1. Background
Earthquakes are catastrophic natural events that affect maternal and infant health in many ways, particularly physiologically, psychologically, and socially (1). On February 6, 2023, earthquakes with magnitudes of 7.8 and 7.6 struck Turkey, also impacting Syria, resulting in more than 50 000 deaths and over 100 000 injuries, which created significant challenges in providing necessary health services (2). During this period, pregnant women faced difficulties in accessing healthcare providers and antenatal follow-ups, while the living conditions for women who gave birth changed after the earthquake (3).
For maternal and infant health, exclusive breastfeeding for the first six months and continued breastfeeding for two years is recommended for infant nutrition (4). Successful breastfeeding should be initiated within the first hour after birth; a suitable and comfortable position must be adopted, the baby's hunger cues should be monitored, and frequent feedings should be provided. Additionally, mothers should be given adequate fluids, nutrients, education, and social support. An adequate breast milk supply is influenced by various factors, including the mother’s breastfeeding experience, age, occupation, mode of delivery, duration of breastfeeding in the hospital, postpartum depression, and social support (5). In particular, conditions that lead to depression or anxiety are significant risk factors for inadequate breastfeeding (6).
The most critical factor influencing the initiation and maintenance of breastfeeding is the mother’s motivation and self-efficacy to breastfeed (7). The breastfeeding self-efficacy scale is an assessment tool that measures this confidence (8). Scores calculated from this scale have been found to correlate with mothers’ satisfaction and, consequently, with longer breastfeeding duration (9). This scale was first developed in 1999, and its short form was created in 2003. It has since been translated into many languages and utilized in numerous studies (10). The reliability of the scale, as measured by Cronbach's alpha, was found to be above 0.9 in the original study, the short form study, and in other research, demonstrating its safe use in assessing breast milk adequacy (11-13).
Postpartum depression is a factor that affects the success of breastfeeding. The Edinburgh Postpartum Depression Scale (EPDS), developed by Cox et al. in 1987, is used to assess the severity of depression in mothers during the postpartum period. This score evaluates various factors, including mood, energy levels, sleep patterns, appetite, anxiety, and overall psychological well-being after childbirth. It is typically administered through a short questionnaire, with the results providing insights into the presence and severity of depression. A high score on this scale indicates postpartum depression (14).
Regional breastfeeding rates are generally reported in UNICEF's annual Scorecard reports (15). However, specific information on 6-month breastfeeding rates concerning specific issues, such as earthquakes, is not available in the literature. In a study conducted in Croatia among pregnant women exposed to earthquakes during the COVID-19 pandemic, the 6-month breast milk intake rate for their babies was 43.8% (16). According to UNICEF data from 2017, the six-month breastfeeding rate for the entire population in Croatia was 10.7% (17). Although these data suggest that breastfeeding is more successful among mother-baby dyads affected by harsh environmental conditions, there is no evidence-based literature on this topic.
2. Objectives
Therefore, this study was conducted to compare the effect of the Turkey-Syria earthquakes on the breast milk intake rate of infants at 6 months between two groups: Earthquake survivors and non-earthquake survivors. By using the Breastfeeding Self-Efficacy Scale and the EPDS, we aimed to investigate the breastfeeding self-confidence and postnatal depression status of mothers. This is the first study comparing two groups of earthquake survivors and non-earthquake dyads using these scales and reporting the rate of breast milk intake at 6 months.
3. Methods
The study is a single-centre prospective cohort study. All infants admitted to Iskenderun State Hospital within 9 months from February 6, 2023 (February 6, 2023 - November 27, 2023), who met the inclusion criteria, were included in the study, while those who met the exclusion criteria were excluded.
Inclusion criteria were defined as: (1) mothers who were pregnant on February 6, 2023; (2) infants born between February 6, 2023, and November 27, 2023; (3) infants for whom parental consent was obtained. Exclusion criteria were: (1) infants requiring second-level or higher NICU hospitalization; (2) premature infants (< 37 weeks); (3) postterm infants (> 42 weeks); (4) infants with congenital anomalies; (5) infants with metabolic diseases.
