1. Context
2. Evidence Acquisition
Articles were searched in the databases of PubMed, Web of Science, Google Scholar, and Scopus from 1960 to 2024. The keywords for our research included "clubfoot", "relapse" or "recurrence", "Ponseti method", "treatment" or "management", "imaging", "anatomy", and "genetics". Articles in languages other than English or those for which the full text was not accessible were excluded.
3. Results
3.1. Anatomy of Clubfoot
In this position, the shape of the foot resembles a golf club, which is why this deformity is called "clubfoot" (3). The acronym "CAVE" summarizes the changes that occur in clubfoot: C stands for Cavus, A stands for Adduction, V stands for Varus, and E stands for Equinus (4). These changes are explained in the following paragraphs.
3.1.1. Cavus
The contracture of the plantar and spring ligaments, along with increased plantar flexion of the first metatarsal bone, results in an increased longitudinal arch of the foot (4).
3.1.2. Adduction
The forefoot is adducted, with the cuneiforms and metatarsals deviating toward the midline while maintaining a normal shape (4).
3.1.3. Varus
This involves the inversion and adduction of the hindfoot, where the heel forms a varus angulation. The calcaneus is in varus, plantar-flexed, and rotated inward below the talus, nearly aligning in the same line (4).
3.1.4. Equinus
The foot exhibits increased plantar flexion at the ankle joint. The calcaneo-pedis block rotates internally around the head of the talus (Figure 1) (4).
3.2. Etiology
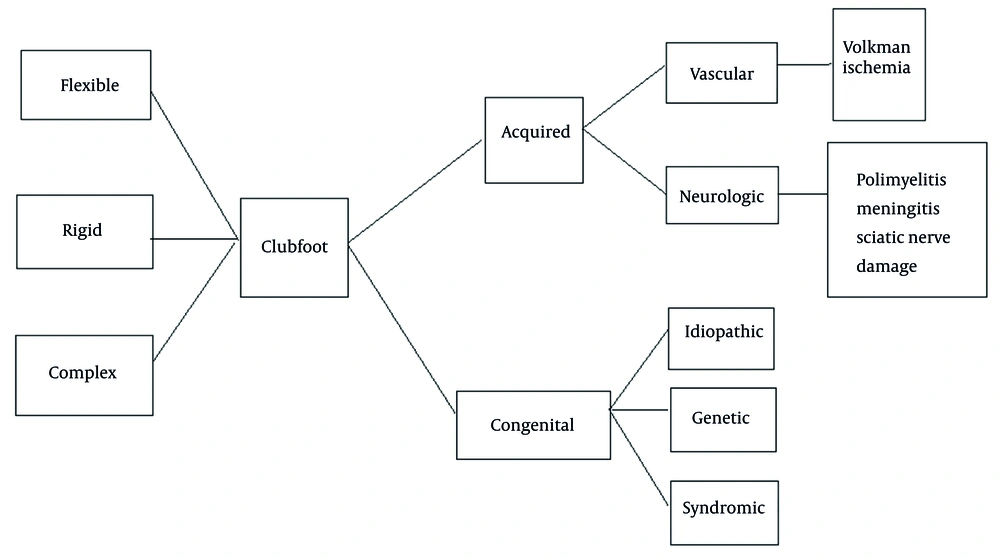
The etiologies of clubfoot are typically classified into two main groups: congenital and acquired. Acquired forms of clubfoot usually occur after birth and are further subdivided into vascular and neurogenic causes. Vascular causes include conditions such as Volkmann ischemic paralysis, while neurogenic causes include diseases such as poliomyelitis, meningitis, or sciatic nerve damage (5). The types of congenital clubfoot are subdivided into idiopathic, neurogenic (e.g., spina bifida, myelomeningocele), and syndromic (e.g., arthrogryposis) (6). Idiopathic clubfoot is the most common type. It is an isolated congenital abnormality, often bilateral, and generally responds better to conservative therapies (5).
