1. Background
Inadvertent intraoperative hypothermia (IIH) is an unplanned and harmful drop in body temperature during surgery, distinguished from therapeutic hypothermia by a core body temperature below 36℃ (1). The IIH is associated with increased risks of adverse outcomes, including cardiovascular events, coagulopathy, delayed wound recovery, infection, immune suppression, and reduced drug metabolism, which can prolong postoperative recovery in pediatric patients (2). A previous study reported (3) that the incidence of intraoperative hypothermia ranges from 50% to 90%. Clinical guidelines for temperature management in surgical patients have been developed in recent years (4, 5). However, most studies have focused on adults, while pediatric-specific evidence remains relatively scarce and fragmented (1-6). Given the unique physiological characteristics of children — such as immature thermoregulatory control, a higher body surface area-to-mass ratio, limited glycogen reserves, and low subcutaneous fat — this population is at greater risk of IIH compared to adults (5, 7, 8). Moreover, regional factors such as the temperate and humid subtropical climate in Zhejiang, as well as differences in local perioperative temperature management practices, may also influence the incidence of IIH (9).
2. Objectives
This study aims to explore the characteristics and risk factors of IIH in pediatric patients, addressing existing gaps in pediatric-focused literature and providing a theoretical basis and clinical guidance for its prevention, with the goal of reducing IIH incidence in pediatric surgery.
3. Methods
3.1. Patient Selection
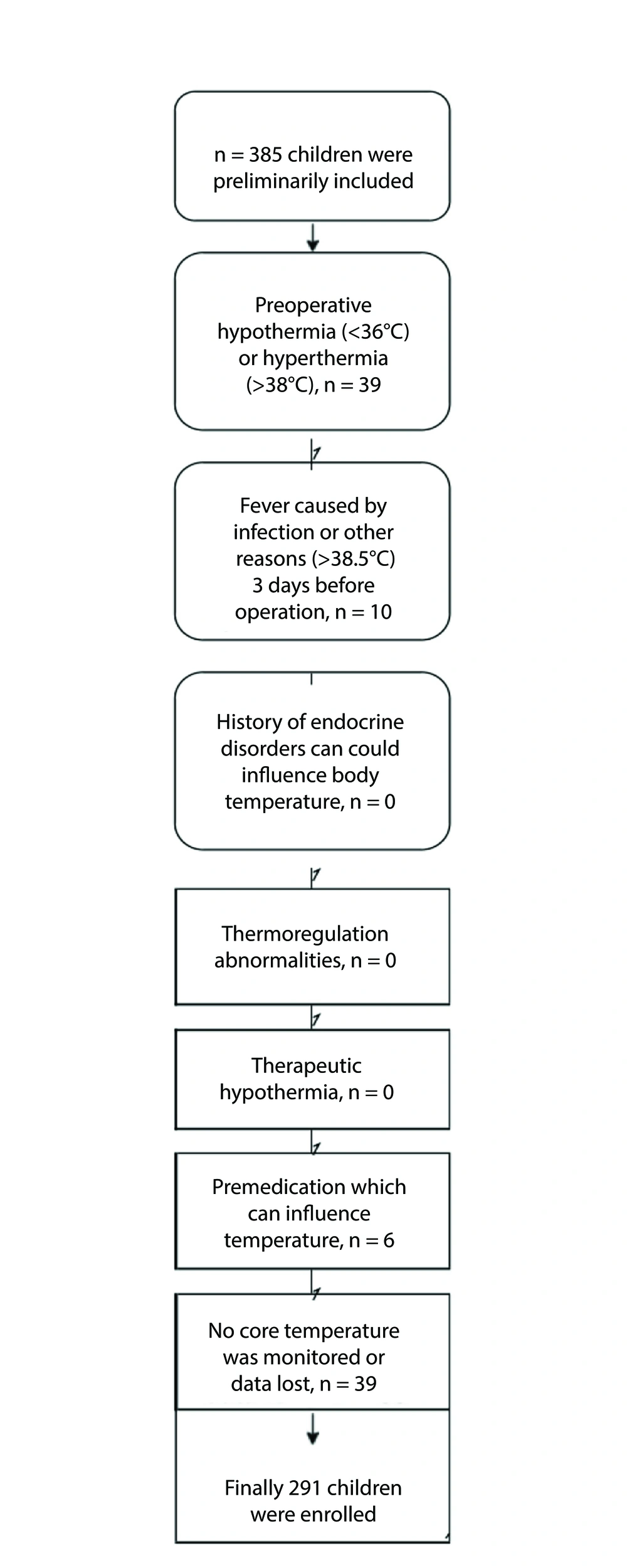
This retrospective study was conducted at the Children's Hospital, Zhejiang University School of Medicine, Hangzhou, China. The protocol was approved by the Ethics Committee (2019-IRBAL-136). Data from 291 pediatric patients who underwent surgery in our center between January and June 2020 were retrospectively analyzed. Inclusion criteria were: (1) Patients under 14 years old; (2) elective surgeries with continuous intraoperative temperature monitoring; (3) surgery duration > 2 hours; (4) preoperative tympanic temperature ≤ 37.5℃. Exclusion criteria were: (1) Patients with preoperative hyperthermia using physical methods or antipyretics for cooling; (2) patients using active intraoperative warming strategies without developing IIH; (3) cases requiring therapeutic hypothermia. The details of patient selection can be found in Figure 1.
