1. Background
Acute pancreatitis (AP) is an acute abdominal condition characterized by the abnormal activation of pancreatic enzymes, leading to digestive damage to the pancreas and neighboring organs, with local pancreatic inflammation as a prominent feature. In severe cases, it can result in organ dysfunction (1). With a rising incidence, AP has emerged as an increasingly significant health issue among children. Approximately 3 - 13 cases are reported annually per 100,000 children, and about 25% of pediatric AP cases develop severe complications, with an overall mortality rate of approximately 4% (2, 3). While diagnostic and evaluation systems for adult AP are relatively well-established, systematic studies on pediatric AP remain limited (4, 5). The clinical manifestations and disease progression of pediatric AP differ significantly from those of adults, posing challenges for early diagnosis and timely treatment. These challenges hinder the likelihood of children receiving prompt and effective care. Therefore, it is necessary to conduct in-depth research on children’s AP.
2. Objectives
The present study aims to conduct an in‐depth analysis of the clinical characteristics and prognosis of pediatric AP caused by various etiologies. Such efforts to identify clinically significant features are expected to enhance clinicians’ understanding and management of pediatric AP.
3. Methods
3.1. General Information
The present study was a retrospective cohort one. Based on the incidence reported in previous literature, statistical software was used to apply the formula:
Calculate the required sample size. A total of 102 pediatric patients aged 4 - 15 years diagnosed with AP and admitted to Baoding Hospital, Beijing Children’s Hospital affiliated with Capital Medical University from January 2023 to December 2024 were selected as study subjects by continuous sampling. The study was approved by the Institutional Ethics Committee of Baoding First Central Hospital (No.: 2024081; date: December 30, 2024), and written informed consent was obtained from all guardians of the children.
The inclusion criteria included: (1) Diagnosed with AP based on the revised Atlanta criteria (6), meeting at least two of the following three criteria: (A) Typical clinical symptoms: Acute onset of upper abdominal pain, often radiating to the back; (B) imaging examination [ultrasound, abdominal CT, and magnetic resonance cholangiopancreatography (MRCP)] showed features of pancreatic inflammation, such as pancreatic enlargement and peripancreatic effusion; (C) serum amylase (AMY) and/or lipase (LPS) levels exceeding three times the upper limit of normal and; (2) complete clinical case records.
The exclusion criteria were: (1) Chronic pancreatitis, (2) aged over 18 years at the time of AP diagnosis, (3) hospital stay for less than 72 hours or those who discontinued treatment.
3.2. Classification of Acute Pancreatitis
Based on the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) management and grading standards (7), AP was classified as mild acute pancreatitis (MAP), moderately severe acute pancreatitis (MSAP), and severe acute pancreatitis (SAP).
- Mild acute pancreatitis: No organ dysfunction, no local or systemic complications, and no exacerbation of chronic comorbidities (e.g., chronic kidney disease, chronic pulmonary diseases).
- Moderately severe acute pancreatitis: Organ dysfunction lasting ≤ 48 hours, or the presence of local/systemic complications, or exacerbation of chronic comorbidities.
- Severe acute pancreatitis: Persistent organ dysfunction lasting > 48 hours.
3.3. Study Parameters
(1) General characteristics: Age, sex, and length of hospital stay.
(2) Etiology: Biliary, anatomical abnormality-related, idiopathic, drug-induced, and traumatic.
(3) Clinical symptoms: Abdominal pain, vomiting, fever, abdominal distension, diarrhea.
(4) Imaging methods: Ultrasound, abdominal CT, and MRCP. Ultrasound was performed using a high-end color Doppler ultrasound machine (model: ACUSON Sequoia of Siemens). Abdominal CT was performed using a multi-slice spiral CT (model: Siemens SOMATOM Force). The MRCP examination was performed using a high-field magnetic resonance imager [model: Siemens MAGNETOM Skyra (3.0T)].