Many researchers suggest that genetic factors play a significant role in the development of clubfoot (7, 8). Studies indicate that monozygotic twins affected by clubfoot exhibit approximately 35% genetic concordance, reinforcing the hereditary component of the condition (9). Additionally, nearly one-quarter of all clubfoot cases are familial, further supporting the role of genetic predisposition (9). Various theories propose that multiple genes and their polymorphisms contribute to the pathogenesis of clubfoot. Specific genes involved in muscle formation and limb development — such as those in the PITX1-TBX4 transcriptional pathway, chromosome 17q23, and the HOX gene family — have been investigated due to their potential association with an increased risk of clubfoot. Furthermore, genes involved in xenobiotic metabolism, including NAT1, NAT2 (linked to the modulation of tobacco smoke), and CYP1A, have also been studied in relation to clubfoot susceptibility (8).
Given the high genetic heterogeneity of clubfoot, researchers recommend the use of advanced genomic techniques such as whole-genome sequencing (WGS) and whole-exome sequencing (WES) to further explore its genetic basis in diverse populations. One study conducted by Milanovic et al. examined 50 randomly selected children with clubfoot, aged 3 to 16 years, who had been initially hospitalized and treated between November 2006 and November 2022 (8). Based on the presence of genetic mutations identified through WES, patients were categorized into two groups: those with confirmed genetic mutations and those without. The results revealed that seven patients carried genetic mutations. A significant association was observed between a family history of clubfoot and the presence of genetic mutations, with over half (57.14%) of mutation-positive cases also having a familial history of clubfoot (8).
Similarly, Charng et al. conducted a study involving exome sequencing of 1,190 individuals with non-syndromic clubfoot and their family members across multiple ethnic backgrounds. To assess the burden of ultra-rare genetic variants, they compared 857 unrelated clubfoot cases of European ancestry with two independent ethnicity-matched control groups. Their findings showed that rare variants in 29 genes, including PITX1 (a well-established clubfoot-associated gene), HOXD12, COL12A1, COL9A3, and LMX1B, were more frequently observed in clubfoot cases. Additionally, rare variants in posterior HOX genes (HOX9–13) were significantly enriched in affected individuals. Overall, genetic variants in these genes were detected in 8.4% (100 out of 1,190) of clubfoot cases across both European and non-European populations. Among them, three were de novo variants, while 22 exhibited variable penetrance, including four HOXD12 variants that segregated with clubfoot. Based on these findings, the study identified HOXD12 as a novel gene associated with clubfoot (7).
Early amniocentesis, performed before 13 weeks of gestation, has been linked to a higher risk of clubfoot compared to chorionic villus sampling or amniocentesis performed later in pregnancy (10). However, amniocentesis is an uncommon risk factor for clubfoot (11). Unlike positional foot deformities such as metatarsus adductus, which are more common in twin pregnancies, there is little evidence linking clubfoot to late-gestational uterine compression (12). No association has been found between Vitamin D intake during pregnancy and the incidence of clubfoot in neonates (13). There are different degrees of clubfoot severity, including flexible clubfoot, rigid clubfoot, and complex clubfoot. Flexible clubfoot can be easily manipulated into a corrected position, while rigid clubfoot is more resistant to correction (14). Complex clubfoot involves additional abnormalities in the foot and ankle, requiring more extensive treatment (Figure 2) (15).
3.3. Work Up
3.3.1. Diagnosis
Prenatal ultrasonography is highly beneficial for diagnosing clubfoot, particularly in developed countries. At 13 weeks' gestational age, transvaginal sonography is used (16), and at 16 weeks' gestational age, transabdominal sonography is employed to detect this abnormality (17). However, the diagnosis of clubfoot is usually made at 20 weeks of gestational age. In a study conducted by Bogers et al. (18), the diagnosis of clubfoot during the first trimester was not advised because transient clubfoot develops at this time as a normal stage of lower limb development. The positive predictive value for prenatal ultrasonography examination is over 80%. If there is an uncertain ultrasonography result, MRI can be helpful (19). MRI is not used as a regular screening method because its effects on the developing fetus are uncertain and the cost is high (20).
There are some weaknesses in ultrasound diagnosis, and results are strongly variable based on the age of pregnancy and the experience of the radiologist (21). It is important to note that a normal sonography result cannot always rule out clubfoot, and the diagnosis of mild or moderate clubfoot can be missed during the prenatal period. On the other hand, the false positive rate of idiopathic clubfoot on prenatal ultrasonography is between 10% and 40% (22), as sometimes a mild positional deformity can be falsely diagnosed as clubfoot. Also, the severity of clubfoot cannot be assessed during ultrasound examination. The insistence on prenatal diagnosis is to facilitate the timely referral of the parents to a clinician, typically a pediatric orthopedic surgeon. This early referral aims to inform parents about the available treatment modalities and to correct the deformity as soon as possible (21, 23).
