1. Background
Cardiac surgery and the use of cardiopulmonary bypass (CPB) during the neonatal period are intricate procedures designed to rectify congenital heart anomalies. Despite significant improvements in survival rates resulting from these interventions, it is imperative to consider the potential risks they bring. Significant fluid and electrolyte imbalances can occur in neonatal patients undergoing cardiac surgery due to blood loss and the utilization of CPB (1). Patient outcomes may be negatively affected by these perioperative electrolyte disturbances. Electrolyte imbalances cause changes in essential ion levels, leading to acute and chronic complications. Maintaining the precise balance of electrolytes is essential for cellular homeostasis, optimal neuromuscular function, and overall organ health. Imbalances in these levels can have harmful impacts, especially for critically ill neonates. Electrolyte imbalances can directly affect the functions of neonatal kidneys. The occurrence of acute kidney injury (AKI) poses a significant concern, as it is associated with increased morbidity and prolonged hospitalization in neonatal cardiac patients following surgery. Limited research has been conducted on the association between imbalances in sodium or chloride levels and AKI following pediatric cardiac surgery (1). Using various cardioplegia options during CPB can effectively address abnormal myocardial sodium depletion and minimize the incidence of hypochloremia in neonates (2).
One of the most common electrolyte disturbances seen in hospitalized patients is dysnatremia, characterized by sodium imbalances. While the impact of dysnatremia has been associated with increased infection complications, coronary events, and hospital mortality in adults following cardiac surgery, its effect on pediatric patients with heart disease remains understudied (3, 4). It is important to note that arrhythmias occurring in neonates shortly after surgery are primarily caused by direct injury to the cardiac conduction system, or edema and inflammation in the myocardial tissue surrounding the conduction pathways. Factors such as electrolyte imbalances, acidosis or alkalosis, patient age during surgery, CPB duration, and hemodynamic status can also affect the occurrence and frequency of arrhythmias (5, 6). Recent studies have revealed a higher prevalence of postoperative hypernatremia compared to hyponatremia in infants, which is linked to increased mortality rates, adverse neurological outcomes, and prolonged hospitalizations (7, 8). Acute hypernatremia can affect synaptic structure and function in the central nervous system (9). The careful selection of intravenous fluid therapy during surgery and CPB is imperative in avoiding dysnatremia (10). Proper recognition and management of electrolyte imbalances are vital for perioperative care, particularly in pediatric cardiac patients, as it has a direct impact on patient outcomes. By gaining a deeper understanding of these imbalances in a clinical setting, we can enhance the quality of care and make a positive difference in patient outcomes. Additional research is required to enhance the management of electrolytes in this vulnerable population.
2. Objectives
The present study aimed to assess the occurrence of electrolyte imbalances during the perioperative, intraoperative, and postoperative phases in neonates undergoing congenital cardiac surgery and their effects on morbidity (e.g., renal failure and seizures) and mortality. Based on these findings, the study seeks to offer valuable insights into preventive measures and clinical enhancements that can improve long-term health outcomes and contribute to the current evidence. Additionally, this study intends to assess electrolyte imbalances in pediatric patients with AKI and arrhythmia comorbidities.