(5) Laboratory parameters (includes range of normal values): Data collected within 24 hours of admission, including LPS (13 - 60 U/L), AMY (30 - 110 U/L), white blood cell count (WBC, 5.0 - 15.0 × 109/L), hematocrit (HCT, 33 - 39%), C-reactive protein [(CRP), < 10 mg/L], blood glucose [(GLU), 3.9 - 6.1 mmol/L], blood calcium [(Ca), 2.2 - 2.6 mmol/L], and imaging findings.
(6) Complications: Pancreatic pseudocyst, respiratory dysfunction, pancreatic necrosis, circulatory dysfunction, peripancreatic fluid collection, and renal dysfunction.
3.4. Statistical Methods
Data were analyzed using SPSS 22.0 statistical software. Measurement data were expressed as mean ± standard deviation (x̄ ± s), and comparisons between groups were conducted using the t-test. Categorical data were expressed as frequencies and percentages [n (%)], and comparisons were made using the χ2 test. A P-value of < 0.05 was considered statistically significant. Measurement data following a skewed distribution were expressed as the median and interquartile [M (P25, P75)]. Multiple group comparisons were performed using the Kruskal‐Wallis H test, and pairwise comparisons between groups were conducted using the Bonferroni correction.
4. Results
4.1. General Clinical Data
From January 2023 to December 2024, 102 pediatric AP cases were admitted to our hospital. Among these, 53 were male and 49 were female. The average age of onset was 9.5 ± 5.4 years, distributed as follows: Infants (11%), preschool-aged children (22%), school-aged children (28%), and adolescents (38%). The length of hospital stay ranged from 4 to 79 days, with an average duration of 15.5 ± 12.2 days.
4.2. Etiology and Severity Assessment
The etiological distribution of the 102 AP cases was as follows: (1) Twenty-four cases of biliary AP (23.5%), (2) 16 cases of anatomical abnormality-related AP (15.7%), (3) 29 cases of idiopathic AP (28.4%), (4) 7 cases of drug-induced AP (6.9%), 26 cases of traumatic AP (25.5%).
The severity distribution of AP cases was 61.8% MAP, 21% MSAP, and 11% SAP. Details of the severity distribution by etiology are shown in Table 1.
4.3. Clinical Symptoms and Imaging Analysis
Among the 102 pediatric AP cases, the most common clinical symptom was abdominal pain, present in 87.3% (89/102) of all cases. Other symptoms included vomiting (59.8%, 61/102), fever (36.3%, 37/102), abdominal distension (13.7%, 14/102), diarrhea (6.9%, 7/102), and others (12.7%, 13/102). Imaging modalities used included ultrasound, abdominal CT, and MRCP. Ultrasound examination was performed in 88.2% (90/102) of cases, with a positivity rate of 74.4% (67/90). Abdominal CT was performed in 98.0% (100/102) of cases, with a positivity rate of 85% (85/100). The MRCP was performed in 55.9% (57/102) of cases, with a positivity rate of 91.2% (52/57).
4.4. Key Laboratory Parameter Analysis
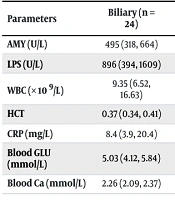
Significant differences were observed in WBC, CRP, GLU, and Ca levels among AP cases of different etiologies (P < 0.05, respectively). The results of the analysis of key laboratory parameters by etiology are shown in Table 2.
