1. Background
In-hospital mortality rate among hospitalized children is a significant indicator that, alongside the primary measure of under-five child mortality (1), serves as a crucial tool for healthcare planning and management in any country. Moreover, analyzing in-hospital mortality can help assess healthcare quality and monitor mortality trends. Although hospital-based mortality reviews may not fully reflect all causes of death within the general population, they provide a valuable opportunity to investigate the immediate and underlying causes of mortality in healthcare settings (2). By analyzing these assessments, high-risk patients can be identified and better managed. According to the World Health Organization, investigating hospital mortality can significantly enhance clinical performance and improve survival rates of hospitalized patients (3). Numerous studies have been conducted worldwide, particularly among children, reporting varied results (4-7). Several studies have also been conducted in Iran. According to existing research, 80% of hospital mortality occurs in the under-five age group (8, 9). Various social and economic factors influence the hospital mortality rate in any society. A precise depiction of in-hospital mortality can significantly aid in identifying the causes of these deaths, pinpointing preventable factors, and designing effective interventions to avert similar fatalities. The pediatric intensive care unit (PICU), equipped with specialized facilities and instruments, is designed to treat critically ill children rapidly. However, due to the limited availability of dedicated pediatric ICUs in general teaching hospitals, many children are admitted to adult ICUs. The PICU admission aims to monitor, support, and maintain vital system capacities in infants and children, which requires skilled personnel and appropriate equipment (10). Many of these patients require intensive care, including mechanical ventilation. Consequently, caring for these patients imposes significant financial burdens on families and society (11, 12). The duration of PICU admission varies depending on the underlying condition (13). Mortality and complications are more prevalent among patients with extended hospital stays and severe illnesses compared to those with shorter admissions (14). Previous findings have shown that the limitation or withdrawal of life-sustaining treatment in PICU contributes to mortality rates ranging from 14% to 75% (15, 16).
2. Objectives
This study aimed to investigate the documented leading cause of death and the most common causes of mortality among patients admitted to the PICU of Bandar Abbas Children's Hospital during 2023.
3. Methods
3.1. Study Design
This research utilized a retrospective study design to analyze mortality cases over a one-year period in the PICU at Bandar Abbas Children's Hospital. The study period spanned from April 2023 to March 2024, encompassing all cases of patient mortality that occurred within the specified timeframe.
3.2. Data Collection
Medical records of all deceased patients admitted to the PICU during the study period were meticulously reviewed and retrieved. A pre-designed checklist was employed to systematically collect key information, including patient age, sex, underlying medical conditions at the time of death, length of hospital stay, and duration of stay in the PICU. Cases with incomplete or missing records were excluded from the study to ensure data integrity. The inclusion criteria for this research encompassed all deceased patients aged 28 days to less than 18 years admitted to the PICU during the specified one-year period.
3.3. Statistical Analysis
Data analysis was conducted using SPSS software version 21. Descriptive statistics were used to summarize demographic and clinical characteristics. Continuous variables, such as age and hospital or PICU stay duration, were reported as mean values with standard deviations. Categorical variables, including sex and leading cause of death, were expressed as frequencies and percentages. The t-test or an appropriate non-parametric equivalent was applied for inferential analysis to compare continuous variables based on their distribution. The chi-square test was used to examine associations between categorical variables. Additionally, the seasonal distribution of mortality cases was analyzed by categorizing the data into four groups corresponding to the four seasons.
4. Results
The mortality rate in the PICU was calculated to be approximately 60.4%, with a total of 125 deaths recorded among 207 admissions. Out of all cases, 65 (52%) were female and 60 (48%) were male. Age distribution of the cases was categorized as follows: Under one year (48 cases, 38.4%), 1 to 5 years (38 cases, 30.4%), 5 to 10 years (28 cases, 22.4%), and over ten years (11 cases, 8.8%). Furthermore, the distribution of mortality based on seasonal occurrence was reported as follows: Spring (31 cases, 24.8%), summer (18 cases, 14.4%), autumn (30 cases, 24%), and winter (46 cases, 36.8%) (Table 1).
| Variables | Values |
|---|---|
| Gender | |
| Boy | 60 (48.0) |
| Girl | 65 (52.0) |
| Age (y) | |
| Less than 1 | 48 (38.4) |
| 1 to 5 | 38 (30.4) |
| 5 to 10 | 28 (22.4) |
| More than 10 | 11 (8.8) |
| Season | |
| Spring | 31 (24.8) |
| Summer | 18 (14.4) |
| Autumn | 30 (24.0) |
| Winter | 46 (36.8) |
| Total | 125 |
a Values are expressed as No. (%).