3. Methods
3.1. Participants
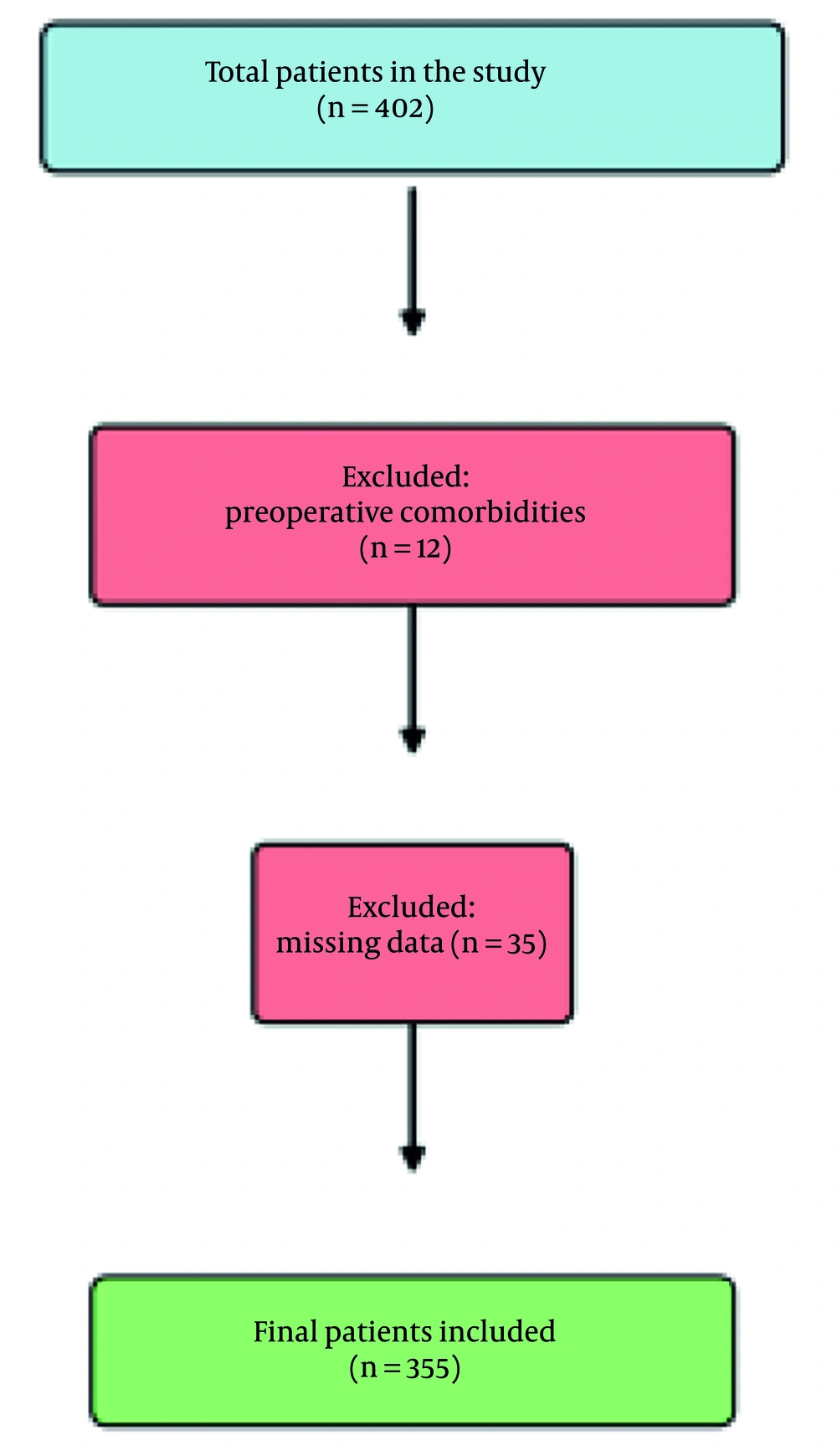
The present retrospective study was conducted at a single center between January 2021 and January 2024 within a tertiary city hospital. The study involved neonates under one month old diagnosed with congenital heart disease who underwent cardiac surgery within this timeframe. Patients presenting with syndromic conditions, preoperative neurological comorbidities, renal failure, or arrhythmias were omitted from the analysis to establish a more standardized preoperative health status within the study sample. Patients with missing data were also excluded from the study. Following the application of the inclusion and exclusion criteria, 355 cases (both male and female) were examined (Figure 1).