| Parameters | Biliary (n = 24) | Anatomical Abnormality‐Related (n = 16) | Idiopathic (n = 29) | Drug‐Induced (n = 7) | Traumatic (n = 26) | H‐Value | P‐Value |
|---|---|---|---|---|---|---|---|
| AMY (U/L) | 495 (318, 664) | 339 (268, 759) | 367 (258, 693) | 362 (225, 594) | 581 (282, 953) | 3.596 | 0.463 |
| LPS (U/L) | 896 (394, 1609) | 656 (249, 1690) | 646 (362, 1342) | 851 (447, 1322) | 1197 (374, 1829) | 2.465 | 0.651 |
| WBC (× 109/L) | 9.35 (6.52, 16.63) | 9.10 (4.94, 12.24) | 15.29 (8.16, 20.44) | 1.65 (0.42, 7.22) | 11.18 (7.24, 15.11) | 21.857 | < 0.001 |
| HCT | 0.37 (0.34, 0.41) | 0.36 (0.34, 0.37) | 0.38 (0.32, 0.43) | 0.34 (0.27, 0.39) | 0.31 (0.25, 0.40) | 8.513 | 0.074 |
| CRP (mg/L) | 8.4 (3.9, 20.4) | 21.6 (3.3,56.4) | 28.9 (6.0, 229.0) | 24.4 (5.2, 55.3) | 35.2 (18.3, 74.4) | 15.371 | 0.004 |
| Blood GLU (mmol/L) | 5.03 (4.12, 5.84) | 4.75 (3.46, 5.45) | 5.46 (4.95, 6.18) | 3.89 (3.10,7.11) | 4.51 (3.94, 5.14) | 18.146 | 0.001 |
| Blood Ca (mmol/L) | 2.26 (2.09, 2.37) | 2.32 (2.26, 2.40) | 2.33 (2.20, 2.39) | 2.14 (2.00, 2.29) | 2.19 (2.11, 2.36) | 15.283 | 0.004 |
Analysis of Key Laboratory Parameters in Pediatric Acute Pancreatitis by Etiology a
4.5. Analysis of Complications by Severity
Among 28 cases of MSAP, the most common complication was pancreatic pseudocyst (32.1%, 9/28). For the 11 cases of SAP, the primary complication was respiratory dysfunction (54.5%, 6/11). The analysis of complications by severity is shown in Table 3.
| Complications | MAP (n = 63) | MSAP (n = 28) | SAP (n = 11) |
|---|---|---|---|
| Pancreatic pseudocyst | 0 | 9 (32.1) | 1 (9.1) |
| Respiratory dysfunction | 0 | 6 (21.4) | 6 (54.5) |
| Pancreatic necrosis | 0 | 4 (14.3) | 1 (9.1) |
| Circulatory dysfunction | 0 | 6 (21.4) | 1 (9.1) |
| Peripancreatic fluid collection | 0 | 3 (10.7) | 0 (0) |
| Renal dysfunction | 0 | 0 (0) | 2 (18.2) |
Analysis of Complications by Severity in Pediatric Acute Pancreatitis a
4.6. Treatment and Prognosis Analysis
In accordance with the treatment principles for AP, systemic treatments were administered, including fasting, fluid resuscitation, acid suppression, continuous gastrointestinal decompression, and intravenous fluid therapy. For patients unable to consume food within 4 - 5 days, specialized nutritional support was provided. The rate of intravenous fluid therapy was 98.0% (100/102). Enteral nutrition was administered either orally or via a nasogastric tube, with nasogastric tube treatment used in 70.6% (72/102) of cases. The initiation of nasogastric tube feeding occurred at a mean of 5.49 ± 1.80 days and lasted for 10.46 ± 5.26 days. Following systematic and scientific treatments, including fasting, intravenous injection, and enteral nutrition, 101 (99.0%) patients either showed improvement or were discharged after recovery. One child (1.0%) with acute leukemia complicated by organ failure was transferred to another hospital at the family’s request. Overall, treatment outcomes were favorable.
5. Discussion
Reports indicate that the incidence of AP in children is increasing globally (8, 9). Pediatric AP differs significantly from adult AP in terms of etiology, laboratory findings, and prognosis. Therefore, it is inappropriate to fully adopt adult standards for diagnosis and treatment (10). In China, there is limited research on the etiology of pediatric AP, and no unified diagnostic and treatment guidelines are available. Consequently, managing AP in children remains challenging due to the lack of standardized protocols.