The average length of hospital stay was 7.35 ± 8.34 days (ranging from 0 to 58 days), while the average length of stay in the PICU was 5.48 ± 6.20 days (ranging from 0 to 41 days). The leading causes of mortality among children admitted to the PICU were as follows: Infections (52 cases, 41.3%), other and unknown causes (30 cases, 23.8%), neurological diseases (9 cases, 7.1%), respiratory diseases (8 cases, 6.3%), malignancies (7 cases, 5.6%), cardiovascular diseases (7 cases, 5.6%), renal diseases (5 cases, 4%), gastrointestinal diseases (4 cases, 3.2%), congenital and chromosomal abnormalities (2 cases, 1.6%), and endocrine diseases (1 case, 0.8%) (Table 2). The most common leading cause of mortality for both genders was infections, with 20 cases (16%) among males and 32 cases (25.6%) among females. According to the χ2 test, no significant difference was found between the leading cause of mortality and gender (P = 0.181).
| Diagnoses | Gender | P-Value b | ||
|---|---|---|---|---|
| Boy | Girl | Total | ||
| Infections | 20 (16.0) | 32 (25.6) | 52 (41.3) | 0.321 |
| Other and unknown | 17 (13.6) | 13 (10.4) | 30 (23.8) | 0.453 |
| Neurological diseases | 5 (4.0) | 4 (3.2) | 9 (7.1) | 0.512 |
| Respiratory diseases | 5 (4.0) | 3 (2.4) | 8 (6.3) | 0.278 |
| Malignancies | 4 (3.2) | 3 (2.4) | 7 (5.6) | 0.642 |
| Cardiovascular diseases | 3 (2.4) | 4 (3.2) | 7 (5.6) | 0.524 |
| Kidney diseases | 3 (2.4) | 2 (1.6) | 5 (4.0) | 0.611 |
| Gastrointestinal diseases | 3 (2.4) | 1 (0.8) | 4 (3.2) | 0.436 |
| Congenital anomalies | 0 (0.0) | 2 (1.6) | 2 (1.6) | 0.728 |
| Endocrine diseases | 0 (0.0) | 1 (0.8) | 1 (0.8) | 0.829 |
| Total | 60 (48.0) | 65 (52.0) | 125 (100) | 0.118 |
a Values are expressed as No. (%).
b χ2 test.
Infections were the predominant cause of mortality, affecting all age groups. Notably, there were no statistically significant differences across the age groups (P = 0.323; Table 3).
| Diagnoses | Age (y) | P-Value b | |||
|---|---|---|---|---|---|
| Under 1 | 1 to 5 | 5 to 10 | Above 10 | ||
| Infections | 20 (16.0) | 13 (10.4) | 12 (9.6) | 7 (5.6) | 0.263 |
| Other and unknown | 11 (8.8) | 10 (8.0) | 8 (6.4) | 1 (0.8) | 0.432 |
| Neurological diseases | 4 (3.2) | 0 (0.0) | 3 (2.4) | 2 (1.6) | 0.541 |
| Respiratory diseases | 4 (3.2) | 3 (2.4) | 1 (0.8) | 0 (0.0) | 0.389 |
| Malignancies | 0 (0.0) | 2 (1.6) | 3 (2.4) | 2 (1.6) | 0.510 |
| Cardiovascular diseases | 3 (2.4) | 1 (0.8) | 0 (0.0) | 2 (1.6) | 0.601 |
| Kidney diseases | 0 (0.0) | 1 (0.8) | 2 (1.6) | 2 (1.6) | 0.470 |
| Gastrointestinal diseases | 3 (2.4) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0.354 |
| Congenital anomalies | 1 (0.8) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0.625 |
| Endocrine diseases | 0 (0.0) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0.480 |
| Total | 47 (37.6) | 33 (26.4) | 29 (23.2) | 16 (12.8) | 0.323 |
a Values are expressed as No. (%).
b χ2 test.