3.3.2. Physical Examination
The physical examination of a patient with clubfoot typically involves assessing the severity of the foot deviation and ruling out any other health problems (14). Additionally, muscle strength and flexibility in the foot and ankle should be evaluated (6). When examining a newborn with clubfoot, a complete physical examination is essential to assess the patient’s general health. This examination should extend beyond a basic orthopedic evaluation of the limbs and include an investigation of potential medical syndromes (6, 14). Therefore, developmental milestones, as well as the face and hands of the patient, should be carefully examined (14). Neurological conditions and diseases such as spina bifida and myelomeningocele must also be considered (6). The range of motion and stability of all joints should be assessed. Radiographs can be recommended for patients with other congenital malformations (24). The lower limbs should also be examined for symmetry. It is crucial to differentiate between postural and rigid clubfoot. In patients with postural clubfoot, the deformity can be fully corrected by passive manipulations. The severity of clubfoot is determined more by the flexibility of the foot than by its appearance (14). The difficulty of correcting clubfoot is more related to the rigidity than to the severity of the deformity (6). The infant’s feet should be examined gently, ensuring that the examination is conducted while the baby is in a relaxed state (14).
Canavese and Dimeglio suggest following a five-step strategy to comprehensively examine the foot (14).
3.3.2.1. Palpation of the Heel
The heel area should be palpated to check for the presence of the calcaneus. The objective is to determine if the calcaneus bone is present. An empty heel sign may suggest a dislocated or absent calcaneus.
3.3.2.2. Assessment of the Lateral Border of the Foot
The lateral border of the foot should be observed and palpated. A convex lateral border may indicate a deformity.
3.3.2.3. Evaluating the Reducibility of the Foot on All Planes
On the horizontal plane, rotation of the calcaneo-tarsal complex and forefoot adduction should be checked to measure how well the foot can be repositioned, indicating its rigidity. On the sagittal plane, the equinus should be evaluated to assess the foot’s ability to dorsiflex, which is crucial for normal walking. On the frontal plane, the hindfoot varus should be examined to assess the alignment of the heel relative to the leg.
3.3.2.4. Examining the Tonicity of Muscles
Assessing muscle tone is crucial to identify any neuromuscular disorders in newborns with clubfoot. Muscle tone is evaluated through passive manipulation and is classified into three categories: hypotonic, normal, and hypertonic.
3.3.2.5. Examining Other Joints
Joints such as hips, knees, shoulders, and elbows should be assessed for subluxation, dislocation, or deformities. Dorsalis pedis and tibial artery pulses are generally detectable, but there is a possibility of vascular malformation. Therefore, it is crucial to evaluate the blood flow in the forefoot and ankle (14).
3.4. Pirani Scoring System
The Pirani score is an effective method for assessing the severity and treatment progress in children with clubfoot. It is recognized for its ease of use and reliability in evaluating the condition and monitoring treatment (14). Additionally, studies by Dyer and Davis and Mejabi et al. have found a significant positive correlation between the initial Pirani score and the number of casts needed to correct the clubfoot deformity (25, 26). This scoring system assesses six clinical signs of clubfoot: three signs are examined in the midfoot, and three are examined in the hindfoot. The score given to each examination varies between 0, 0.5, and 1 based on the severity. If the abnormality is severe, the score is 1. If it is partially abnormal, the score is 0.5, and if it is normal, it scores 0 (14, 27).
3.4.1. Midfoot Contracture Scores (0 to 3)
3.4.1.1. Medial Crease Examination
For this examination, the foot position should be corrected, for example, by lifting the foot while holding the second toe. Then the depth of the crease and the presence of other creases should be assessed. If several fine creases are present, the score is 0. If two or three moderate creases are present, the score is 0.5. In the presence of a single and deep crease where the bottom is not visible, the score is 1 (27).