3.2. Research Design
This study was a retrospective cohort analysis aimed at investigating the influence of perioperative electrolyte disturbances on postoperative outcomes, such as AKI, arrhythmia, seizure, and mortality, in neonates undergoing cardiac surgery. Data were obtained from patient medical records during the preoperative, intraoperative, and postoperative phases. The primary variables of interest were sodium, potassium, chloride, and calcium levels, which were assessed at designated time points: Preoperatively (blood gas sample taken in the operating room before surgery initiation), intraoperatively (blood gas sample taken in the operating room at the end of surgery), and postoperatively (blood gas sample taken at the 6th hour of postoperative intensive care admission). The assessed outcomes included the duration of postoperative intensive care unit (ICU) stay, seizures, AKI, arrhythmias, requirement for extracorporeal membrane oxygenation (ECMO), and mortality.
3.3. Measures
Electrolyte levels served as the key metrics in this research, utilizing predetermined thresholds to classify abnormal levels. Abnormal sodium levels were defined as less than 135 mmol/L or greater than 145 mmol/L potassium imbalances were described as levels less than 3.5 mmol/L or greater than 5.5 mmol/L chloride imbalances were defined when levels were below 98 mmol/L or above 107 mmol/L hypocalcemia was characterized by serum calcium levels below 8.5 mg/dL, while hypercalcemia was defined as levels exceeding 10.5 mg/dL. Age-specific thresholds were used to detect phosphorus irregularities. Data on electrolyte values were collected from medical records at the specified time points.
Secondary measures such as AKI were ascertained using the Kidney Disease: Improving global outcomes (KDIGO) criteria, while arrhythmias were identified through electrocardiographic findings observed during the patient’s stay in the ICU (11). Seizures were identified during the ICU stay by motor symptoms typically seen in epileptic seizures and a clear and detailed clinical description by the treating intensivists, including postictal cessation of symptoms and recovery of consciousness and/or neurological status. Mortality rates and the requirement for ECMO assistance were documented from patient medical files.
3.4. Statistical Analysis
Descriptive statistics were employed to summarize the baseline characteristics of the study population, encompassing demographic variables and the occurrence of perioperative electrolyte imbalances. Continuous variables, such as electrolyte levels and CPB duration, were documented as either means ± standard deviations or medians with interquartile ranges, depending on the distribution of the data. Categorical variables, such as arrhythmia occurrences or mortality rates, were presented as frequencies and percentages. Categorical variables between groups with and without electrolyte abnormalities were compared using the chi-square test or Fisher’s exact test. Continuous variables were examined using t-tests or Mann-Whitney U tests following assessments of normality. Logistic regression models were employed to examine the links between perioperative electrolyte imbalances and outcomes, such as AKI, arrhythmia, and mortality. A P-value lower than 0.05 was regarded as statistically significant. Statistical analyses were carried out utilizing R version 4.3.3 provided by the R Foundation for Statistical Computing in Vienna, Austria. The study was conducted in accordance with the Declaration of Helsinki and was approved by the University of Health Sciences Turkiye, Basaksehir Cam and Sakura city Hospital Local Ethics Committee (28.02.2024.130).
4. Results
Among the 355 patients, ages ranged from 0 to 1 month, with a median age of 0.3 months and an average age of 0.406 ± 0.30 months. Patient heights varied from 39 to 62 cm, with a median height of 50 cm and a mean of 50.175 ± 3.30 cm, suggesting a homogeneous distribution. Similarly, the weight range was from 1.6 to 5.8 kg, with a median weight of 3.1 kg (IQR: 0.70) and an average weight of 3.2 ± 0.64 kg, indicating a consistent neonatal weight distribution within this group of patients.
The length of anesthesia showed considerable variation, spanning from 95 to 810 minutes, with a median duration of 340 minutes. The CPB duration also exhibited significant variability, ranging from 0 to 545 minutes, with a median duration of 110 minutes. Postoperative ICU stays ranged from 1 to 180 days, with a median stay of 12 days and a mean stay of 16.70 ± 18.62 days. Hospital stays followed a comparable pattern, lasting from 1 to 180 days, with a median stay of 17 days and an average stay of 21.59 ± 18.62 days, demonstrating differences in recovery times and postoperative outcomes in the group.