3.2. Body Temperature Monitoring and Assessment
Nasopharyngeal temperature was measured as core temperature using an anesthetic monitor. Based on previously published studies, the optimal probe depth was adjusted according to the child’s age to ensure accurate placement (10). The core temperature was recorded by insertion of a nasopharyngeal probe (Philips Esophageal/Rectal Temperature Probe 25℃ - 45℃) after induction of anesthesia (11). The nasopharyngeal temperature was recorded every 15 minutes from the insertion of the probe to the end of the operation. Hypothermia was defined as a core temperature below 36℃. Patients were divided into the hypothermic group and the normothermic group. The degree of hypothermia was classified as mild (34 - 36℃), moderate (30 - 34℃), and severe (< 30℃) based on the American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (12). All patients were provided with both passive and active warming throughout their surgical procedures, with some receiving active prewarming. Active prewarming involved the use of a Forced-Air Warmer (Covidien LLC, USA) and a blanket, initiated prior to anesthesia induction and continued throughout the surgery based on the patient’s body temperature. Additionally, all patients were administered warmed infusion fluids, and forced-air warming was applied intermittently as needed during the operation. The operating room maintains a constant temperature of 24 - 26 degrees Celsius and a humidity level of 40 - 60% throughout the year. However, due to incomplete data recording, the exact temperature of the operating room during the operation was not identified. Additionally, the duration and frequency of the use of these active warming systems could not be found in the recording system.
3.3. Data Collection
Data were retrieved from the electronic anesthetic information system. Demographic data, including gender, birthdate, and weight [weight for age Z-score (WAZ), based on WHO Child Growth Standards 2006], were collected. Surgical data, including baseline body temperature, modes of anesthesia, American Society of Anesthesiologists (ASA) physical status, surgery levels (13), surgical positions, surgery types, date and duration of surgery, preoperative preparation duration, intraoperative blood loss, intraoperative fluid volume, hypothermic interventions, and vital signs (body temperature, heart rate, blood pressure, and blood oxygen saturation), were collected.
3.4. Statistical Analysis
Data were analyzed using SAS (version 9.2). Continuous variables are shown as mean ± standard deviation (SD) following a normal distribution and as median (P25, P75) otherwise. Categorical variables are summarized in frequency (n) and percentage (%). We compared the differences between hypothermic and normothermic groups using t-test, rank sum test, and chi-square test as appropriate. The following parameters were included in the model: Gender, age, WAZ, baseline body temperature, surgical positions, levels of surgery, types of surgery, modes of anesthesia, ASA, duration of surgery, duration of anesthesia, duration of preoperative preparation, intraoperative fluid volume, and intraoperative blood loss. LASSO regression was utilized in variable selection to control overfitting and collinearity. A logistic regression model was used to explore the risk factors of IIH. Subgroup analysis was conducted by age groups: Neonate and infant (0 - 1 year) and children (> 1 year). A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Demographic Data and Surgical Data
Table 1 summarizes the demographic and surgical characteristics of the 291 included participants, comprising 171 males and 120 females. The mean age was 5.02 (1.44, 26.52) months, including 54 neonates (within 28 days of birth), 122 infants (28 days - 1 year), 48 toddlers (1 - 3 years), 30 preschoolers (3 - 6 years), and 37 school-age children (over 6 years of age). In this study, 214 (73.53%) cases presented with IIH and were included in the hypothermic group. The remaining 67 cases constituted the normothermic group. Gender, age, WAZ, surgical positions, levels of surgery, types of surgery, and duration of preoperative preparation were compared between the two groups, and the results showed significant differences (P < 0.05). No significant differences were observed in baseline body temperature, modes of anesthesia, ASA, duration of surgery, duration of anesthesia, intraoperative fluid volume, and intraoperative blood loss (P > 0.05).
