hypercoagulable state (28). While there is no conclusive evidence directly linking thrombosis to the etiology of IgAVN, dysregulated coagulation mechanisms and thrombotic events are frequently observed in these patients. Abend et al. suggested that individuals with IgAVN who exhibit elevated levels of antiphospholipid antibodies are prone to a prothrombotic state and face an increased risk of cerebral venous sinus thrombosis. In addition, antiphospholipid antibodies are associated with various forms of renal injury, including renal large vessel thrombosis and renal artery stenosis, which can worsen the progression of IgAVN (29). Case reports indicate that elevated levels of coagulation factor VIII and homocysteine in patients with IgAV are linked to an increased risk of thrombosis (30-32). High homocysteine levels have been shown to correlate significantly with the risk of developing CKD (33). Elevated plasma levels of coagulation factor VIII are associated with more severe renal impairment in IgAVN patients and are also linked to poor survival outcomes (34). The evidence suggests that patients with IgAV may face an elevated risk of thrombosis due to dysregulated levels of antiphospholipid antibodies, homocysteine, and factor VIII. These abnormalities contribute to renal thrombosis, renal dysfunction, and reduced survival, indicating that a disturbed coagulation profile may be an important factor in precipitating the onset of IgAVN in affected individuals.
2.5. Immune Genetics
Though IgAVN is not classified as a hereditary illness, there is a notable genetic predisposition associated with the condition. In patients with IgAVN, the deposition of immune complexes in the mesangial region of the kidneys contributes to renal dysfunction. A significant factor contributing to this immune complex deposition is the frequent presence of a C4 gene deletion in patients with IgAVN. This deletion results in a severe deficiency of C4 throughout the body, which impairs the immune response and exacerbates the pathological damage to the kidneys (35-39).
3. Results
3.1. IgA Vasculitis Nephritis in Children: Biological Markers of Disease Progression
3.1.1. C-reactive Protein
C-reactive protein is an acute-phase reactant protein commonly used as a biomarker for inflammation. C-reactive protein can sensitively reflect the degree of inflammatory reactions in the body, and its expression is significantly elevated during inflammation. In a study by Ozdemir et al. (40), 112 children with anaphylactoid purpura were followed and compared to 81 healthy children. The results indicated that CRP levels were significantly higher in patients diagnosed with anaphylactoid purpura. Furthermore, a logistic regression analysis suggested that elevated CRP levels could predict the involvement of visceral organs in hypersensitivity purpura, indicating a potential prognostic use for CRP in disease monitoring.
Additionally, a study by Teng et al. (41) revealed that CRP levels in children with abdominal anaphylactoid purpura were significantly higher, suggesting that CRP has valuable diagnostic utility in cases of anaphylactoid purpura with abdominal involvement. These findings underscore the importance of monitoring CRP levels as a marker of disease progression and as a tool for predicting complications in children with IgAVN.
3.2. Pentraxin-3
Pentraxin-3 (PTX3) is a member of the pentraxin superfamily of proteins. Unlike CRP, which is primarily synthesized in the liver, PTX3 is produced by various cell types in peripheral tissues, including vascular endothelial cells, macrophages, myeloid cells, dendritic cells, fibroblasts, smooth muscle cells, and endothelial cells, in response to pro-inflammatory cytokines. Pentraxin-3 serves as an independent biological marker for inflammatory and infectious diseases due to its production outside the liver.
Clinical studies have explored the role of PTX3 in various diseases. For instance, Zhou et al. (42) investigated the feasibility of using PTX3 in sepsis diagnosis and concluded that PTX3 could assist in diagnosing the condition. Similarly, Erdenen et al. (43) found that PTX3 levels were significantly higher in patients with diabetic retinopathy, suggesting that PTX3 could serve as a predictor for the progression of the disease. Tunç et al. (44) studied neonatal bacterial septicemia and found that both CRP and PTX3 levels were significantly elevated in patients with clinical sepsis and septicemia compared to a control group, indicating that PTX3 could aid in diagnosing neonatal bacterial septicemia.
In the context of IgAVN, Ge et al. (45) proposed that PTX3 is implicated in the pathogenesis of IgAVN and may serve as a potential early biomarker for predicting the development of this condition. These findings highlight the utility of PTX3 as a diagnostic and prognostic tool in various inflammatory diseases, including IgAVN.
3.3. Interleukin
Interleukins are a group of cytokines crucial for immune regulation and are widely used in clinical research. Interleukin-2 (IL-2) is primarily produced by Th1 cells and plays a role in enhancing natural killer cell function, activating B-cells, and stimulating the secretion of immunoglobulin G (IgG) and immunoglobulin M (IgM). In patients with IgAVN, serum levels of IL-2 receptor are often abnormally elevated, and this receptor can bind to IL-2 on the cell membrane, further contributing to immune activation. Th2 cells are responsible for producing interleukin-4 (IL-4) and interleukin-10 (IL-10). Interleukin-4 promotes the transformation of IgG into immunoglobulin E (IgE), induces the development of eosinophils and mast cells, and stimulates B-cells. Interleukin-4 also triggers B cells to produce IgE after antigen stimulation, leading to its deposition in the mesangial area of the kidney, which contributes to renal function damage and plays a key role in the pathophysiology of IgAVN. Interleukin-10, an immunosuppressive molecule, can increase B cell viability and stimulate B cell growth, further contributing to disease progression.