3.4.1.2. Curved Lateral Border Examination
The examiner should ensure that the foot is relaxed. Then the plantar aspect of the foot should be observed, using a pen held against the lateral edge of the calcaneum. The deviation point on the lateral border of the foot should be assessed. If the foot’s border is straight without deviation, the score is 0. If the foot’s deviation is at the level of the metatarsals, the score is 0.5. If the border deviates at the calcaneo-cuboid joint, the score is 1 (27).
3.4.1.3. Lateral Head of Talus Examination
The examiner should initially move the foot into a more deformed position and then gently correct the foot. If the talus completely sinks away under the navicular, the score is 0. If the talus moves partially but not completely, the score is 0.5. If the talus is fixed, the score is 1 (27).
3.4.2. Hindfoot Contracture Scores (0 to 3)
3.4.2.1. Posterior Crease Examination
For this examination, the plantar flexion of the foot should be corrected gently. The score is 0 if several fine creases are present. If two or three moderate creases are present, the score is 0.5. If there is a single, deep crease, the score is 1 (27).
3.4.2.2. Empty Heel Examination
The foot should be positioned in mild correction. The heel is palpated with a single index finger to feel the calcaneum. If the calcaneum is not far under the skin and is easy to palpate, the score is 0. If the calcaneum is palpated through a layer of muscle, the score is 0.5. If the calcaneum is felt with difficulty and is under a deep layer of tissue, the score is 1 (27).
3.4.2.3. Rigid Equinus Examination
For this examination, the plantarflexion should be corrected as much as is comfortable for the child, while the knee is in a straight position. Then the degree of obtained dorsiflexion is assessed. If it is more than 90 degrees, the score is 0. If it is 90 degrees, the score is 0.5. If it is less than 90 degrees, the score is 1 (27).
All scores from the six examinations are summed up for the final result, with the total score ranging from 0 to 6.
3.5. Dimeglio Classification
The Dimeglio classification is a widely used system for assessing and grading the severity of clubfoot. This classification aids in selecting the optimal treatment plan and monitoring therapeutic progress. It assigns scores to four primary deformities of clubfoot — equinus, heel varus, medial rotation of the calcaneopedal block, and forefoot adduction — based on the severity of the deformities (28, 29). The assigned score reflects the reducibility of the deformity, with additional points allocated for the presence of a posterior crease, medial crease, cavus deformity, and poor muscle condition. The total score ranges from 4 to 20 (Tables 1 and 2) (30).
| Major Components Reducibility (Degrees) | Score | Other Parameters | Score |
|---|---|---|---|
| 90 - 45 | 4 | Posterior crease | 1 |
| 45 - 20 | 3 | Medial crease | 1 |
| 20 - 0 | 2 | Cavus | 1 |
| < 0 to - 20 | 1 | Poor muscle condition | 1 |
| Classification | Type | Score |
|---|---|---|
| Grades | ||
| 1 | Benign | < 5 |
| 2 | Moderate | 5 - 10 |
| 3 | Severe | 10 - 15 |
| 4 | Very severe | 15 - 20 |
3.6. Imaging
3.6.1. X-ray
Despite ongoing debate, there is no consensus on the value of routine X-ray evaluation in managing clubfoot cases (4). Standard radiographs do not provide a definitive method for evaluating and managing clubfoot, primarily because most tarsal bones are not ossified, with the exceptions of the talus and calcaneus, which appear as rounded ossicles on plain radiographs. The ossification centers of the metatarsal bones are visible at birth and become sufficiently ossified by 3 to 4 months of age (31). Radiological information is typically obtained from standing anteroposterior and lateral views, with specific measurements used to assess clubfoot. These measurements include the angle between the talus and calcaneus in both planes and the relationship of the calcaneal equinus to the tibia’s longitudinal axis (4, 14). Meary’s angle, the angle between the long axes of the first metatarsal and the talus, indicates forefoot cavus (4, 32). Evaluating bone morphology, including the flattening of the talar head and subluxation of the navicular bone, is crucial in assessing clubfoot. Navicular bone ossification around age five allows for a more precise foot evaluation, which should be repeated at age ten. This thorough clinical and radiographic assessment at ages five and ten is essential for objectively evaluating outcomes (29).
