Fulltext
Lipoma is a benign neoplasm of adipose tissue. In children it rarely rises in mesentery or gastrointestinal tract and the secondary midgut volvulus caused by lipoma is very rare[1,2].Herein, we report a 6-year-old girl with small bowel lipoma causing midgut volvulus.
The patient presented to emergency ward with a 2-day history of moderate central abdominal pain, colicky in nature accompanied with nausea and vomiting. No mass was touched on palpation. Routine blood tests showed normal white cell count, urea, creatinine, amylase and electrolytes. Plain abdominal X-ray showed a gasless pelvis and lower abdomen, but laterally deviated and dilated intestinal loops. Abdominal ultrasonography revealed a loose ill-defined lobulated mass quite isoechoic with mesenteric fat in right lower abdomen displacing the echogenic small bowel loops gas. Computed tomography revealed a well-capsulated, homogeneous mass with negative HU about lipid density, 13×3×5 cm in size, filling the right portion of the inferior abdomen and pelvis, deviating the intestinal loops (Fig. 1). Volvulus of midgut by twisted (about 360° clockwise) appearance of the main mesenteric vessels in their root was depicted (Fig. 2). The diagnosis of volvulus was confirmed in color Doppler ultrasonography, where superior mesenteric vein was observed to lie in the left side of superior mesenteric artery. At laparotomy, after detorsion, a mesenteric lipoma was identified in
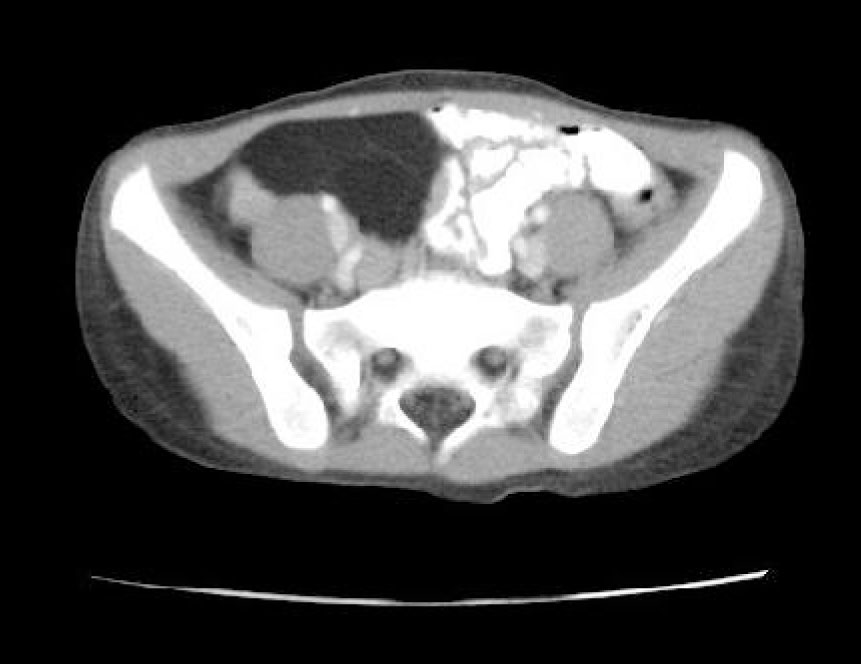
Fig. 1: Contrast enhanced CT scan showing a mass with lipid density filling the right portion of the inferior abdomen and pelvis, deviating the intestinal loops
the terminal ileum approximately 15 cm proximal to the ileocecal valve. Macroscopically a yellowish encapsulated, homogeneous mass measuring approximately 13×3×5 cm was revealed (Fig. 3).
Microscopically, the tumor was composed of a fibrous capsule and mature fat cells next to the intestinal wall. After the surgery all abdominal symptoms were alleviated and the patient remained symptom free for the next 8 months in follow up.
Lipomas are benign mesenchymal tumors, resembling normal fat with very low potential for malignant degeneration. They have been reported in children of all ages with no specific predilection[2,3]. In gastrointestinal tract lipomas mostly present as an insidious-growing, soft and mobile mass without penetration into surroundings[2,3]. Very infrequently they lead to intermittent abdominal pain, distension, small intestine volvulus, and constipation[1,2].
X-ray imaging reveals a well-demarcated, radiolucent area along with the intestinal obstruction, while ultrasonography and CT display more reliable information about the lipid basis of the tumor[1,3].