Interleukin-6 (IL-6) is an inflammatory cytokine released by various cell types, including monocytes, macrophages, B-cells, T-cells, vascular endothelial cells, and fibroblasts. Interleukin-6 promotes the production of immunoglobulin A (IgA) and IgE, which can deposit in the mesangial area of the kidney, causing kidney damage and inflammation.
Interleukin-8 is a chemokine secreted by mononuclear macrophages that acts primarily on neutrophils. It stimulates the release of calcium ions in neutrophils, increasing their concentration and inducing chemotaxis of neutrophils and lymphocytes, thereby mediating the inflammatory response.
Interleukin-22 (IL-22) is mainly secreted by T lymphocytes and natural killer cells. Its receptor proteins are widely distributed in organs such as the liver, lung, and kidney, indicating its participation in inflammatory processes.
Berthelot et al. proposed that cytokines, including IL-1β, IL-6, IL-8, and IL-10, are correlated with the risk of nephritis in patients with IgAV. These cytokines may serve as predictive biomarkers for the development of nephritis in IgAV patients, aiding in early diagnosis and treatment (9).
3.4. Tumor Necrosis Factor
Tumor necrosis factor-α (TNF-α) is a systemic inflammatory cytokine primarily produced by macrophages. Tumor necrosis factor-α plays a crucial role in immune regulation by acting on lymphocytes and granulocytes, stimulating vascular endothelial cells to secrete more leukocyte adhesion molecules, and promoting the release of numerous inflammatory mediators, thereby inducing an inflammatory response (46). Wu et al. indicated that serum TNF-α levels correlate with both renal function and the pathological classification in patients with IgAVN, suggesting that TNF-α may serve as a potential biomarker for assessing the severity of the disease (47).
3.5. Pediatric IgA Vasculitis Nephritis: Treatment
3.5.1. Glucocorticoids
The treatment of IgAVN is generally symptomatic due to the limited understanding of its underlying causes. Glucocorticoids, commonly used in IgAVN treatment, provide local anti-inflammatory effects to control kidney inflammation and regulate immune function, thereby managing the disease to some extent in children. However, the clinical effectiveness of glucocorticoids in pediatric IgAVN remains controversial. Some researchers argue that while glucocorticoids can control kidney inflammation, they do not alter renal lesions or prevent the recurrence of purpura (48).
Despite the lack of robust evidence supporting glucocorticoid efficacy in IgAVN, the European initiative Single Hub and Access point for Pediatric Rheumatology in Europe (SHARE) recommends oral prednisolone as the first-line treatment for mild IgAVN. For moderate IgAVN, oral prednisolone and/or pulsed methylprednisolone are advised as first-line treatments. In severe cases, intravenous cyclophosphamide (CYC) combined with pulsed methylprednisolone and/or oral prednisolone is recommended (49).
3.5.2. Immunosuppressants
Immunosuppressants are often used in combination with glucocorticoids in the treatment of IgAVN, particularly in cases where patients do not respond well to glucocorticoid treatment or are resistant to it (50). Cyclosporin A is a commonly used immunosuppressant in IgAVN treatment (51, 52). Cyclosporin A works by inhibiting cytoplasmic calcium phosphatase, preventing its movement to the nucleus and blocking the transcription of IL-2, which is necessary for T-cell proliferation and differentiation. Without the support of T-cells, B-cell antibody production decreases, indirectly inhibiting humoral immunity and improving the abnormal immune responses observed in IgAVN patients (53).
also recommends that immunosuppressants such as azathioprine (AZA), mycophenolate mofetil (MMF), and/or pulsed methylprednisolone may be utilized as second-line treatments for patients with IgAVN following a renal biopsy or for those with moderate IgAVN. Cyclophosphamide in combination with pulsed methylprednisolone and/or oral prednisolone is recommended as a first-line treatment for patients with severe IgAV nephritis (49). However, these recommendations are based on expert consensus, and there is an urgent need for well-designed randomized controlled trials (RCTs) to evaluate the efficacy and safety of these treatments.
3.5.3. Anticoagulant Drugs
Hypercoagulability is a common complication in patients with IgAVN, closely linked to impaired coagulation function. As a result, anticoagulant drugs are considered for treating IgAVN (54). However, definitive evidence supporting the efficacy of anticoagulants in IgA nephropathy (IgAN) has yet to be identified (55).
One commonly used anticoagulant in clinical settings is low-molecular-weight heparin, which acts on coagulation factor IIa and coagulation factor Xa to inhibit platelet activation and aggregation. This action helps reduce blood flow resistance in vessels and alleviates the hypercoagulable state of the blood. Additionally, because low-molecular-weight heparin is produced through the chemical decomposition and enzymatic catalysis of regular heparin, it can also inhibit the activity of antiphospholipid antibodies. By blocking the activation of these antibodies, low-molecular-weight heparin helps reduce the risk of thrombosis (56).