4.1. Acute Kidney Injury
The research revealed significant distinctions between patients with AKI and those without. Hyponatremia was more prevalent in the AKI group (46.43%) compared to the non-AKI group (27.68%) before the operation (P = 0.002). Similarly, hypocalcemia was significantly more prevalent in patients with AKI (53.57% vs. 32.47%, P < 0.001), while hypochloremia also displayed a notable difference, occurring more frequently in the AKI population (22.62% vs. 11.81%, P = 0.022). No significant differences were found in other preoperative electrolyte disturbances between the groups.
Intraoperatively, a significantly higher proportion of patients in the AKI group exhibited persistent hypernatremia (42.86%) compared to the control group (24.72%) (P = 0.002), and there was also a greater prevalence of hypokalemia (61.90% vs. 46.86%, P = 0.022).
Post-surgery, AKI patients demonstrated notably higher rates of hypernatremia (59.52% vs. 14.39%, P < 0.001) and hyperchloremia (61.90% vs. 35.06%, P < 0.001). There were no significant differences between the two groups in terms of other post-surgery electrolyte imbalances, including hypokalemia, hyperkalemia, hypocalcemia, and hypochloremia (Table 1).
| Variables | Overall (N = 355) | Non-AKI Group (N = 271) | AKI Group (N = 84) | P-Value |
|---|---|---|---|---|
| Preoperative | ||||
| Hyponatremia | 114 (32.11) | 75 (27.68) | 39 (46.43) | 0.002 |
| Hypernatremia | 7 (1.97) | 4 (1.48) | 3 (3.57) | 0.363 |
| Hypokalemia | 116 (32.68) | 83 (30.63) | 33 (39.29) | 0.179 |
| Hyperkalemia | 32 (9.01) | 26 (9.59) | 6 (7.14) | 0.640 |
| Hypocalcemia | 133 (37.46) | 88 (32.47) | 45 (53.57) | < 0.001 |
| Hypercalcemia | 5 (1.41) | 4 (1.48) | 1 (1.19) | > 0.999 |
| Hypochloremia | 51 (14.37) | 32 (11.81) | 19 (22.62) | 0.022 |
| Hyperchloremia | 58 (16.34) | 40 (14.76) | 18 (21.43) | 0.202 |
| Intraoperative | ||||
| Hyponatremia | 10 (2.82) | 7 (2.58) | 3 (3.57) | 0.706 |
| Hypernatremia | 103 (29.01) | 67 (24.72) | 36 (42.86) | 0.002 |
| Hypokalemia | 176 (49.58) | 144 (53.14) | 32 (38.10) | 0.022 |
| Hyperkalemia | 22 (6.20) | 14 (5.17) | 8 (9.52) | 0.235 |
| Postoperative | ||||
| Hypernatremia | 89 (25.07) | 39 (14.39) | 50 (59.52) | < 0.001 |
| Hypokalemia | 201 (56.62) | 159 (58.67) | 42 (50.00) | 0.202 |
| Hyperkalemia | 12 (3.38) | 7 (2.58) | 5 (5.95) | 0.251 |
| Hypocalcemia | 226 (63.66) | 178 (65.68) | 48 (57.14) | 0.196 |
| Hyperchloremia | 147 (41.41) | 95 (35.06) | 52 (61.90) | < 0.001 |
Abbreviation: AKI, acute kidney injury.
a Values are expressed as No. (%).
4.2. Arrhythmia
We examined variations in laboratory results in patients with and without arrhythmia, focusing on electrolyte imbalances before, during, and after surgery. Significant variations were evident preoperatively, with hypocalcemia being notably more prevalent in the arrhythmia group (50.65% vs. 33.81%, P = 0.010). Despite the higher occurrence of hyponatremia and hypokalemia in the arrhythmia group (40.26% for both) compared to the non-arrhythmia group (29.86% and 30.58%, respectively), these disparities did not show statistical significance (P = 0.111 for hyponatremia, P = 0.143 for hypokalemia).