| Variables | Total (N = 291) | Normothermic Group (N = 77) | Hypothermic Group (N = 214) | P-Value |
|---|---|---|---|---|
| Gender | 0.013 | |||
| Male | 171 (58.76) | 36 (46.75) | 135 (63.08) | |
| Female | 120 (41.24) | 41 (53.25) | 79 (36.92) | |
| Age (mo) b | 5.02 (1.44, 26.52) | 9.48 (3.02, 49.80) | 3.56 (1.21, 14.20) | 0.003 |
| WAZ | -0.43 ± 2.16 | -0.17 ± 1.95 | -0.52 ± 2.23 | 0.232 |
| Baseline body temperature (℃, continuous) | 36.58 ± 0.38 | 36.63 ± 0.37 | 36.56 ± 0.38 | 0.142 |
| Baseline body temperature (℃, categories) | 0.398 | |||
| 36.4 < T ≤ 37.5 | 221 (75.95) | 62 (80.52) | 159 (74.30) | |
| 36 < T ≤ 36.4 | 44 (15.12) | 8 (10.39) | 36 (16.82) | |
| ≤ 36 | 26 (8.93) | 7 (9.09) | 19 (8.88) | |
| Surgical positions | 0.015 | |||
| Supine | 164 (56.36) | 38 (49.35) | 126 (58.88) | |
| Lateral position | 66 (22.68) | 14 (18.18) | 52 (24.30) | |
| Other positions | 61 (20.96) | 25 (32.47) | 36 (16.82) | |
| Levels of surgery | 0.307 | |||
| Level 4 surgery | 165 (56.70) | 39 (50.65) | 126 (58.88) | |
| Level 3 surgery | 86 (29.55) | 28 (36.36) | 58 (27.10) | |
| Level 2 surgery | 40 (13.75) | 10 (12.99) | 30 (14.02) | |
| Types of surgery | 0.050 | |||
| Open abdominal surgery | 122 (41.92) | 25 (32.47) | 97 (45.33) | |
| Laparoscopic surgery | 169 (58.08) | 52 (67.53) | 117 (54.67) | |
| Modes of anesthesia | 0.115 | |||
| General anesthesia | 237 (81.44) | 68 (88.31) | 169 (78.97) | |
| General anesthesia combined with sacral block | 26 (8.93) | 6 (7.79) | 20 (9.35) | |
| Nerve block | 28 (9.62) | 3 (3.90) | 25 (11.68) | |
| ASA | 0.604 | |||
| Ⅰ level | 110 (37.80) | 31 (40.26) | 79 (36.92) | |
| Ⅱ, Ⅲ level | 181 (62.20) | 46 (59.74) | 135 (63.08) | |
| Duration of surgery (min) | 124.75 ± 72.42 | 134.40 ± 79.50 | 121.28 ± 69.56 | 0.173 |
| Duration of anesthesia (min) | 174.84 ± 73.43 | 178.47 ± 80.08 | 173.53 ± 71.04 | 0.614 |
| Duration of preoperative preparation (min) | 47.24 ± 17.11 | 41.47 ± 17.98 | 49.31 ± 16.33 | 0.001 |
| Intraoperative fluid volume (mL) b | 200 (100, 500) | 300 (170, 500) | 200 (100, 450) | 0.065 |
| Intraoperative blood loss (mL) b | 10 (5, 15) | 10 (5, 20) | 5 (5, 10) | 0.242 |
Comparison of the General Condition of the Two Groups a
4.2. Characteristics of the Hypothermic Group
The degree of hypothermia was classified based on AHA guidelines for cardiopulmonary resuscitation. In the hypothermic group, 196 cases (91.59%) presented with mild hypothermia, 18 cases (8.41%) presented with moderate hypothermia, and no severe hypothermia occurred. The lowest body temperature recorded was 31.2℃. In pediatric surgical patients with hypothermia, intraoperative interventions were implemented in 128 cases (59.81%), while the remaining 86 cases (40.19%) did not receive active interventions. The median (P25, P75) lowest body temperature of the hypothermic group was 35.25 (34.70, 35.60)℃. The duration of hypothermia was 98.5 (50.0, 138.00) minutes. Heart rate, blood pressure, and percutaneous blood oxygen saturation during hypothermia were 120.93 ± 28.07 beats per minute, 78.75 ± 19.20/47.05 ± 12.83 mmHg, and 97.86 ± 2.87%, respectively (Table 2).