3.5.4. Gamma Globulin
Gamma globulin is an exogenous immunoglobulin drug that is rich in immune antibodies. When administered to children with IgAVN, it helps replenish immune antibodies, thereby promoting the recovery of the body’s immune protection. Gamma globulin works by neutralizing antigens, enhancing the activity of natural killer cells, and effectively controlling inflammatory reactions (57). A clinically controlled trial demonstrated that the concurrent administration of dexamethasone and immunoglobulin, alongside prednisone, can boost the immune capabilities of pediatric IgAVN patients and support the restoration of renal function. While the study did not conclusively attribute the therapeutic benefits to immunoglobulin alone, it suggested a possible synergistic effect when combined with other treatments (58).
3.5.5. Traditional Chinese Medicine
Traditional Chinese medicine (TCM) is often regarded as having the advantages of mild drug properties and minimal side effects. There has been a growing body of clinical research investigating the use of TCM in treating IgAVN (59-64). A commonly used TCM treatment for IgAVN is tripterygium polyglycolide tablets, derived from Tripterygium wilfordii, a plant of the Celastraceae family. These tablets have anti-inflammatory and immune regulatory properties, helping to dredge channels, activate collaterals, improve blood circulation, and eliminate blood stasis (65).
Limited evidence also suggests that the Chinese patent medicine Sophora flavescens, when combined with conventional treatments, may be effective for treating IgAVN in children, with fewer side effects (63). Danshen-based formulations have also been reported to provide protective effects against renal disease in pediatric IgAVN patients, with minimal adverse effects (66). However, the existing evidence supporting the use of TCM in IgAVN is of low quality. More rigorous research is needed to establish the efficacy and safety of TCM in the prevention and management of IgAVN.
4. Conclusions
The pathophysiology of IgAVN in children remains incompletely understood, presenting a significant challenge for both clinical management and research. While current evidence suggests that abnormalities in humoral immunity, inflammatory responses, defective coagulation, and genetic predispositions contribute to the disease's development, these mechanisms are not fully delineated. Biomarkers such as CRP, interleukins, and PTX3 have been identified as potentially valuable in understanding disease progression and informing treatment strategies. However, the precise roles of these biomarkers and the pathways through which they influence IgAVN require further elucidation.
The current treatment approach for IgAVN primarily focuses on symptomatic care, utilizing glucocorticoids, immunosuppressants, anticoagulants, and gamma globulin. Although TCM has also been employed, there is limited high-quality evidence supporting its efficacy. The reliance on symptomatic treatment underscores the need for a deeper understanding of the disease’s underlying mechanisms to develop targeted therapies. Furthermore, recognizing and monitoring the identified biomarkers could potentially enhance early diagnosis and enable personalized treatment strategies, thus improving patient outcomes.
Despite advances in identifying potential biomarkers and understanding disease mechanisms, significant knowledge gaps persist. Current research is limited by the lack of large-scale, multicenter studies, and RCTs that could provide robust evidence for the efficacy of various treatments. Additionally, the genetic factors contributing to IgAVN are not well-characterized, and the interaction between genetic predispositions and environmental triggers remains speculative. The heterogeneity in clinical presentations and outcomes also complicates the establishment of standardized treatment protocols.
When compared with other pediatric renal conditions such as IgAN and Henoch-Schönlein purpura nephritis (HSPN), IgAVN shares several pathogenic features, including the involvement of abnormal IgA1 molecules and inflammatory responses. However, IgAVN often presents with a more acute onset and carries a higher risk of rapid progression to CKD than IgAN (67). The pathogenesis of IgAVN may involve a range of factors, including post-infectious triggers, such as group A β-hemolytic streptococcal infections, which have been implicated in related conditions like Henoch-Schönlein purpura and post-streptococcal glomerulonephritis (68).
Future research should prioritize large-scale, multicenter RCTs to evaluate the efficacy and safety of current treatment modalities, including the use of immunosuppressants and TCM in managing IgAVN. Longitudinal studies are also needed to explore the natural history of IgAVN, with an emphasis on identifying early predictive biomarkers for disease progression. Genetic studies should aim to elucidate the hereditary factors involved in IgAVN, which could lead to the development of genetic screening tools for at-risk populations.
Furthermore, research comparing IgAVN with other pediatric renal conditions, such as IgAN and HSPN, could provide valuable insights into shared and distinct pathogenic pathways, aiding in the development of more effective, condition-specific treatments.
When contextualized with other pediatric renal conditions, such as IgAN and HSPN, IgAVN shares several pathogenic features, including the involvement of abnormal IgA1 molecules and inflammatory responses. However, IgAVN often presents with a more acute onset and carries a higher risk of rapid progression to CKD compared to IgAN. This comparison underscores the need for tailored treatment approaches that address the unique aspects of IgAVN, while also leveraging insights from related conditions to improve clinical outcomes.