Between February 6, 2023, and November 27, 2023, information about the babies admitted to İskenderun State Hospital was obtained from the hospital information system. The families of these babies were contacted through the telephone numbers they provided to the system. Families were informed about the study, and those who accepted to participate were invited for a face-to-face interview when their babies were 6 months old. Informed consent forms were signed by the families after verbal consent was obtained in advance. Questions in the case report form were then administered. This form included demographic characteristics of the mothers and infants, characteristics of the post-earthquake environment, antenatal and postnatal health history, and breastfeeding and other feeding characteristics of the infants. The Breastfeeding Self-Efficacy Short Form and the EPDS were administered to the mothers.
The Breastfeeding Self-Efficacy Short Form was based on the original study and consisted of 14 questions, each of which was formatted as a multiple-choice question with a single answer ranging from 1 to 5, indicating levels of certainty from "not at all sure" to "very sure." The total score for this scale was calculated as the sum of the scores from each question. The EPDS, similarly based on the original study, consisted of 10 questions, each with a single multiple-choice answer ranging from 0 to 3. The score for this scale was calculated as the sum of the scores based on the responses.
The sample size was calculated based on a study that found a breast milk intake rate of 47% after the earthquake in a population with a pre-earthquake breast milk intake rate of 10.7% (16). Using G*Power analysis with a Fisher's exact test for proportions, it was determined that 34 patients were needed in each of the control and study groups (alpha: 0.05, power: 0.95).
In the interim evaluation in April 2024, members of a social messaging application group for mothers who gave birth in July-September 2023 in Turkey were added to the control group to ensure an adequate sample size. Consent was obtained from the volunteers by contacting the members through the application. The relevant questionnaires were administered to this group online.
3.1. Statistical Analysis
The SPSS v.25 software package was used to evaluate the data. In descriptive statistics, categorical variables were expressed as frequency (n) and percentage (%), while continuous variables that fit a normal distribution were expressed as mean ± standard deviation, and those that did not fit a normal distribution were expressed as median (minimum-maximum). The suitability of continuous variables for normal distribution was determined using normality tests. For datasets with fewer than 30 samples (n < 30), the Shapiro-Wilk test was employed, while for datasets with more than 30 samples (n > 30), the Kolmogorov-Smirnov test was used. The chi-square test was utilized for analyzing categorical variables. The independent samples t-test was applied for comparisons of continuous variables between two independent groups when they were normally distributed, and the Mann-Whitney U test was used when they were not. A P-value of < 0.05 was considered statistically significant.
All subjects provided informed consent to participate in the study before enrollment. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Hatay Mustafa Kemal University Non-interventional Research Ethics Committee on October 12, 2023 (decision No: 7.19.16).
4. Results
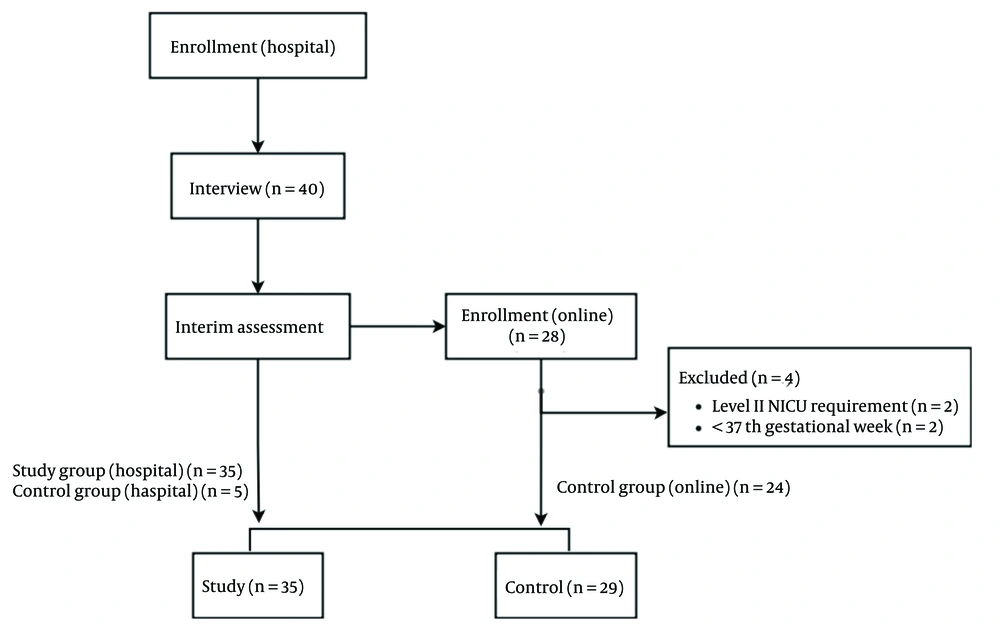
Patients admitted to İskenderun State Hospital within nine months after the earthquake were contacted. Volunteers who met the inclusion criteria and did not meet the exclusion criteria were invited for an interview. Between February 12, 2024, and May 17, 2024, 40 face-to-face interviews were conducted. In these interviews, 5 cases were designated as the control group and 35 cases as the study group.