| Variables | Hypothermic Group (N = 214) |
|---|---|
| The degree of hypothermia | |
| Mild: 34 - 36℃ | 196 (91.59) |
| Moderate: 30 - 34℃ | 15 (7.01) |
| Severe: < 30℃ | 3 (1.40) |
| Active heating intervention | |
| No | 86 (40.19) |
| Yes | 128 (59.81) |
| Lowest body temperature (℃) b | 35.25 (34.70, 35.60) |
| The duration of hypothermia (min) b | 98.50 (50.00, 138.00) |
| Heart rate during hypothermia (beats/min) | 120.93 (28.07) |
| Systolic blood pressure during hypothermia (mmHg) | 78.75 (19.20) |
| Diastolic blood pressure during hypothermia (mmHg) | 47.05 (12.83) |
| Percutaneous oxygen saturation in hypothermia (%) | 97.86 (2.87) |
Characteristics of the Hypothermic Group a
4.3. Influencing Factors of Inadvertent Intraoperative Hypothermia in Neonates and Infants
After stratification by age, 176 cases of the hypothermic group were included in the neonate and infant group. After selection by LASSO, age and duration of preoperative preparation were included in the logistic model. The results showed that in neonates and infants, older age (OR = 0.88, 95% CI: 0.78 - 0.99, P = 0.031) was associated with a reduced risk of IIH, whereas longer preoperative preparation (OR = 1.03, 95% CI: 1.00 - 1.06, P = 0.050) was related to a higher risk of IIH (Table 3).
| Variables | OR (95% CI) | P-Value |
|---|---|---|
| Neonates and infants (n = 176) | ||
| Months | 0.88 (0.78, 0.99) | 0.032 |
| Duration of preoperative preparation (min) | 1.03 (1.00, 1.06) | 0.050 |
| Children (n = 115) | ||
| Gender | ||
| Female | 1.00 | - |
| Male | 7.06 (2.29, 26.57) | 0.001 |
| WAZ | 0.48 (0.27, 0.81) | 0.008 |
| Surgical position | ||
| Other positions | 1.00 | - |
| Lateral position | 5.94 (1.20, 33.02) | 0.033 |
| Supine | 5.53 (1.42, 24.11) | 0.017 |
| Levels of surgery | ||
| Level 2 surgery | 1.00 | - |
| Level 4 surgery | 12.15 (2.92, 64.14) | 0.001 |
| Types of surgery | ||
| Laparoscopic surgery | 1.00 | - |
| Other abdominal surgery | 5.71 (1.27, 36.21) | 0.037 |
Influencing Factors of Inadvertent Intraoperative Hypothermia in Neonates, Infants, and Children
4.4. Influencing Factors of Inadvertent Intraoperative Hypothermia in Children
The children group consisted of 115 pediatric surgical cases. The logistic regression model included the following parameters, which passed the LASSO selection: Gender, WAZ, baseline body temperature, surgical position, levels of surgery, types of surgery, modes of anesthesia, duration of surgery, duration of preoperative preparation, and intraoperative fluid volume. The results showed that in the children group, male children (OR = 7.06, 95% CI: 2.29 - 26.57, P = 0.001) and patients in supine (OR = 5.53, 95% CI: 1.42 - 24.11, P = 0.017) or lateral positions (OR = 5.94, 95% CI: 1.20 - 33.02, P = 0.033) were related to a higher risk of IIH. For different levels of surgery, level 4 surgery was more likely to induce IIH than level 2 surgery (OR = 12.15, 95% CI: 2.92 - 64.14, P = 0.001). Laparotomy was more likely to cause IIH than laparoscopy (OR = 5.71, 95% CI: 1.27 - 36.21, P = 0.037). The WAZ was a predictive factor for IIH in children (OR = 0.48, 95% CI: 0.27 - 0.81, P = 0.008) (Table 3).