The present study analyzed the etiology, severity, clinical symptoms, laboratory parameters, complications, treatment approaches, and prognosis of pediatric AP cases. The incidence and etiology of pediatric AP vary significantly across geographical regions. In Western countries, systemic diseases and drug-induced pancreatitis are the predominant causes, whereas in Asia, biliary disease and idiopathic factors are more commonly implicated in pediatric AP (9, 11). Among the 102 children with AP in this study, the leading etiologies were categorized as idiopathic, biliary, anatomical abnormality-related, drug-induced, and traumatic, aligning with findings from domestic and international research (11). Metabolic, infectious, vascular, and hereditary pancreatitis are rare in children, so no significant cases were found in this study. This is consistent with the epidemiological characteristics of AP in children and is also related to the limitations of the small sample size of this study.
In terms of severity, the majority of pediatric AP cases were classified as MAP, accounting for 61.8%, followed by MSAP at 21.0%, and SAP at 11.0%. Zhong et al. reported the clinical characteristics and prognosis of AP in children and found that most cases were MAP, accounting for more than 60%, and MSAP and SAP accounted for about 20% and 10%, respectively, which was roughly consistent with the conclusions of our study (11). This distribution underscores the predominance of mild cases in pediatric AP.
The study results indicate that the primary clinical symptoms of pediatric AP were abdominal pain, vomiting, and fever. When children present with unexplained vomiting and abdominal pain, the possibility of AP should be considered. Currently, abdominal CT is widely regarded as the gold standard for diagnosing AP both domestically and internationally (12). In this study, abdominal CT had the highest completion rate at 98.0% and a relatively high positive rate of 85%. Ultrasonography, which is cost-effective, simple to perform, and free of radiation exposure, had a completion rate of 88.2%, second only to CT. However, the positive rate of ultrasonography was slightly lower compared with CT. Although ultrasound is non-invasive and radiation-free, its results are highly influenced by factors such as the skill level of the operator and the size of the child, so in some cases, CT and MRI are more reliable. This is consistent with the views of Yang et al. (13). The MRCP demonstrates high sensitivity for detecting congenital pancreatic anomalies and biliary diseases but is less commonly used in routine examinations due to its higher cost and the need for greater patient cooperation (14). All three diagnostic methods offer significant reference value for the confirmation of AP in children.
Significant differences were observed in the levels of WBC, CRP, GLU, and Ca among children with AP caused by different etiologies (P < 0.05, respectively). These laboratory parameters can be used to analyze the underlying causes of AP. White blood cell count and CRP are two critical inflammatory markers (15). Reportedly, AMY and LPS are important laboratory markers for screening AP. C-reactive protein is a key factor for evaluating the prognosis and predicting the progression of AP to SAP in pediatric patients (16). In contrast, LPS, another vital marker for assessing the severity of AP (17), did not show statistically significant differences across pediatric AP cases of different etiologies.
Among the 28 children with MSAP, pancreatic pseudocysts were the most common complication, whereas respiratory dysfunction was the primary complication in 54.5% of SAP cases. Intravenous fluid therapy was administered in 98.0% of cases, and nasogastric tube feeding was used in 70.6%, with an average initiation time of 5.49 ± 1.80 days and a duration of 10.46 ± 5.26 days. Current studies indicate that enteral nutrition can reduce the risks of secondary infections and malnutrition in AP patients (18, 19). The complete response rate in this study was 99.0%, demonstrating excellent treatment outcomes for pediatric patients.
5.1. Conclusions
This study provided useful information about the characteristics and outcomes of pancreatitis in children, showing that the most common clinical symptom was abdominal pain, the most common cause was idiopathic, most cases were mild, and the outcomes were satisfactory.
5.2. Limitations
There are still some shortcomings in this study. This study focuses on the clinical symptoms and treatment outcomes of AP in children with different etiologies. However, there is a lack of analysis regarding the differences in related parameters between the initial onset and recurrence of AP, as well as the interference caused by comorbidities. To ensure the comprehensiveness and depth of research, it is essential to conduct more extensive follow-up studies to address the limitations of this short-term investigation.