Hypernatremia was detected in a larger proportion of patients with arrhythmia (37.66%) based on blood tests performed during surgery, but this variation was not statistically significant (P = 0.081). Similarly, the arrhythmia group had a lower rate of hypokalemia (40.26%) compared to the non-arrhythmia group (52.16%), indicating a potential significance (P = 0.086).
After surgery, distinct disparities were identified in the blood test results across the groups, particularly in hypernatremia and hyperchloremia. Patients diagnosed with arrhythmia exhibited a marked increase in hypernatremia (50.65% vs. 17.99%, P < 0.001), alongside an elevated prevalence of hyperchloremia (62.34% vs. 35.61%, P < 0.001). Although hypocalcemia was significantly more frequent in subjects with arrhythmia before the operation, there was a slight decrease postoperatively, and the controls had a higher hypocalcemia rate (66.91% vs. 51.95%, P = 0.023) (Table 2).
| Variables | Overall (N = 355) | Non-arrhythmia Group (N = 278) | Arrhythmia Group (N = 77) | P-Value |
|---|---|---|---|---|
| Preoperative | ||||
| Hyponatremia | 114 (32.11) | 83 (29.86) | 31 (40.26) | 0.111 |
| Hypernatremia | 7 (1.97) | 6 (2.16) | 1 (1.30) | > 0.999 |
| Hypokalemia | 116 (32.68) | 85 (30.58) | 31 (40.26) | 0.143 |
| Hyperkalemia | 32 (9.01) | 25 (8.99) | 7 (9.09) | > 0.999 |
| Hypocalcemia | 133 (37.46) | 94 (33.81) | 39 (50.65) | 0.010 |
| Hypercalcemia | 5 (1.41) | 4 (1.44) | 1 (1.30) | > 0.999 |
| Hypochloremia | 51 (14.37) | 37 (13.31) | 14 (18.18) | 0.371 |
| Hyperchloremia | 58 (16.34) | 42 (15.11) | 16 (20.78) | 0.309 |
| Intraoperative | ||||
| Hyponatremia | 10 (2.82) | 8 (2.88) | 2 (2.60) | > 0.999 |
| Hypernatremia | 103 (29.01) | 74 (26.62) | 29 (37.66) | 0.081 |
| Hypokalemia | 176 (49.58) | 145 (52.16) | 31 (40.26) | 0.086 |
| Hyperkalemia | 22 (6.20) | 15 (5.40) | 7 (9.09) | 0.356 |
| Hypocalcemia | 53 (14.93) | 42 (15.11) | 11 (14.29) | > 0.999 |
| Hypercalcemia | 145 (40.85) | 113 (40.65) | 32 (41.56) | 0.990 |
| Postoperative | ||||
| Hypernatremia | 89 (25.07) | 50 (17.99) | 39 (50.65) | < 0.001 |
| Hypokalemia | 201 (56.62) | 161 (57.91) | 40 (51.95) | 0.421 |
| Hyperkalemia | 12 (3.38) | 10 (3.60) | 2 (2.60) | > 0.999 |
| Hypocalcemia | 226 (63.66) | 186 (66.91) | 40 (51.95) | 0.023 |
| Hyperchloremia | 147 (41.41) | 99 (35.61) | 48 (62.34) | < 0.001 |
a Values are expressed as No. (%).
4.3. Seizure
Seizures were documented in 17 (4.7%) of the 355 patients in our study group during postoperative intensive care monitoring. When all electrolyte imbalances in blood gas analyses at three time points were compared, none showed a statistically significant association with seizure occurrence (P > 0.05) (Table 3).