According to the CT findings, other fat attenuation processes associated with the mesentery are considered as differential diagnosis, including liposarcoma, lipoblastoma, lymphangiomas, and the cavitating, mesenteric lymph node syndrome. Mesenteric lipomas are encircled with a uniform matrix. Liposarcomas usually have a mixed heterogenous fat and soft tissue structure[4]. Lipoblastoma is a benign tumor of embryonal fat cells and its nonhomogeneous, septated, and hyperechogenic appearance on ultrasonography and CT makes it easy to differentiate from a lipoma[4,5]. Mesenteric lymphangiomas are multilocular or unilocular fat or fluid attenuation masses with thin walls[6]. Cavitating mesenteric lymph node syndrome is recognized as lipid-containing
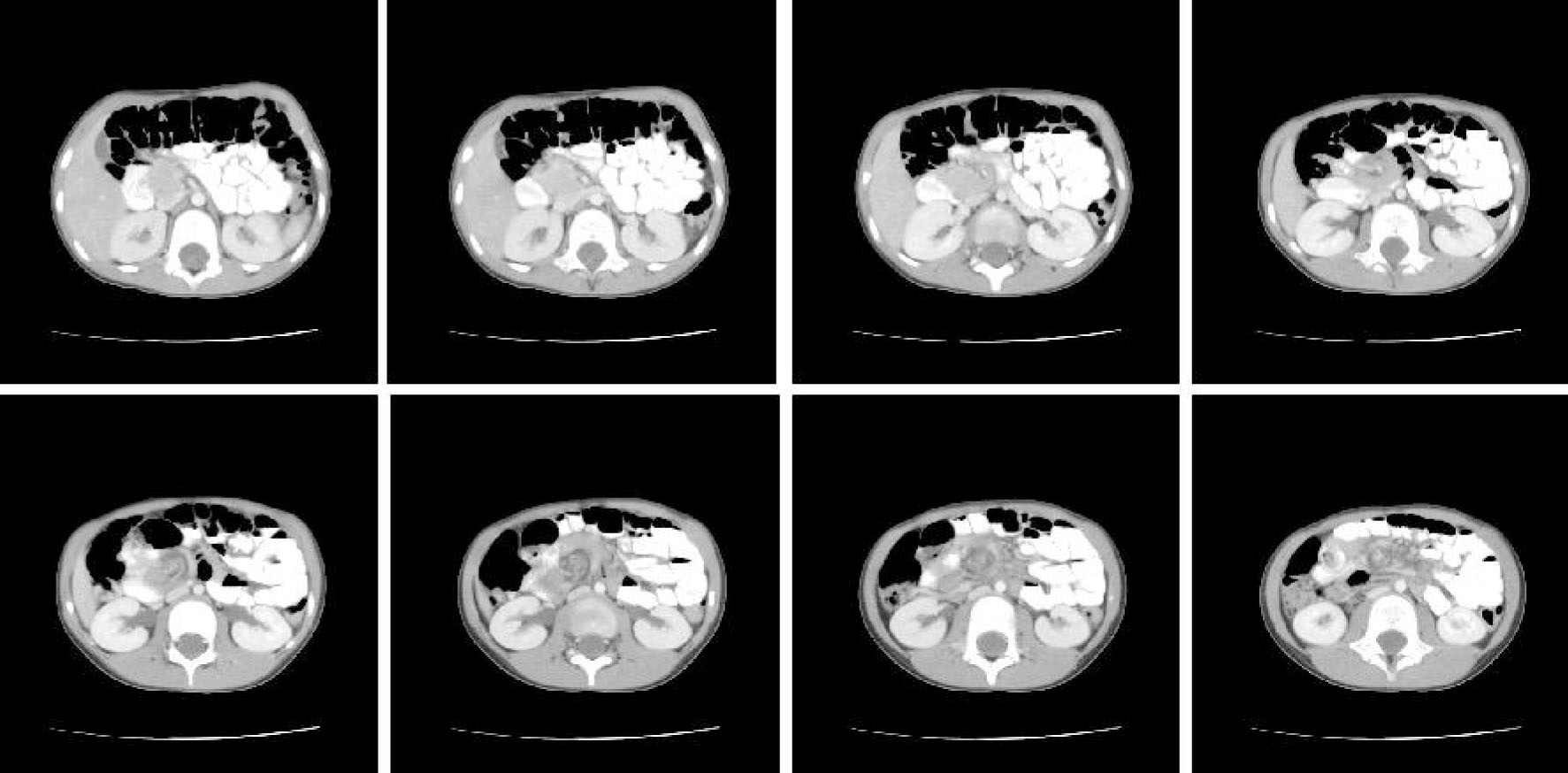
Fig. 2: Contrast enhanced CT scan showing twisted appearance of volvulus of midgut (about 360° clockwise) around the mesenteric vessels
Fig. 3: Gross view of lipoma at antimesenteric border of terminal ileum, before resection
mesenteric nodal masses and may be found in patients with celiac sprue[7].