For the control group, there were 28 subjects who completed an online questionnaire and met the inclusion criteria. Four of these subjects were excluded. Consequently, 24 individuals from the online questionnaires were added to the control group. In total, analyses were performed with 35 subjects in the study group and 29 subjects in the control group (Figure 1).
At the time of the earthquake, the gestational weeks for mothers in the control group were 28 ± 1 (mean ± SD), while those for mothers in the study group were 27 ± 1 (mean ± SD). All participants in the control group were Turkish, whereas 2 participants in the study group were Syrian and 1 was of another nationality. All participants were married. The number of mothers with a profession was statistically significantly higher in the control group than in the study group. Demographic data are presented in Table 1.
| Features | Control (n = 29) | Study (n = 35) | P-Value |
|---|---|---|---|
| Age of mother, year b | 31 + 1 | 29 + 1 | 0.104 |
| Nationality | NA | ||
| Turkish | 29 (100) | 32 (91.4) | |
| Syrian | - | 2 (5.7) | |
| Others | - | 1 (2.9) | |
| Married | 29 (100) | 35 (100) | NA |
| Education status | NA | ||
| Primary school | - | 10 (28.6) | |
| Secondary school | 1 (3.4) | 14 (40.0) | |
| University | 28 (96.6) | 11 (31.4) | |
| Employed mother | 22 (75.9) | 6 (17.1) | < 0.001 |
| Residence | NA | ||
| Home | 29 (100) | 20 (57.1) | |
| Hostel | - | 6 (17.1) | |
| Container | - | 3 (8.6) | |
| Tent | - | 6 (17.1) | |
| Change of residence | - | 26 (74.3) | NA |
| Household | |||
| Number of people c | 3 (1 - 4) | 5 (3 - 15) | < 0.001 |
| Presence of a person other than nuclear family | 8 (27.6) | 15 (42.9) | 0.2 |
| Spoken language other than Turkish | - | 4 (11.4) | NA |
| Loss of labor | 1 (3.4) | 4 (11.4) | 0.366 |
| Loss of property | 1 (3.4) | 12 (34.3) | 0.002 |
| Income less than minimum wage | - | 8 (22.9) | NA |
| Nuclear family in earthquake | |||
| Death | - | 2 (5.7) | NA |
| Hospitalization | - | 1 (2.9) | NA |
| Injury requiring treatment | - | 2 (5.7) | NA |
| Family and friends in earthquake | |||
| Death | 2 (6.9) | 23 (65.7) | < 0.001 |
| Hospitalization | - | 18 (51.4) | NA |
| Injury requiring treatment | 1 (3.4) | 17 (48.6) | < 0.001 |
Abbreviation: NA: non-applicable.
a Values are expressed as No. (%) unless otherwise indicated.
b Values are shown as mean + SD and comparisons were made with the Student's t-test,
c Values are shown as median (minimum-maximum) and comparisons were made by the Mann-Whitney U test.
There was no change in the place of accommodation for the control group after the earthquake, while 74.3% of the study group experienced a change in their accommodation. The most common place of accommodation for the study group was home (57.1%), followed by hotel and tent (17.1%), with containers being the least frequent option (8.6%). After the earthquake, property loss and the number of people living in the home were found to be statistically significantly higher in the study group. There was no significant difference in terms of loss of labor force and the number of people living in the house beyond the nuclear family. The study group also reported a higher number of individuals who died, required hospitalization, or were injured (Table 1).