| Variables | Overall (N = 355) | Non-seizure Group (N = 338) | Seizure Group (N = 17) | P-Value |
|---|---|---|---|---|
| Preoperative | ||||
| Hyponatremia | 114 (32.11) | 109 (32.15) | 5 (29.41) | > 0.999 |
| Hypernatremia | 7 (1.97) | 6 (1.77) | 1 (5.88) | 0.292 |
| Hypokalemia | 116 (32.68) | 110 (32.45) | 6 (35.29) | > 0.999 |
| Hyperkalemia | 32 (9.01) | 31 (9.14) | 1 (5.88) | > 0.999 |
| Hypocalcemia | 133 (37.46) | 127 (37.46) | 6 (35.29) | > 0.999 |
| Hypercalcemia | 5 (1.41) | 5 (1.47) | 0 (0.00) | > 0.999 |
| Hypochloremia | 51 (14.37) | 47 (13.86) | 4 (23.53) | 0.282 |
| Hyperchloremia | 58 (16.34) | 55 (16.22) | 3 (17.65) | 0.746 |
| Intraoperative | ||||
| Hyponatremia | 10 (2.82) | 8 (2.36) | 2 (11.76) | 0.077 |
| Hypernatremia | 103 (29.01) | 97 (28.61) | 6 (35.29) | 0.750 |
| Hypokalemia | 176 (49.58) | 165 (48.67) | 11 (64.71) | 0.298 |
| Hyperkalemia | 22 (6.20) | 21 (6.19) | 1 (5.88) | > 0.999 |
| Hypocalcemia | 53 (14.89) | 49 (14.45) | 4 (23.53) | 0.297 |
| Hypercalcemia | 145 (40.73) | 139 (41.00) | 6 (35.29) | 0.830 |
| Postoperative | ||||
| Hypernatremia | 89 (25.07) | 84 (24.78) | 5 (29.41) | 0.886 |
| Hypokalemia | 201 (56.62) | 191 (56.34) | 10 (58.82) | > 0.999 |
| Hyperkalemia | 12 (3.38) | 11 (3.24) | 1 (5.88) | 0.449 |
| Hypocalcemia | 226 (63.66) | 216 (63.72) | 10 (58.82) | 0.880 |
| Hypercalcemia | 2 (0.56) | 2 (0.59) | 0 (0.00) | > 0.999 |
| Hypochloremia | 25 (7.02) | 24 (7.08) | 1 (5.88) | > 0.999 |
| Hyperchloremia | 147 (41.29) | 136 (40.12) | 11 (64.71) | 0.079 |
a Values are expressed as No. (%).
4.4. Mortality
Finally, we examined the discrepancies in electrolyte imbalances prior to, during, and following surgery among patients who survived and those who did not. Before the surgery, there were notable differences in the occurrence of hyponatremia, which was more prevalent in the group that passed away (45.98%, P = 0.002). The occurrence of hypocalcemia was markedly higher in non-survivors (50.57% vs. 32.84%, P = 0.004), as was hypochloremia (24.14% vs. 11.19%, P = 0.005).
Hypernatremia demonstrated a notable rise among the deceased during or shortly after the procedure (41.38% vs. 25.00%, P = 0.005). Similarly, hypokalemia was found to be more prevalent in the group experiencing mortality (63.22% vs. 46.64%, P = 0.010). Post-surgery, in patients who deceased, hypernatremia (56.32% vs. 14.93%, P < 0.001) and hyperchloremia (59.77% vs. 35.07%, P < 0.001) were notably more prevalent. Moreover, there was a higher incidence of hypocalcemia in the group that experienced mortality (47.13% compared to 32.84%, P = 0.023). The mortality subgroups did not show notable differences in other electrolyte imbalances in potassium (Table 4).