5. Discussion
5.1. High Risk of Inadvertent Intraoperative Hypothermia in Pediatric Surgical Patients
With the development of comfortable medical treatment and enhanced recovery after surgery (ERAS), the issue of intraoperative temperature management in pediatric surgical patients has garnered more attention among medical workers. The IIH is a concern in pediatric surgery. A reliable and effective method to prevent hypothermia is still unclear, and the incidence of IIH remains high. Children have their own distinct anatomical and physiological characteristics and are not simply "mini versions" of adults. The overall incidence of IIH in pediatric surgical patients was 73.53% (214/291) in this study, which was slightly higher than the incidence (60 - 63.6%) reported by Motta et al. (14) and Shen et al. (15). Recent studies further contextualize these findings. For instance, a recent study from Ethiopia reported a 44.7% incidence of IIH in pediatric patients under general anesthesia, highlighting regional variations in healthcare practices (16). This may be related to the fact that only pediatric cases with continuous intraoperative temperature monitoring were included in the study, potentially selecting patients at higher risk for IIH based on clinical judgment. Most hypothermic cases (91.59%) in this study were mild (34 - 36℃) (17), which aligned with the results of a previous study (18). In recent years, increased attention to IIH prevention and the implementation of intraoperative measures have helped mitigate temperature drops during surgery (19).
In this study, hypothermia still occurred in 128 cases despite active interventions, accounting for 59.81% of the hypothermic group, which was higher than the results shown in a previous study (20). The incidence of perioperative hypothermia in adult surgery with active warming interventions was still 29.4%, indicating that IIH cannot be completely avoided despite active interventions in both adult and pediatric surgeries under the influence of multiple factors. Therefore, it is important for medical workers to evaluate the risk of IIH and monitor intraoperative body temperature in pediatric surgical patients. Identifying effective methods to maintain body temperature is also a focus in pediatric surgery. The risk assessment of IIH in pediatric surgical patients and standard interventions require further investigation.
5.2. Different Age-Related Risk Factors for Inadvertent Intraoperative Hypothermia in Pediatric Surgical Patients
A review (21) found that factors contributing to IIH in adults included low BMI, low height, low body weight, older age, low body temperature at the time of transferring to the operating table, low systolic pressure, low heart rate, long anesthesia duration, and more blood loss. Children are in a stage of rapid growth and development, with functions of vital organs and tissues gradually improving. Children of different ages show varied degrees of maturation, and individual differences are also large. This study found that pediatric surgical patients in different age groups have different risk factors of IIH. Medical workers should be familiar with the features of children’s growth and development at different stages, knowing the characteristics and influencing factors of IIH in children of different ages, accurately assessing and identifying pediatric surgical patients at high risk, thus implementing individualized medical care and interventions against IIH.
5.3. Risk Factors of Inadvertent Intraoperative Hypothermia in the Neonate and Infant Group
5.3.1. Higher Risk of Inadvertent Intraoperative Hypothermia in Younger Patients (by Age in Months)
Our results reveal that pediatric surgical patients with younger ages in months were at higher risk of IIH. A recent study by Zhao (20) reported an incidence of IIH of 82.83% in neonates and 38.31% in infants, highlighting the heightened vulnerability of younger pediatric patients to hypothermia. This aligns with our observation on age in the neonate and infant group. The functions of tissues and organs are immature in infants of younger age, especially in neonates. An immature central neural thermoregulation system, weak body temperature regulation, and a thin subcutaneous fat layer make children’s body temperature more susceptible to ambient changes (22). An ambient operating temperature of 21 - 25℃ is relatively low for children, requiring more preoperative preparations. Younger children have a higher body surface to mass ratio, about twice that of adults, and thus heat is more easily lost through the mechanisms of radiation, conduction, convection, and evaporation.