Mortality (55.2%, 69 cases) occurred in children with a PICU stay of 1 - 7 days. For stays under 24 hours, deaths were mainly due to unspecified causes and infections. The leading cause of mortality significantly varied with the duration of PICU stay (P = 0.014; Table 4).
| Diagnoses | Duration of Stay in PICU (d) | P-Value b | |||
|---|---|---|---|---|---|
| Under 1 | 1 to 7 | 7 to 14 | Above 14 | ||
| Infections | 5 (4.0) | 32 (25.6) | 9 (7.2) | 6 (4.8) | 0.028 |
| Other and unknown | 20 (16.0) | 10 (8.0) | 0 (0.0) | 0 (0.0) | < 0.001 |
| Neurological diseases | 1 (0.8) | 6 (4.8) | 0 (0.0) | 2 (1.6) | 0.291 |
| Respiratory diseases | 0 (0.0) | 3 (2.4) | 3 (2.4) | 2 (1.6) | 0.092 |
| Malignancies | 2 (1.6) | 4 (3.2) | 0 (0.0) | 1 (0.8) | 0.768 |
| Cardiovascular diseases | 0 (0.0) | 7 (5.6) | 0 (0.0) | 0 (0.0) | 0.142 |
| Kidney diseases | 1 (0.8) | 2 (1.6) | 2 (1.6) | 0 (0.0) | 0.269 |
| Gastrointestinal diseases | 1 (0.8) | 3 (2.4) | 0 (0.0) | 0 (0.0) | 0.773 |
| Congenital anomalies | 0 (0.0) | 1 (0.8) | 1 (0.8) | 0 (0.0) | 0.381 |
| Endocrine diseases | 0 (0.0) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0.845 |
| Total | 30 (24.0) | 69 (55.2) | 15 (12.0) | 11 (8.8) | 0.014 |
Abbreviation: PICU, pediatric intensive care unit.
a Values are expressed as No. (%).
b χ2 test.
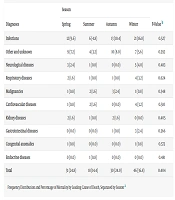
The highest mortality occurred in winter. Infections were the leading cause of death in all seasons. There was no statistically significant difference in the leading cause of mortality across the seasons (P = 0.404; Table 5).
| Diagnoses | Season | P-Value b | |||
|---|---|---|---|---|---|
| Spring | Summer | Autumn | Winter | ||
| Infections | 12 (9.6) | 6 (4.8) | 13 (10.4) | 21 (16.8) | 0.527 |
| Other and unknown | 9 (7.2) | 4 (3.2) | 10 (8.0) | 7 (5.6) | 0.392 |
| Neurological diseases | 3 (2.4) | 1 (0.8) | 0 (0.0) | 5 (4.0) | 0.483 |
| Respiratory diseases | 2 (1.6) | 1 (0.8) | 1 (0.8) | 4 (3.2) | 0.624 |
| Malignancies | 1 (0.8) | 2 (1.6) | 3 (2.4) | 1 (0.8) | 0.348 |
| Cardiovascular diseases | 1 (0.8) | 2 (1.6) | 0 (0.0) | 4 (3.2) | 0.510 |
| Kidney diseases | 2 (1.6) | 1 (0.8) | 2 (1.6) | 0 (0.0) | 0.405 |
| Gastrointestinal diseases | 0 (0.0) | 0 (0.0) | 1 (0.8) | 3 (2.4) | 0.366 |
| Congenital anomalies | 1 (0.8) | 0 (0.0) | 0 (0.0) | 1 (0.8) | 0.573 |
| Endocrine diseases | 0 (0.0) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0.481 |
| Total | 31 (24.8) | 18 (14.4) | 30 (24.0) | 46 (36.8) | 0.404 |
a Values are expressed as No. (%).
b χ2 test.
5. Discussion
This study was carried out with the belief that understanding the leading causes of death is the first step in reducing mortality rates. Similar studies have been conducted around the world and should continue regularly, as outcomes can differ across regions and years. By examining these differences, we can better address preventable and avoidable deaths. In this research, we looked at the most common causes of death among children in the PICU at Bandar Abbas Children's Hospital in 2023. The PICU mortality rate, which was about 60.4%, highlights the urgent need for focused interventions. We found that mortality was higher among girls, most common in children under one year of age, and more frequent during the colder months. Infections were the primary documented cause of death, followed by unspecified causes and neurological conditions.
Hashemian et al. (17) reported higher mortality in boys, with pneumonia, sepsis, liver failure, and malignancies as the leading causes. While our findings align regarding infections as the leading cause, they differ in gender-related mortality, with our study showing higher rates in girls. Another retrospective study in Kermanshah (18) found a mean age of 13 months, a higher mortality rate among boys, and respiratory diseases as the main causes. Our study contradicts these findings regarding gender and leading causes but aligns with the young age of most fatalities. Bilan et al. (19) found congenital heart disease, malignancies, and other congenital anomalies as the top causes of mortality over five years, with boys more affected than girls and the highest death rate in children under one year. This aligns with our findings concerning age but not gender or causes of death. In Nigeria, a five-month study reported 8.5% PICU mortality, higher among girls and children under one year (8), consistent with our results. In India, Patil and Godale (9) showed mortality higher in girls, with sepsis being a primary cause for those over one year, matching our findings. However, another Indian study reported higher mortality in boys, with similar causes to ours (4). A different Indian study by Deenadayalan (5) noted higher mortality in girls, with infections (sepsis, acute respiratory infections, and meningitis) and congenital heart disease as significant causes. They also reported a spike in summer deaths due to seasonal rains and snakebites, with most deaths occurring within the first 24 hours of admission, attributed to referral delays and delayed hospital interventions. Our study concurs on causes and gender but differs in seasonal mortality, with 24% of deaths occurring in the first 24 hours of admission.