| Variables | Overall (N = 355) | No Mortality (N = 268) | Mortality (N = 87) | P-Value |
|---|---|---|---|---|
| Preoperative | ||||
| Hyponatremia | 114 (32.11) | 74 (27.61) | 40 (45.98) | 0.002 |
| Hypernatremia | 7 (1.97) | 4 (1.49) | 3 (3.45) | 0.369 |
| Hypokalemia | 116 (32.68) | 81 (30.22) | 35 (40.23) | 0.110 |
| Hyperkalemia | 32 (9.01) | 27 (10.07) | 5 (5.75) | 0.313 |
| Hypocalcemia | 132 (37.18) | 88 (32.84) | 44 (50.57) | 0.004 |
| Hypercalcemia | 5 (1.41) | 4 (1.49) | 1 (1.15) | > 0.999 |
| Hypochloremia | 51 (14.37) | 30 (11.19) | 21 (24.14) | 0.005 |
| Hyperchloremia | 57 (16.06) | 39 (14.55) | 18 (20.69) | 0.235 |
| Intraoperative | ||||
| Hyponatremia | 10 (2.82) | 7 (2.61) | 3 (3.45) | 0.712 |
| Hypernatremia | 103 (29.01) | 67 (25.00) | 36 (41.38) | 0.005 |
| Hypokalemia | 175 (49.30) | 143 (53.36) | 32 (36.78) | 0.010 |
| Hyperkalemia | 22 (6.20) | 14 (5.22) | 8 (9.20) | 0.281 |
| Hypocalcemia | 53 (14.93) | 39 (14.55) | 14 (16.09) | 0.859 |
| Hypercalcemia | 145 (40.85) | 110 (41.04) | 35 (40.23) | 0.993 |
| Postoperative | ||||
| Hypernatremia | 89 (25.07) | 40 (14.93) | 49 (56.32) | < 0.001 |
| Hypokalemia | 200 (56.34) | 155 (57.84) | 45 (51.72) | 0.382 |
| Hyperkalemia | 12 (3.38) | 7 (2.61) | 5 (5.75) | 0.287 |
| Hypocalcemia | 226 (63.66) | 180 (67.16) | 46 (52.87) | 0.023 |
| Hyperchloremia | 146 (41.13) | 94 (35.07) | 52 (59.77) | < 0.001 |
a Values are expressed as No. (%).
Further investigation through regression analysis was conducted to understand the connection between electrolyte imbalances and the risk of mortality. An association between preoperative hyponatremia and mortality was observed in the univariable analysis, with an odds ratio (OR) of 0.80 (95% CI, 0.30 - 1.3; P = 0.002). After adjusting for other factors in the multivariable analysis, hyponatremia was still identified as a significant indicator of mortality (OR, 0.77; 95% CI, 0.22-1.3; P = 0.006).
The presence of preoperative hypocalcemia was identified as a significant predictor of mortality in the univariable model (OR, 0.74; 95% CI, 0.25 - 1.2; P = 0.003); however, it only approached significance in the multivariable model (P = 0.074). Hypochloremia emerged as another crucial factor, demonstrating a notable correlation with mortality in both univariable (OR, 0.93; 95% CI, 0.30 - 1.5; P = 0.003) and multivariable analysis (OR, 0.79; 95% CI, 0.09 - 1.5; P = 0.025).
No significant relationships with mortality were observed for other electrolyte imbalances, such as preoperative hypernatremia, hypokalemia, hyperkalemia, and hypercalcemia, in either univariable or multivariable analyses.
5. Discussion
Perioperative electrolyte imbalances were found to be closely connected to critical outcomes, such as AKI, arrhythmia, and mortality, as highlighted in this study. Our research aligns with existing data, emphasizing the crucial role of monitoring and correcting electrolyte levels, especially in at-risk groups, to enhance recovery after surgery.
Preoperative hyponatremia, hypocalcemia, and hypochloremia were notably more prevalent in patients who experienced AKI compared to those who did not. The findings presented are in line with the study by Formeck et al., which emphasized hyponatremia as a pivotal factor influencing the prognosis of AKI patients (12). Hyponatremia in AKI is often linked to impaired renal handling of sodium and water, exacerbating fluid imbalances and leading to poorer prognoses (8, 13, 14).
Reinforcing our results, Lin et al. illustrated the correlation between intraoperative and postoperative hypernatremia and increased mortality among cardiac patients, underscoring the importance of meticulous intraoperative fluid control (9). In our study, both intraoperative hypernatremia and hypokalemia were more prevalent in the AKI group, reinforcing the critical role of perioperative electrolyte control. CoŞKun et al. reported that hypernatremia and hyperchloremia in postoperative AKI patients are associated with poorer renal outcomes and increased mortality (15). While the administration of postoperative free water is a topic of debate, there is a consensus on the unfavorable outcome (10, 16, 17).