There was no difference between the control and study groups regarding the presence of morbidity during pregnancy, gestational age at birth, birth weight, and mode of delivery. Similarly, the duration of hospital discharge, breast milk intake rates in the first hour, and the availability of a suitable area for breastfeeding were found to be comparable in both groups. In the control group, there were more nulliparous mothers, and a greater number of individuals had received supplementary food before the 6th month. Conversely, in the study group, family support for infant care was lower, and financial difficulties in infant feeding were more common. Clinical and nutritional characteristics are detailed in Table 2.
| Features | Control (n = 29) | Study (n = 35) | P-Value |
|---|---|---|---|
| Nulliparity | 27 (93.1) | 17 (48.6) | < 0.001 |
| Morbidity during pregnancy | 7 (24.1) | 5 (14.3) | 0.315 |
| Morbidity during postpartum period | - | 4 (11.4) | NA |
| Gestational age (in weeks) b | 39 (37 - 40) | 38 (37 - 41) | 0.815 |
| Birth weight c | 3238 ± 372 | 3303 ± 412 | 0.509 |
| C/s | 20 (69) | 21 (60) | 0.457 |
| Age at postnatal discharge (hour) b | 24 (24 - 120) | 24 (24 - 72) | 0.259 |
| Breastfeeding in first hour of birth | 26 (89.7) | 32 (91.4) | 0.809 |
| Shared baby care with family members | 23 (79.3) | 19 (54.3) | 0.036 |
| Presence of a suitable area for breastfeeding | 26 (89.7) | 27 (77.1) | 0.319 |
| Financial difficulties in infant feeding | 1 (3.4) | 8 (22.9) | 0.033 |
| Last month of breastfeeding c | 6 (2 - 6) | 6 (1 - 6) | 0.280 |
| Any formula feeding before 6 months | 20 (69) | 22 (62.9) | 0.609 |
| Supplementary food before 6 months | 15 (51.7) | 9 (25.7) | 0.032 |
| Water before 6 months | 11 (37.9) | 19 (54.3) | 0.192 |
Abbreviation: C/s, C-section; NA, non-applicable.
a Values are expressed as No. (%) unless otherwise indicated.
b Values are shown as median (minimum-maximum) and comparisons were made by the Mann-Whitney U test.
c Values are shown as mean + SD and comparisons were made with the Student's t-test,
The rate of breast milk intake at 6 months, which is the primary outcome of the study, was found to be 18 (61.1%) in the control group and 22 (62.9%) in the study group. No statistically significant difference was observed between the two groups (P = 0.95) (Table 3).
a Values are expressed as No. (%) unless otherwise indicated.
b Values are shown as median (minimum-maximum) and comparisons were made by Mann-Whitney U test.
The breastfeeding self-efficacy scale score was statistically significantly higher in the study group compared to the control group [64 (33 - 70) vs 54 (31 - 70), median (min-max), P: 0.02]. The EPDS score was 10 (0 - 21), median (min-max) in the control group, while it was 7 (0 - 26), median (min-max) in the study group. Although the score was higher in the control group than in the study group, the difference was not statistically significant (P = 0.58) (Table 3).
5. Discussion
As far as is known, this is the first study comparing mother-infant dyads who are earthquake survivors with those who are non-earthquake survivors, demonstrating the effect of the earthquake on the rate of breast milk intake at the 6th month. The strengths of the study include the pre-determination of the sample size and the use of the breastfeeding self-efficacy scale and the Edinburgh Postnatal Depression Scale as assessment tools through face-to-face interviews with families in the study group.
A challenge encountered during the study was that it was conducted in an earthquake zone, leading many families to be reluctant to volunteer due to issues such as difficulties in transportation to the hospital. The control group was formed from a larger population after the interim evaluation, as the initial hospital interviews did not yield a sufficient number of participants. The addition of a larger population to the control group, which began as a single-center study, and the inclusion of 5 individuals from the earthquake zone during hospital interviews, provided a more appropriate representation of the control group in the study.
Earthquake-related physical and environmental characteristics, which were the main factors investigated in the study, were found more frequently in the study group, as expected. However, statistical comparisons could not be made in the control group due to a lack of data on these variables. The study revealed differences between the groups in several parameters, such as multiparity, timing of initiation of supplementary food, educational status, and participation of family members in infant care (Tables 1 and 2). Although household income, education level, and social status have been positively associated with breastfeeding initiation and duration in developed countries, some studies have found no difference in breastfeeding self-efficacy scores (BSES) across different household incomes, education levels, or family types (5, 7, 8, 11).
