Fulltext
Wernicke's encephalopathy (WE) is a potentially fatal, neuropsychiatric syndrome and absolutely a neurological emergency caused most commonly by thiamine deficiency[1]. It is recognized by the constellation of symptoms including ataxia, confusional state, and diplopia. The disorder is still significantly missed, leading to death or to the chronic form of the encephalopathy recognized as Korsakoff's syndrome[2]. Herein, we describe the disease in a girl who suffered from acute myeloblastic leukemia (AML).
A 12-year-old female, known case of AML M4 was consulted due to mild confusion, diplopia, and ataxia. Her disease had started 6 months prior to admission. She had received bone marrow transplantation from her brother 40 days before. On neurological examination, she was mildly confused with right sixth nerve palsy and truncal ataxia; also, she demonstrated gait ataxia and impaired finger to nose test prominently on the right side. For the better evaluation, brain MRI was recommended. On T2 weighted axial brain MRI (Fig. 1, parts A and B), hyperintense lesions in middle cerebellar peduncles, and similar intensities in the tectum and tegmentum of midbrain on the left side were detected; furthermore, on brain T1 weighted MRI with contrast (Fig. 1, part C), severely intense enhancement in mammillary bodies was seen; on the other hand, diffusion weight brain MRI revealed hyperintense lesions in the medial
portions of thalami (Fig. 1, part D).
According to the clinical findings in conjunction with imaging studies, the diagnosis of WE was made and thiamin was started. In the next day visit, ocular palsy had resolved completely.
We believe that malnutrition stemming from persistent loss of appetite as a result of the chemotherapeutic agents or the leukemia itself may have provoked thiamin deficiency and had caused WE.
The clinical settings in which WE takes place is growing; conspicuously, in conditions like alcohol consumption, prolonged feeding through parenteral routes, hyperemesis gravidarum, AIDS, anorexia nervosa, thyrotoxicosis, malabsorption states, dialysis, malignancy, and gastroplasty with postoperative vomiting[3].
Previously, few authors have described the association of acute lymphoblastic leukemia (ALL) and Wernicke's encephalopathy[4-9]; likewise, on the subject of AML, the reports are scarce, too[10,11]. Baek et al[10], described a case of acute WE arising following allogeneic peripheral blood stem cell transplantation accompanying with prolonged administration of total parenteral nutrition. Also, Pitella et al[11] reported a 30-year-old female suffering from WE associated with promyelocytic leukemia which was detected at autopsy.
In WE, characteristic radiologic findings on brain MRI consist of symmetric signal changes in the thalami, mamillary bodies, tectal plate, and periaqueductal area[12]. Atypical MRI findings comprise symmetric alterations of the cerebellum, vermis of cerebellum, cranial nerve nuclei, red nuclei, dentate nuclei, caudate nuclei, splenium, and cerebral cortex[12].
In conclusion, the possible occurrence of Wernicke’s encephalopathy should be regarded
in young patients encountering confusion or other neurological deficits who are suffering from malignancies especially when concurrent chemotherapy is administrated. It is significant that clinical suspicion is of utmost importance in the diagnosis and treatment of WE since delayed diagnosis may potentially cause devastating results.
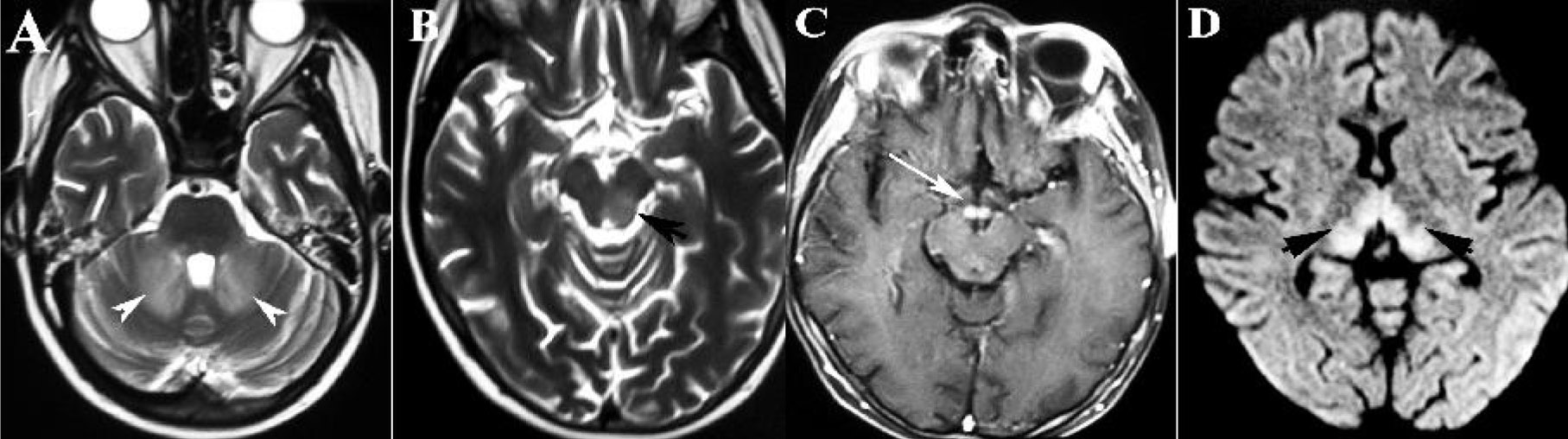
Fig. 1: Brain MRIs demonstrating hyperintense lesions in middle cerebellar peduncles on axial T2 weighted brain MRI (Part A), similar intensities in the tectum and tegmentum of midbrain on the left side (Part B), intense enhancement of mammillary bodies on the T1 weighted MRI with contrast (Part C), and hyperintense lesions in the medial portions of thalami in diffusion weighted MRI (Part D).