Infants under 1 year old lack the thermogenesis of subcutaneous brown fat and the ability to increase thermogenesis by shivering, and preoperative fasting deprives the body of glycogen reserves. Due to the anesthetic-induced inhibition of vasoconstriction and the weak vasomotor control in infants, a core-to-peripheral redistribution of heat occurs, leading to a decrease in core temperature. This is consistent with the findings of a previous study (7). Medical workers should be aware of the importance of temperature management in neonates and infants, especially those with younger ages in months, and consider intraoperative body temperature monitoring as a routine.
5.3.2. Higher Risk of Inadvertent Intraoperative Hypothermia in Patients with Longer Duration of Preoperative Preparation
Preoperative preparation is essential for surgery. Adequate preparation ensures smooth operation and the safety of children. Routine preparation includes anesthesia procedures, nursing procedures, surgical positioning, and skin disinfection of the surgical field. Previous research (18) showed that the core temperature of infants and young children decreased by 1 - 2℃ during the first hour of general anesthesia, and the results of this study are consistent with that.
Anesthetics induce a core-to-peripheral redistribution of heat, where 75% of the heat is lost through radiation, convection, conduction, and evaporation. The first and second phases of the redistribution process fall within the period of preoperative preparation, which is associated with the following reasons: Preoperative preparation requires exposure of the patient's body; procedures including disinfection will take away body heat, especially in infants who have a relatively large skin surface ratio; blood vessels in infants under 1 year old are small, making artery puncture difficult, thus prolonging the duration of preoperative preparation.
Actionable interventions to mitigate this risk include streamlining preoperative processes to minimize preparation time, using experienced anesthesiologists and nurses to enhance efficiency, and employing prewarming techniques (e.g., forced-air warming blankets or warmed mattresses) before anesthesia induction. Maintaining an operating room temperature above 25℃ and using warmed disinfectants can further reduce heat loss, especially in younger patients with higher body surface-to-mass ratios.
5.4. Risk Factors of Inadvertent Intraoperative Hypothermia in the Children Group
5.4.1. Higher Risk of Inadvertent Intraoperative Hypothermia in Male Children
In the children group of this study, 63.08% of the cases with IIH were male, with a statistically significant difference in gender. However, this association should be interpreted cautiously, as it may be influenced by confounding factors such as surgery type and duration. For instance, male patients in our cohort were more likely to undergo laparotomy, which is associated with a higher risk of IIH due to prolonged exposure of body cavities and greater intraoperative heat loss. Additionally, the duration of surgery, although not significantly different between groups, may contribute to this association, as longer procedures could exacerbate heat loss in male patients undergoing more complex surgeries.
A meta-analysis by Campbell et al. (23) found that gender was not independently associated with IIH, suggesting that our observed gender difference may not reflect a direct mechanistic link but rather an interplay of surgical and patient-related factors. Limited mechanistic explanations, such as slight differences in basal body temperature or thermoregulation thresholds (24), do not fully account for this finding. Further studies with larger sample sizes and detailed stratification by surgery type and duration are needed to clarify whether gender independently contributes to IIH risk in pediatric patients.
5.4.2. Increased Inadvertent Intraoperative Hypothermia Risk in Supine and Lateral Surgical Positions
Supine and lateral positions are the most commonly used surgical positions. In the children group of this study, 178 cases (83.18%) adopted these two positions. Macario and Dexter (25) developed a Risk Factors Evaluation Index System consisting of 23 indexes for perioperative hypothermia via the Delphi method and hierarchy analysis, which found that surgical position was a risk factor for IIH. Our study, consistent with the former study, showed that supine and lateral positions were associated with a higher incidence of IIH. About 85% of body heat is lost through the skin by radiation and convection. Children are characterized by a "big head, short legs, and large proportion of torso" in body shape. The proportion of exposed skin area, i.e., the heat dissipation area, is therefore larger when children adopt supine and lateral surgical positions.