Our research on arrhythmia revealed important electrolyte disruptions, notably preoperative hypocalcemia, among patients with arrhythmia. Pillai et al. established a link between hypocalcemia and critical morbidity and mortality, especially in patients undergoing major surgical interventions (18). Calcium is crucial for the proper functioning of the heart muscle, and a lack of it can cause disturbances in the heart’s electrical activity, resulting in irregular heartbeats (5, 19). Although preoperative hyponatremia and hypokalemia did not show statistical significance in our research, their increased occurrence in the arrhythmia group corresponds to literature, which presents that imbalances in sodium and potassium can lead to arrhythmias by interfering with the electrolyte equilibrium for cardiac stability (6, 7, 20).
Furthermore, the occurrence of postoperative hypernatremia and hyperchloremia, which were notably higher in patients with arrhythmia in our study, aligns with the conclusions drawn by Ganea et al., who highlighted the impact of perioperative sodium and chloride imbalances on postoperative arrhythmias and cardiac issues (21). The results emphasize the necessity of perioperative electrolyte surveillance, especially in high-risk patients for arrhythmias, to avoid unfavorable cardiac consequences.
Strong links were noted between certain electrolyte imbalances and the likelihood of patient survival in terms of mortality. Preoperative hyponatremia, hypocalcemia, and hypochloremia were significant predictors of mortality, consistent with the literature that preoperative hyponatremia is associated with a significantly increased risk of in-hospital mortality (4, 22, 23). Studies have indicated that hyponatremia can exacerbate outcomes in critically ill individuals by interfering with cellular processes and leading to organ dysfunction (3, 24). Current evidence has demonstrated that hyperchloremia plays a role in exacerbating metabolic acidosis and deteriorating renal and cardiac function in critically ill patients (25-27). These results underscore the significance of managing sodium and chloride imbalances during the perioperative phase to enhance patient outcomes.
The present study shows that electrolyte imbalances, particularly disruptions in sodium, calcium, and chloride levels, play a significant role in affecting postoperative results. Recent studies have affirmed the crucial impact of these disruptions on AKI, arrhythmia, and mortality. The strong associations we have recognized, particularly in hyponatremia, hypernatremia, and hypocalcemia, highlight the significance of precise electrolyte correction protocols, especially for neonates with congenital heart disease who have undergone cardiac surgery.
5.1. Conclusions
This study revealed a significant correlation between perioperative electrolyte imbalances and adverse outcomes, including AKI, arrhythmia, and mortality. The results of our study indicate that specific electrolyte abnormalities before and after surgery are important indicators of poor outcomes in high-risk surgical groups. The increasing frequency of electrolyte disruptions in patients with AKI and arrhythmia, as well as their strong link to mortality, underscores the vital need for proactive monitoring of electrolyte levels and timely interventions. Prompt correction of imbalances, specifically those concerning sodium, calcium, and chloride, might mitigate postoperative complications and enhance survival rates among these at-risk cohorts.
Future research should focus on enhancing protocols and exploring targeted interventions to reduce the impact of electrolyte imbalances on postoperative outcomes, thereby improving patient prognosis and decreasing mortality rates.
5.2. Limitations
Despite its strengths, this study has several limitations. First, its retrospective and single-center design may limit the generalizability of our findings. The study population was derived from a single tertiary hospital, which may not fully represent variations in surgical and perioperative management across different institutions. Additionally, we were unable to account for all potential confounders, such as specific fluid management protocols, variations in electrolyte correction strategies, and the impact of different anesthetic techniques. However, in our study, anesthesia and fluid management protocols were standardized for all patients, and the same anesthesiologist was responsible for intraoperative management in all cases. This consistency minimizes variations related to anesthetic and fluid administration.
Future prospective studies with larger multicenter cohorts are needed to validate our findings and explore potential interventions aimed at mitigating electrolyte-related complications.