Despite the expectation that physical environmental challenges—such as the change in accommodation for 3 out of 4 earthquake survivor mother-infant dyads, property loss in one-third of them, and nearly half accommodating at home—would affect the availability of suitable areas for breastfeeding, the same breastfeeding rates were found in both groups. This suggests that under tough environmental conditions, mothers prioritize their infants’ needs and adopt a protective mindset, thereby strengthening the mother-infant relationship. Consequently, higher self-efficacy scores may have been observed in the study group. A study conducted in Turkey after the earthquake indicated that breastfeeding helped reduce post-traumatic stress disorder during the earthquake period, suggesting that breastfeeding provides protective benefits for both the mother and infant, which supports this perspective (18).
A study comparing cross-sectional feeding before and after the Nepal earthquake two years apart showed that breastfeeding rates in infants younger than six months were higher after the earthquake, although this was not statistically significant (19). Our study employs a different design than that in the literature, comparing infants exposed to the earthquake with those not exposed during the same period, and it found similar breast milk intake rates at the 6th month.
The literature indicates that during the earthquake period, various groups donated formula despite all restrictions, while mothers expressed concerns about providing adequate breast milk (20). Furthermore, it is noted that during natural disasters, the media can influence mothers' preferences for breast milk and formula, potentially affecting breast milk intake (21). Although our study revealed that the study group faced more financial difficulties in infant feeding, there was no significant difference between the two groups regarding formula use before 6 months of age. This finding suggests that there is no decrease in exclusive breastfeeding among earthquake-affected mother-infant dyads compared to other infants, making it unreasonable to provide artificial feeding with formula. A comprehensive review of the literature has shown that resilience is more common than pathological outcomes in natural disasters (22). Therefore, due to this increased resilience, it is believed that BSES were higher in the study group, thereby preventing pathological outcomes.
The mean score in the original study of the breastfeeding self-efficacy short-form scale, an important tool for assessing breastfeeding efficacy, was 55 (13). In a study involving postpartum women, the BSES was also found to be 55 (23). Another study compared the BSES of mothers with healthy and sick babies, reporting scores of 55 for mothers with healthy babies and 52 for those with sick babies (10). In our study, the BSES was 54 (31 - 70), median (min-max) in the control group, consistent with the literature, and 64 (33 - 70), median (min-max) in the study group, which is higher than reported in the literature (P = 0.02). The elevated score in the study group suggests that this may be due to increased resilience in both mothers and infants. The finding of a higher breastfeeding self-efficacy score in the study group supports the hypothesis that in challenging situations, mothers' self-efficacy increases due to their instinct to protect their babies, resulting in a longer breastfeeding duration than expected.
The literature indicates that natural disasters, such as pandemics, earthquakes, and hurricanes, increase the incidence of postnatal depression (24). An Edinburgh Postnatal Depression Score above 12 is indicative of postnatal depression (14). In this study, the median values in both groups were below this threshold. Although the score was higher in the study group than in the control group [7 (0 - 26) vs. 10 (0 - 21)], the median (min-max) difference was not statistically significant (P = 0.58). Therefore, no relationship between the earthquake and postnatal depression could be established. The questions on the EPDS assess the mother's condition over the past week, and it is recommended in the literature that screening be performed in the second postnatal month. Since this study investigated data at the 6th month and the mothers had experienced the initial months—when postnatal depression is more prevalent—there may not have been a significant difference between the groups in EPDS scores. Different results might have emerged if these mothers had been contacted at 2 months old for the EPDS assessment. However, this was not feasible due to environmental conditions. We recommend that future studies take this into account.
In general, although this study compared two groups of earthquake survivors and non-earthquake survivors with available resources, it found that the earthquake did not affect infants' breast milk intake at 6 months. The fact that the control group was drawn from a different population meant that confounding factors could not be analyzed in this study. Therefore, the results will guide future research in this area.
5.1. Conclusions
Major disasters, such as earthquakes, do not significantly alter breast milk intake rates in infants at six months compared to the general population. If breastfeeding is maintained despite deteriorating environmental conditions, mothers' breastfeeding self-confidence increases, protecting both the mother and baby from negative factors. The most important need for the baby in the first six months is its mother, and artificial feeding should not be encouraged unless medically necessary.