The conclusion may be affected by data bias, since the number of cases in supine and lateral surgical positions in this study was significantly larger than that of other positions. Studies with larger samples are required to further verify this conclusion.
5.4.3. Higher Inadvertent Intraoperative Hypothermia Risk Associated with Higher Levels of Surgery
In this study, the incidence of IIH in level 4 surgery was 58.88%, significantly higher than that in other levels of surgery. Table 3 shows an increased incidence of IIH with higher levels of surgery. According to the surgery management documentation of China (2011), level 4 surgery is defined as surgery with high technical complexity, a complicated operating process, and a high risk of complications. Yi et al. (26) established a prediction equation to estimate the risk of intraoperative hypothermia in adults, which was recommended by the China guideline for perioperative hypothermia. Previous research showed that the incidence of IIH increased significantly when the duration of surgery exceeded 2 hours (8). Intravenous infusion of 1000 mL of fluid at room temperature or 1 unit of blood lowers the body temperature by 0.25 - 0.5℃. The use of more than 1000 mL of irrigation fluid without warming will increase the risk of IIH. Level 4 surgery is usually accompanied by longer duration, more blood loss, and more fluid volume due to surgical complexity.
Experienced surgeons are recommended for level 4 surgeries to ensure smooth operation and reduce intraoperative blood loss, thus decreasing the risk of IIH in pediatric surgical patients.
5.4.4. Higher Risk of Inadvertent Intraoperative Hypothermia in Children Undergoing Laparotomy
This study showed that laparotomy was more likely to cause IIH than laparoscopy in pediatric surgical patients (P < 0.05), which conforms to the results of Giuliano and Hendricks (27). Kim et al. (28) also suggested that the types of surgery, especially laparotomy, were a main cause of perioperative hypothermia in infants. Multiple factors contribute to hypothermia in open abdominal surgery, including an open surgical site, exposure of organs, fluid irrigation, usage of wet gauze to stop bleeding, and long duration of surgery.
Children scheduled for laparotomy should be considered key patients for temperature management. Comprehensive preoperative evaluations should include individual features and the type of surgery. Specific insulation methods should be adopted to reduce the incidence of IIH: Reduce unnecessary skin exposure during pediatric surgery; warming of intravenous fluids, irrigation fluids, and skin disinfectant is suggested; and a well-coordinated surgical team is preferred to shorten the exposure time of body cavities and organs. In addition, active warming for abdominal surgeries and reducing preoperative preparation time are also critical in laparotomy surgery to avoid IIH.
5.5. Conclusions
This study identified age, low WAZ, preoperative preparation duration, surgical position, surgical level, and surgery type as significant risk factors for IIH in pediatric surgery. The observed association with male gender (P = 0.013) should be interpreted cautiously, as it may be confounded by factors such as surgery type (e.g., laparotomy) and duration, which are known to increase IIH risk. Risk factors varied between neonates, infants, and older children, highlighting the need for age-specific interventions to reduce IIH incidence. Larger, high-quality studies with robust adjustment for confounders are needed to further elucidate the role of gender and other risk factors in IIH among pediatric patients. Developing a comprehensive risk assessment system will provide a stronger theoretical basis for intraoperative temperature management in pediatric surgery.
5.6. Limitations
This study has several limitations. First, the study included only pediatric patients with continuous intraoperative temperature monitoring, which may introduce selection bias, as these patients might have been identified as higher risk for IIH based on clinical judgment. Second, the study was conducted at a single center in Zhejiang province, China, which may limit the generalizability of the findings to other populations or healthcare settings with different surgical practices, environmental conditions, or patient demographics. Third, the sample size may have been insufficient to detect smaller effect sizes or less prevalent risk factors, potentially reducing the statistical power for some comparisons. Fourth, while we included multiple potential influencing factors in our analyses, unmeasured confounding factors, such as ambient operating room temperature and variations in intraoperative warming techniques, could have influenced the incidence of IIH. Finally, the study did not assess long-term clinical outcomes associated with IIH, such as postoperative complications or recovery time, which limits our understanding of the clinical impact of hypothermia in this population. Future prospective, multicenter studies with larger sample sizes and comprehensive data collection are needed to address these limitations and further elucidate the risk factors and consequences of IIH in pediatric surgery.