3.6.2. Ultarsonography and Magnetic Resonance Imaging
Ultrasound is a valuable imaging modality for examining soft tissues, ligaments, and joint structures in clubfoot. It allows real-time visualization of dynamic foot movements, making it particularly useful for evaluating the flexibility and reducibility of the deformity. Ultrasound can also identify associated anomalies, such as tendon abnormalities or joint contractures, which may impact treatment planning (33). Additionally, ultrasound-guided interventions, such as Achilles tenotomy, can be precisely performed under real-time imaging guidance (34).
MRI provides detailed cross-sectional images of muscles, tendons, ligaments, and joints in clubfoot. It is indicated when there is a suspicion of complex soft tissue abnormalities, such as neurovascular compression, muscle abnormalities, or joint pathology. MRI helps differentiate between fibrous tissue and muscle bulk, assess tendon integrity, and guide surgical planning in cases requiring soft tissue releases (29, 35). MRI can provide a more precise characterization of clubfoot deformities and has the potential to identify recurrences and complications of clubfoot earlier than traditional X-ray imaging (35).
3.7. Primary Management
The treatment of clubfoot should begin as soon as possible after birth, ideally within the first three weeks (36). The earlier the treatment starts, the better the results, as an infant’s bones and joints are more flexible, allowing the deformity to be corrected more easily and with less invasive procedures. Lack of treatment or improper treatment can cause functional harm, resulting in alterations in the bone structures (37). Although the best treatment choice is conservative, the degree of clubfoot can change the overall management. Non-operative treatments are mostly preferred for mild and flexible clubfoot. In severe cases, surgery may be added to the conservative plan. Surgery primarily involves releasing tight tendons or ligaments and should be considered for severe or rigid clubfoot deformities that do not respond to conservative treatments, but it should not be extensive (38). It is recommended to postpone surgical treatments until the infant is between six and nine months old (39).
The Ponseti method is a non-surgical treatment approach for clubfoot that involves three main parts: a series of manipulations and casting (with or without Achilles tenotomy) to correct the foot and the use of an orthosis to maintain the correction (40). The Ponseti method is the gold standard for treatment (41) and is accepted worldwide as a life-changing treatment (42). It is also a suitable treatment for non-idiopathic clubfoot (43).
In the manipulation and casting phase, manipulations and weekly serial above-knee castings are conducted by an expert in this technique (Figure 3) (44). After this phase, 90% of patients need to undergo Achilles tenotomy surgery (45). Pre-term infants treated at term needed a similar number of casts and tenotomies to achieve initial correction as term infants (46). After full correction of clubfoot, and immediately after removing the casts, a foot abduction orthosis (FAO) should be used to maintain the correction. This brace is made up of two shoes connected by a bar (Denis-Browne model). The feet are held shoulder-width apart by this bar (6). When the affected foot is placed in the FAO, it is kept in 60 to 70 degrees of external rotation and 10 to 15 degrees of dorsiflexion, while the unaffected foot is placed in 30 degrees of external rotation (47, 48). During the first three months after cast removal, the brace should be worn 24 hours a day approximately. After that, the time can be progressively reduced to night and siesta time when the child starts to stand and will be used only during nighttime after the acquisition of gait (49). It is now recommended to wear the brace until the age of five to minimize the risk of relapses (49). The most important factor in the final result of treatment and the prevention of recurrence is compliance with the bracing phase by both the patient and the parents (50). The initial success rate of treatment with the Ponseti method is above 90% (51).
The Ponseti method has been reported to significantly decrease the need for extensive corrective surgery and can be used in children, preferably up to 2 years old, even after previous unsuccessful non-surgical treatments (52). In a study conducted by Verma et al., the initial success rate of the Ponseti method for children between the ages of 1 to 3 years was 89% (53). The Ponseti method has been shown to be highly effective in treating clubfoot deformity with minimal risk of complications in short- and mid-term follow-ups (54). However, a systematic review by Rastogi and Agarwal indicated that there are high relapse and surgery rates in infants with primary idiopathic clubfoot treated with the Ponseti method in long-term follow-ups (55). This study highlighted the importance of long-term follow-up and adhering to treatment for children with clubfoot, given the potential for late relapses and secondary late changes.
3.8. Alternative Approaches to Clubfoot Treatment
Although the Ponseti method remains the gold standard for treating clubfoot, alternative treatment approaches have been introduced over the years to provide clinicians with additional options. The following paragraphs discuss some of these methods.
