Fulltext
Sacrococygeal teratomas are the most common teratomas, while head and neck cases are extremely rare[1,2]. The approximately reported incidence of teratoma is 1 in 35000 to 40000 live-births[3,4]. Although they are generally more common in females, no gender preference is reported in head and neck ones[2].
It is thought that teratoma originates from those multi-potential germinal cells which are lost during a migration from yolk sac endodermal layer adjacent to allantois to gonadal edge in fourth and fifth gestational week[5]. The mentioned cells then can be arisen as teratoma somewhere from brain to coccyx, often in the midline[1,5,6].
A full-term female infant, gestational age of 40 weeks, was born via cesarian section to a 24 year old primigravida. The mother had history of hypertension and limb edema at 36th week of pregnancy in which abdomino-pelvic ultrasound examination revealed a fetus facial mass and congenital heart anomaly in addition to polyhydramnios. The infant's birth weight was 3530g and the Apgar scores were nine and ten at 1 and 5 minutes respectively. Evaluation of the infant in nursery room revealed a mid-facial mass in shape of beak protruding about 10 cm with a base extending to forehead at the top and to palate at the bottom where it made nasal trills to deviate aside (Fig. 1). She was then referred to our hospital regarding her congenital heart anomaly and mild respiratory distress. On admission, she was in a subtle respiratory distress for which the diagnosis of an upper

Fig. 1: Infant with nasal teratoma
respiratory tract obstruction due to mass was made. Subsequently fixation of the mass not only relieved the respiratory distress, it also surprisingly made her free of supplemental oxygen.
Further examination of the mass with Ultrasound and MRI showed a mass with homogenous hyper-echogenecity (density resembling fat tissue) all over except in central part in which cystic areas with different echogenecity and hypo-echogenecity (most presumably bony structure) were detected. MRI scan by a 1.5T device showed a large soft tissue mass in anterior part of the face in midline originating in ethmoid sinuses and posterior aspect of the nasal fossa with a midline defect in palate, mostly showing T1 T2 high signal in favor of fat with tubular T1 T2 low signal region which could be due to bone and also a small central cystic component (Fig. 2). No definite connection with the meninges or brain was noted.
Severe tricuspid atresia, atrial septal defect,
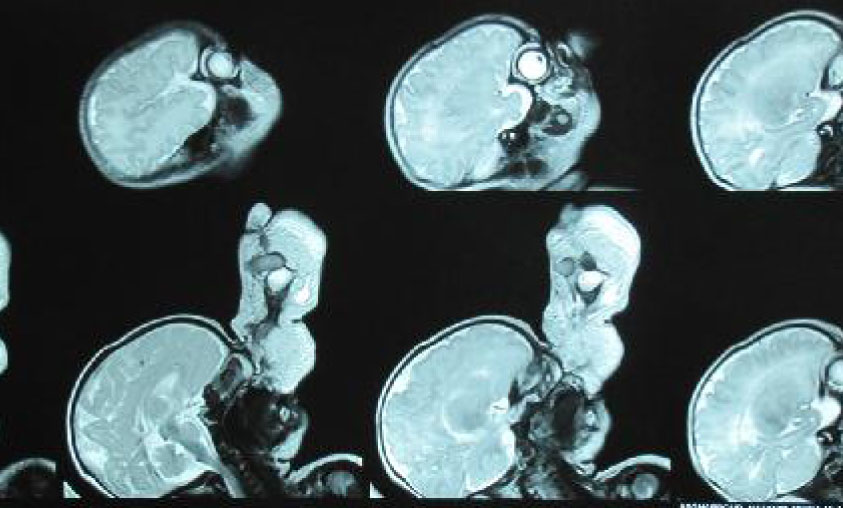
Fig. 2: Infant MRI (highsignal fat component with central cystic part)
ventricular septal defect and pulmonary stenosis were detected during Echocardiographic assessment.
After essential evaluation and preparation, the patient underwent surgery and a large mid-facial protrusion was resected. Pathology reported neoplastic tissue consisting of heterologous elements such as skin and its appendages, glandular structure, cartilage, marrow elements and bone with no evidence of neuroepithelial elements compatible with mature teratoma.
Nasal masses could be due to glioma, meningoencephalocele, encephalocele, conge-nital rabdomyosarcoma, and lymphatic malfor-mations[5,6]. Tumor arising from hard and soft palate and Rathke’s pouch are called epignathus teratomas.
Sometimes a fetus bearing teratoma is unable to swallow amniotic fluid due to its mass effect, thus polyhydramnios may be detected at about 15% of pregnant women[1].
The main treatment of teratoma is Surgery. The overall long term prognosis is excellent and relapses take place rarely. Despite benign nature of teratomas, routine follow-up is necessary in all cases[5]. In our patient in 1 year follow-up, no recurrence occurred and alfa fetoprotein (AFP) levels reduced after tumor resection.