Bohn et al. (6) noted pneumonia as a significant cause of mortality in Ethiopia. Variations in study type, hospital setting, and population demographics can explain differences in outcomes across regions. Still, pneumonia remains a critical cause of in-hospital mortality worldwide (20, 21). A study in China reported pneumonia, sepsis, and tumors as the leading causes, with higher mortality among girls, aligning with our results. They also noted that younger children were more susceptible to infectious diseases (7).
Daher et al. (22) reported a mean age of 24 months, with 52% being male. The mortality rate was 6.7%, with most deaths occurring in younger patients. Respiratory failure was the cause of death (34%), followed by cardiac diseases (20%) and gastrointestinal diseases (19%). Ayar et al. (23) reported a mortality rate of 18.06%, and found that age, gender, and length of stay did not show significant differences. Conditions such as hematologic diseases, immune deficiencies, and sepsis were prominent and associated with mortality. Al-Eyadhy et al. (24) reported a mortality rate of 4.4%, with the mean age 49.9 months. The most common causes of death were sepsis (30.7%), lower respiratory infections (18.8%), and cardiovascular causes (11.9%). Gundogdu et al. (25) reported a mortality rate of 13.4%, with 57.9% of patients being female. The mean PICU stay duration was 5.5 days. Bae et al. (26) found no significant differences in age or sex but noted a higher prevalence of gastrointestinal tract diseases. The PICU mortality rate was 11%, and the pathogen infection rate was 34% in the PICU. Hajidavalu and Sadeghizadeh (27) found that 56.9% of patients were male, with a mean age of 51.8 months. The leading causes for hospitalization were status epilepticus (12.9%) and pneumonia (11.6%), with a mortality rate of 12.2%. The average length of stay in the PICU was 10.8 days. Additionally, the length of stay in the hospital and PICU did not correlate with mortality rates. Seifu et al. (28) found that 54.6% of patients were male, with most staying in the PICU for 1 - 7 days. The mortality rate was 43.8%, with shorter stays having higher mortality odds.
Our study consistently found infections to be the top cause across all age groups. Given the role of infections as the leading documented medical diagnosis at the time of death at our center, highlighted by the significant mortality rate of 60.4%, epidemiological and interventional studies are necessary to improve diagnosis and treatment. It is important to note that in several cases, particularly among patients with underlying malignancies, the immediate cause of death was an acute infection (e.g., sepsis or pneumonia); however, the predisposing factor was the chronic condition itself. Immunosuppressive states induced by chemotherapy or the disease process inherently compromised the host's immune defense, thereby increasing susceptibility to severe infections. This underscores the complex interplay between chronic comorbidities and infectious mortality in pediatric intensive care settings, suggesting that addressing these conditions and reducing infection-related deaths could significantly lower mortality rates in this group.
The primary limitations of this study are its restriction to a single hospital and the inability to generalize its findings to other regions or populations. Our study lacked data on socioeconomic status and perinatal factors, which could have enriched the analysis of risk factors for pediatric hospital mortality. Furthermore, we did not explore the full impact of seasonal variations in depth. While our study noted some seasonal differences in mortality, the specific factors contributing to higher mortality in winter months (such as increased cases of infections related to seasonal changes, such as respiratory infections) were not fully examined. Moreover, due to the retrospective nature of the study and reliance on routine medical records, critical variables such as referral delays, pre-PICU stabilization efforts, and socioeconomic status were not available. Additionally, many critically ill patients were directly admitted to the PICU without prior stabilization, and emergency interventions were initiated after admission, which may have influenced the observed outcomes.
5.1. Conclusions
The mortality rate in the PICU was calculated to be approximately 60.4%, and the highest incidence of hospital mortality was observed in children admitted to the PICU at less than one year of age, with the most significant mortality rates occurring within the first one to seven days of PICU hospitalization. The most prevalent leading causes of death among these patients included infections, unknown etiologies, and neurological diseases. Additionally, the relative frequency of hospital mortality was higher in girls and occurred more frequently in the colder seasons.