3.8.1. The French Functional Method
This conservative approach to treating clubfoot is based on daily physiotherapy sessions aimed at achieving a gradual and painless correction. It follows specific sequences, ensuring a progressive improvement in foot alignment. The sequence of manipulations in French functional method (FFM) adheres to the same principles as the Ponseti method, beginning with talo-navicular joint reduction followed by lateral derotation of the calcaneo-forefoot unit (56). However, unlike the Ponseti method, which uses serial casting for acute corrections, FFM involves daily manual manipulations with an emphasis on stretching the triceps surae to enhance tibio-talar joint function (56, 57).
Over time, the FFM technique has evolved, incorporating additional measures. One such measure is percutaneous Achilles tenotomy, which, unlike in the Ponseti method, is not routinely performed (58). Instead, it is reserved for cases where tibio-talar dorsiflexion is less than 10° at walking age, aiming to improve range of motion. Another modification includes the use of above-knee casts with semi-rigid tapes or Perlstein leather night bracing to manage mild residual deformities — such as ankle dorsiflexion between 0° and 10°, a calcaneal-thigh angle between 10° and 20°, dynamic cavus, or adduction—and to prevent recurrence (57).
French functional method should ideally be performed by physiotherapists specifically trained in this method, as it follows precise guidelines tailored to each patient’s deformity severity. All manipulations and immobilizations must be executed gradually and carefully to avoid complications such as midfoot breaks. Additionally, supportive immobilization techniques — such as strapping, above-knee splints, and leather night bracing — are employed solely to maintain the achieved correction between sessions rather than to impose or force further correction (57).
A study by Souchet et al. included all patients treated with FFM for clubfoot between 1993 and 2010, covering a total of 779 feet. According to the International Clubfoot Study Group (ICFSG) evaluation system, 86% of these cases achieved excellent to good outcomes, exhibiting minimal residual deformities or minor radiological imperfections (56).
3.8.2. The Hybrid Method
The two primary approaches for treating congenital clubfoot are the Ponseti method and the FFM. While the Ponseti method relies on serial casting, FFM is based on manual manipulations (57). Despite their differing clinical approaches, both techniques have demonstrated high efficacy, reliability, and durable results. The primary goal of both methods is to achieve a pain-free, flexible, and plantigrade foot while minimizing the need for surgical intervention. However, neither the Ponseti method nor FFM can completely eliminate the necessity for surgery in all cases.
In an effort to further reduce surgical rates, Canavese et al. introduced the hybrid method, which integrates the advantages of both approaches (29, 57). Specifically, the hybrid method combines the serial casting technique of the Ponseti method with the manipulative assessments used in FFM. The goal is to achieve long-term correction while ensuring full foot functionality and pain-free mobility (29, 57).
In their initial 2017 study, Canavese et al. reported an 8.7% posterior release rate among a cohort of 92 clubfeet treated using the hybrid method. Their findings suggested that gentle pre- and post-casting manipulations performed by skilled physiotherapists could enhance outcomes, lower surgical rates, and accelerate foot correction (29). A subsequent study, conducted by the same team (14), was published in 2021 and further evaluated the hybrid method. Between May 2010 and August 2020, 139 newborns with congenital clubfoot (66 unilateral and 73 bilateral) were treated using this protocol and retrospectively analyzed. The surgical rate among children treated between 2010 and 2014 was 8.7%, whereas in the later cohort (2015 - 2020), it dropped to 6%. Notably, the hybrid method not only reduced the need for surgery but also minimized the extent of surgical interventions. These findings indicate that as experience with the hybrid method has grown, the need for surgical intervention has consistently decreased, both in terms of frequency and surgical extent (59).
3.9. Follow-up
Clubfoot is a complex orthopedic disorder requiring continuous management to sustain correction, avoid relapse, and mitigate functional impairments. The role of follow-up care is crucial in evaluating the outcomes of treatment, monitoring growth and development, and addressing any residual deformities or complications that may occur after treatment. During follow-up appointments, it is important to assess patient compliance with treatment protocols, particularly the correct use of orthoses and braces (14, 29). To accurately monitor the progression of the initial treatment’s correction, consistent and unbiased clinical evaluations are essential. Therefore, scheduling follow-up appointments at intervals of one to two years is recommended (29).
