Dear Editor
Sogrens Syndrome (SS) is an uncommon condition in the pediatric age group. SS is a chronic autoimmune disorder mainly affects salivary and lacrimal glands, with varying degrees of systemic involvement. SS occurs usually after 40 years and nine times more common in females (1, 2). Primary SS, is not associated with any other illness, and secondary develops in the presence of autoimmune disorder such as rheumatoid arthritis, lupus, scleroderma or polymyositis (1). Clinically the hallmark symptoms of SS are dry mouth (xerostomia) and dry eyes (xerophthalmia). Recurrent parotid swelling is the common feature in children unlike in adults (1, 3). We report a nine -year-old patient with primary SS who presented with dry mouth, dry eyes, and recurrent parotid swelling.
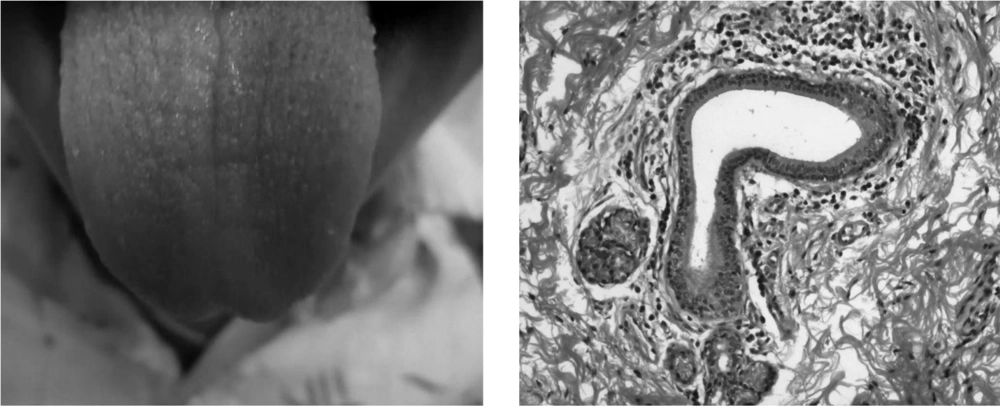
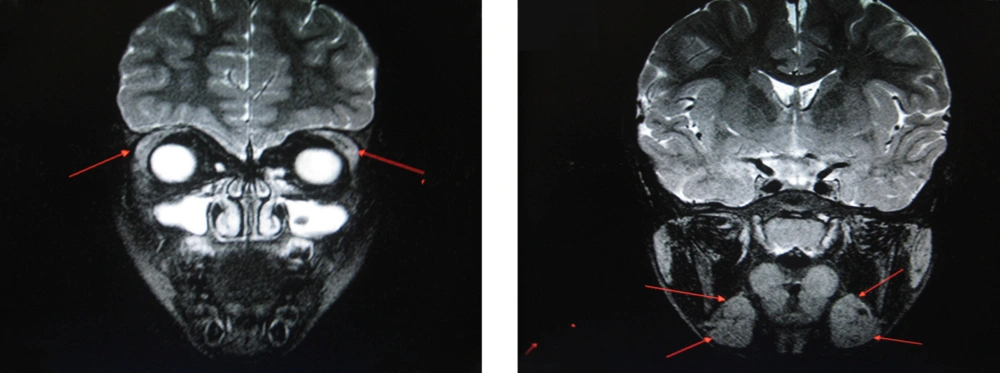
A nine-year-old boy presented with recurrent swelling of bilateral parotid glands since one year, dryness of mouth and eyes since six months ago. There was no history of joint pains, jaundice, drug ingestion, skin lesions, radiation or family history of autoimmune disorder. His weight and height were in 25th percentile. On examination he had dry oral mucosa, dry fissured tongue (Figure 1) and bilateral parotid enlargement. His conjunctiva was lusterless, tear film non uniform and break-up time was less than ten seconds. The rest of the systemic examination was normal. Investigations: Hb 12 gms/dL, WBC 8800 cells/cu.mm with normal differentiation, platelet count 390.000/cu mm, ESR 35 mm in first hour, urea 21 units/L, creatinine 0.7 mg/dL, sodium 139 mEq/L, potassium 3.9 mEq/L, AST 26 units/L, ALT 18 units/L and Amylase 42 units/L. His serology for RF, HCV, Hepatitis B, HIV, CRP, ANA, anti-double stranded DNA, Anti-SSA, Anti-SSB were negative. Ultrasonography of the parotid, submandibular and lacrimal glands showed hypoechoic areas with enlargement. MRI showed enlarged and hyper intense parotid, submandibular, sublingual and lacrimal glands on T1 images (Figure 2). His Schirmers test was positive (Right eye 3 mm, left eye 4 mm at 5 minutes), flourescin staining demonstrated superficial punctate keratitis. Minor salivary gland biopsy from lip revealed salivary acini and periductal lymphocytic and plasma cell infiltration (Figure 1). Our child fulfilled 4 AEC criteria for SS out of 6 with histopathological evidence. Child was started on refresh tear eye drops and advised to come for regular follow up.