During growth, clinical assessment of the foot should include an evaluation of the overall foot morphology, the identification of any deformities, the mobility of the subtalar joint, plantar and dorsal flexion of the ankle, calf muscle atrophy, and the anatomical alignment of the lower limb (14). Functional assessments should examine the patient’s ability to perform activities such as toe and heel walking, descending stairs, standing on one leg, rope jumping, and walking on uneven surfaces. Additionally, the assessment should identify any abnormalities in gait type and severity (14). Ensuring compliance with brace usage is vital for relapse prevention. Initially, clinicians should demonstrate the correct application of the brace to the family and verify that they can apply it properly. If difficulties arise, it may be beneficial to schedule a follow-up visit within one week to ensure proper application techniques are being followed (60). Early identification of relapses allows for more efficient and effective management. Following the commencement of post-corrective bracing, patients should be scheduled for evaluations every 3 to 4 months, especially within the first two years due to the rapid growth phase of the foot (60).
3.10. Relapse
Relapse is defined as the recurrence of one or more of the deformities of clubfoot in a patient after initial treatment and correction (61). The most prevalent presentations of relapse are equinus and adductus, which can occur in isolation or in combination, with or without dynamic supination (62). Relapse of the deformity occurs in more than 40% of patients treated with the Ponseti method in some centers. However, if relapse occurs after the Ponseti method, it is easier to manage and the outcomes are more predictable than relapses that occur after invasive treatments (61).
There are various causes for the relapse of clubfoot. Poor compliance, particularly with brace wear, is one of the most significant reasons for relapses. The discomfort associated with braces or lack of cooperation from parents are the most common reasons for non-compliance (43). Other factors influencing relapse include early cessation of brace use, the severity of clubfoot, soft tissue contractures, muscle imbalance, genetic predisposition, and undiagnosed neuromuscular conditions (62, 63). It is important to understand and pay attention to various causes and mechanisms of relapse to prevent and manage relapse in the best possible way.
Relapsed clubfoot deformities present with varying degrees of severity, ranging from mild residual deformities to complete recurrence of the original malalignment. Timely recognition of relapsed clubfoot allows for prompt intervention to prevent further progression and optimize outcomes (61). The management of relapsed clubfoot involves a tailored approach based on the individual patient's clinical presentation, previous treatment history, and underlying risk factors (64, 65). Non-operative interventions, such as brace wear, physiotherapy, and serial casting, may be effective in addressing mild relapses and maintaining correction. In cases of severe deformity or failed conservative measures, surgical options, including soft tissue releases, osteotomies, or tendon transfers, may be considered to achieve proper realignment and functional outcomes. Close monitoring, patient education, and long-term follow-up are essential components of relapse management to prevent future recurrence and ensure sustained correction (66).
3.11. Casting Alone
Patients treated with the Ponseti method exhibit more flexibility and less stiffness in their feet compared to those initially treated with surgical methods. Consequently, recasting is a desirable approach for treating relapse in these patients (61). Recasting should adhere to the rules and principles of the Ponseti method (61). The use of braces during nighttime is crucial after recasting. Given that non-compliance with orthoses and braces is a major cause of relapse, educating parents about the importance of brace use and close follow-ups must be integral to the treatment plan. Additionally, parents should be instructed on the correct use of orthoses and braces (61).
3.12. Soft Tissue Release
Soft tissue release can be indicated for patients with stiffer feet and severe relapses where non-surgical procedures, such as casting alone, have been ineffective in obtaining full correction (1). There are two surgical techniques used for soft tissue release: the "A la carte" approach and the "One-size-fits-all" approach (67).
3.12.1. A la Carte Procedure
The a la carte procedure is a selective approach tailored to the patient’s specific anatomical abnormalities. The goal is to minimize surgical intervention to preserve as much functionality and mobility as possible. Rather than performing a full release of soft tissues, only the tight structures that impede proper alignment are released (67, 68).
3.12.2. One-Size-Fits-All Procedure
This method involves a complete soft tissue release through a circumferential incision, aiming to correct all aspects of the deformity in a single surgery. However, it generally results in more post-operative complications and is not favored these days (69, 70).
The a la carte procedure is usually preferred, as it leads to fewer complications, greater muscle strength, and better radiological outcomes (1, 67, 68, 70).
3.13. Bony Osteotomies
3.13.1. Midfoot Osteotomies
These procedures are typically indicated for clubfoot patients exhibiting residual adduction deformity (71). They are generally performed on patients who are either beyond the optimal age for soft tissue release or not old enough for arthrodesis, usually within the age range of 4 to 8 years (72).
3.13.2. Hindfoot Osteotomies
Historically, the Dwyer calcaneal osteotomy was the preferred technique for addressing varus heel deformities. However, it has fallen out of favor due to its high complication rates (72). Alternatively, a lateralization slide osteotomy is now commonly used to correct varus heel deformities in adolescents and young adults (72).
3.13.3. Supramalleolar Osteotomies
This technique is applied to correct rigid deformities of the midfoot and hindfoot when soft tissue interventions are no longer viable (73).
3.14. Achilles Tenotomy or Lengthening
For patients with equinus deformity unresponsive to casting, particularly in early relapses, the equinus may be due to an incomplete initial tenotomy or the erroneous non-indication of tenotomy. In patients younger than 2 years old, an Achilles tenotomy is often the treatment of choice. In older patients, however, Z-plasty lengthening of the Achilles tendon is typically performed (61). Some patients also present with a cavus deformity, which can accentuate the appearance of equinus. For these patients, casting is a useful option (74). If tightness of the plantar fascia persists despite casting, a plantar fascia release may be performed during the tenotomy (66).
3.15. Tibialis Anterior Tendon Transfer
Tibialis anterior tendon transfer (TATT) is a commonly performed procedure for treating relapsed clubfoot in patients initially treated with the Ponseti method. It is most frequently indicated for patients exhibiting dynamic supination during the swing phase of gait. The TATT should be considered when the foot demonstrates dynamic supination but can otherwise be passively corrected. The optimal approach is to first attempt to align the deformity with casting. Post-casting, the foot should be reassessed to determine whether surgery is necessary. If dorsiflexion without supination is achieved after casting, surgery might not be required. In cases where equinus contracture is present alongside dynamic supination, Achilles tendon lengthening or gastrocnemius recession may also be performed during surgery.
The timing of the TATT procedure is crucial for its success. Performing TATT before adequate ossification of the lateral cuneiform increases the risk of relapse. It is mostly indicated for stopping the use of the splint in children who are older than 5 to 6 years old (61). The recurrence rate for a second relapse following the TATT procedure is approximately 15% (75).
3.16. Ilizarov Correction
Severe and persistent clubfoot deformities can be managed through gradual correction using Ilizarov techniques (76, 77). Initial flexibility can be achieved through a combination of osteotomies and soft tissue release, which then facilitates a gradual correction into a plantigrade position (64, 65).
3.17. Patient Education and Engagement
Educating patients and caregivers about the significance of follow-up care is crucial for ensuring adherence to treatment recommendations and brace-wearing protocols. Many relapses are attributed to non-compliance and improper use of braces, highlighting the necessity for parents to be thoroughly educated on the importance of braces and the correct methods for their use (66). A study by Kumari et al. on the lived experience of parents of children with clubfoot revealed that participants emphasized the need for comprehensive awareness programs for the general public, potentially as part of government policy. Such initiatives could enhance societal knowledge and mitigate the negative impact faced by parents. Therefore, it is essential to understand the caregiver’s role and the associated challenges to improve the lives of affected children (78).
Despite adequate treatment, idiopathic clubfoot continues to exert physical, emotional, and social effects on both affected children and their families (79). Addressing these emotional and social effects is a critical component in educating parents of children with clubfoot.
4. Conclusions
Clubfoot is one of the most prevalent pediatric musculoskeletal deformities worldwide. Although different research indicates a genetic component in the occurrence of clubfoot, there is a notable lack of studies focusing on the specific genes involved. The initial treatment for clubfoot is the Ponseti method; however, there is a high relapse rate associated with this approach. One of the major causes of relapse is non-compliance with brace wearing after the Ponseti treatment. Therefore, educating parents on the correct use of braces and emphasizing their importance is crucial. Despite this, there is limited research on other causes of relapse and their effects. Various methods exist for managing clubfoot relapse depending on its severity, but there is no consensus on the optimal treatment approach. Further investigation into the causes of relapse and effective management strategies is necessary.