SS is a chronic inflammatory systemic autoimmune disease mainly affecting the exocrine, particularly the salivary and lacrimal glands. SS consisting of xerophthalmia and xerostomia with or without autoimmune disease is uncommon in children. The clinical and immunological features of SS in childhood have not been adequately described in the literature. Children with SS demonstrate a clinical heterogeneity comparable to that seen in adults (4). Recurrent parotid enlargement appears to be important as an initial manifestation of SS in children and was observed in our child also (3, 5-7). Keratoconjunctivitis symptoms include dry eyes with reduced tear production, gritty or sandy sensation under the lids, red eyes, and photosensitivity like in our case. Mouth mucosa appears dry and parchment like. Diagnosis depends on AEC criteria in adults and our boy fulfilled the required criteria. AEC criteria proposed by Vitali et al. 2002 (8) are 1) Dry eye symptoms of 3 months duration 2) Dry oral symptoms 3) Evidence of ocular involvement [Schirmer test 5 mm in 5 minutes] 4) Lymphocytic sialadenitis from minor salivary gland biopsy 5) Objective instrumental evidence of salivay gland involvement 6) Presence of auto antibodies (Anti-SSA, Anti-SSB). To say SS, 4 criteria out of 6 and one must be either a positive biopsy or auto antibodies should be present. Exclusions are Hepatitis C, HIV, radiation and drugs. Still et al concluded that even if young patients do not completely fulfill the required criteria, SS can be assumed or confirmed in the presence of positive testing for oral and ocular manifestations and recurrent salivary gland enlargement (9). The inclusion of recurrent parotitis increases the sensitivity of the pediatric criteria and should alert the clinician to the possibility of SS (3). Civilibal et al. in their review of 146 cases observed that 77% were females with 9.8 years as the mean age of onset (6). Out of those 66.4 % had eye involvement, 43.2% had xerostomia and 69.9% parotid enlargement. They also noted RF in 66.2%, ANA in 78.2%, Anti-SSA 74.4% and Anti-SSB 64.8% (6), Minor salivary gland biopsy is the gold standard for the diagnosis (6). Periductal lymphocytic infiltration is regarded as consistent finding of SS (1, 2) and the same was seen in our case. In our child serology was negative. Probably serology in males may take some more time to become positive. Male patients seem to have less systemic manifestations and lower frequency of autoantibodies (10). Recurrent parotid swelling is the common feature and any child who presents with this should be investigated for SS (3, 5, 9). Our child had typical features of SS along with recurrent parotid swelling. Juvenile recurrent parotitis (JRP) mimics SS and characterized by recurrent swelling associated with pain, fever, erythema and absence of autoantibodies and no infiltration of lymphocytes in the salivary glands in contrast to SS (6). To conclude, even though rare, SS should be considered in the differential diagnosis of children with recurrent parotid swelling, keratoconjunctivitis sicca, or xerostomia.