Dear Editor,
Hydrocarbon compounds such as petroleum jelly and mineral oil can cause lower respiratory disease named exogenous lipoid pneumonia because of high viscosity and surface tension (1).
Acute exogenous lipoid pneumonia occurs after exposure to large amounts of mineral oils. The acute form in children is mostly a consequence of accidental poisoning. (2). Consolidation, nodular lesions, reticular and alveolar-interstitial patterns are the most common findings in the chest X-rays. Lower lobes or right middle lobe commonly get involved, but multifocal and bilateral lesions are shown too (3). The diagnosis of exogenous lipid pneumonia is made by a positive history of mineral oil exposure and radiologic findings in favor of the disease and revealing lipid-laden macrophages on bronchoalveolar lavages (BALs) or sputum specimen. Multiple BALs can remove Lipid-laden macrophages as a leading cause of fibrosis in the alveoli and interstitium (3, 4).
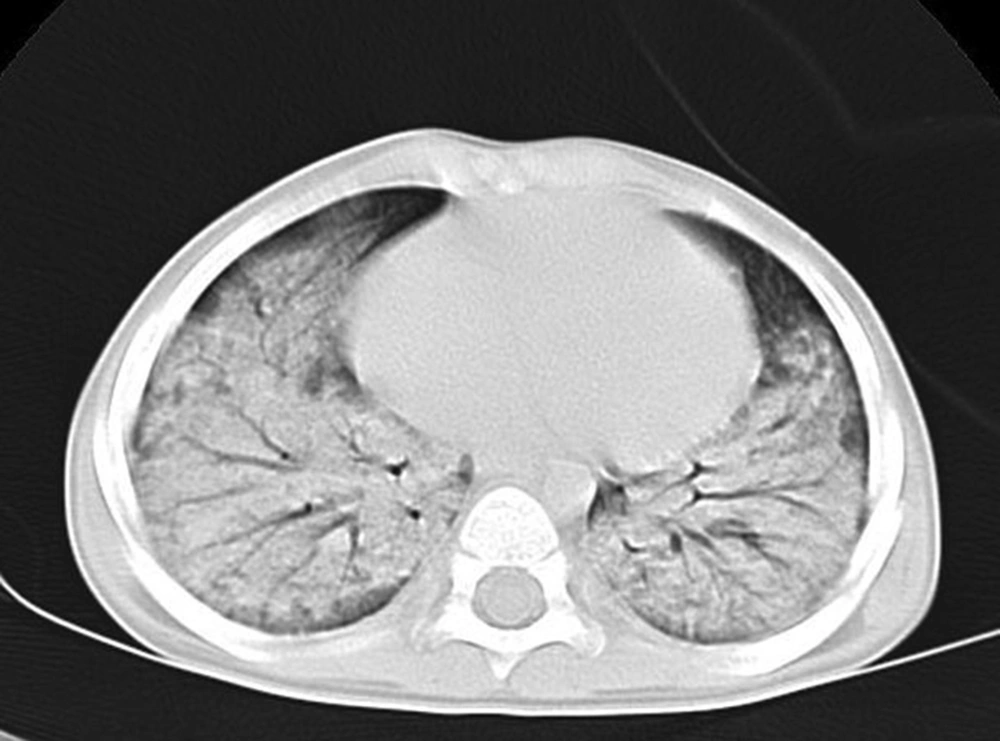
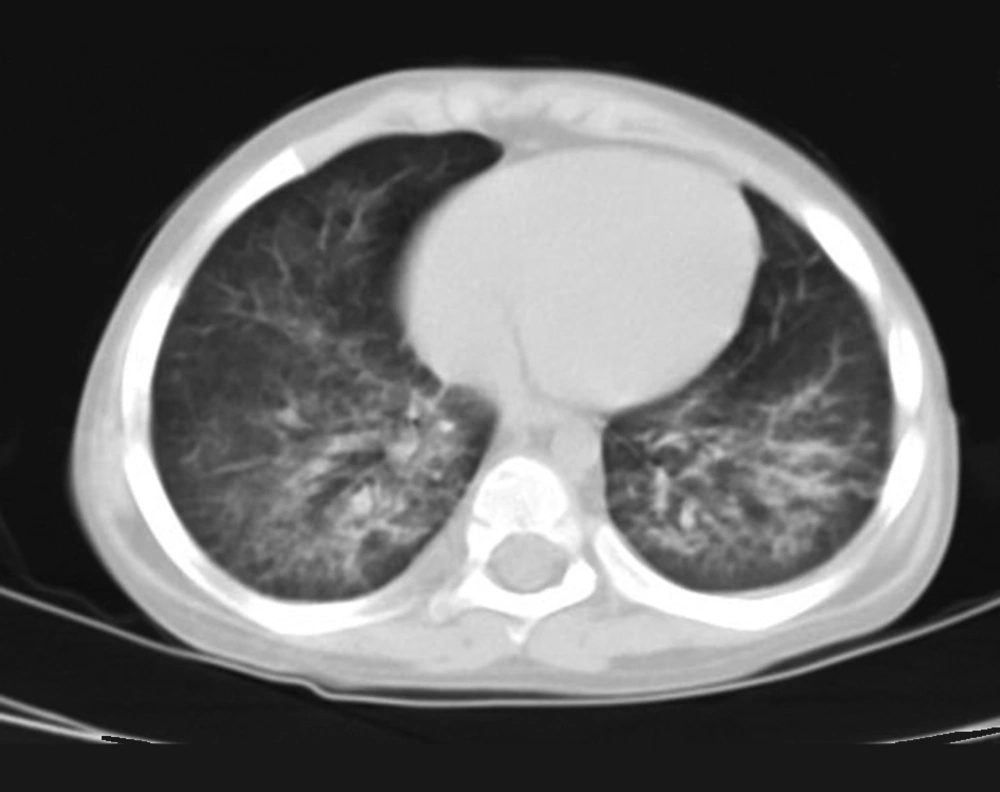
We present a rare case of exogenous lipoid pneumonia in a 2.5-year old boy with a history of mineral oil aspiration who admitted to the pediatric intensive care unit because of cyanosis and severe respiratory distress. On physical examination he presented with tachycardia (190 min), tachypnea (80 min), O2 saturation 50%, numerous crackles on auscultation of both lungs. Laboratory findings were leukocytosis with a left shift and increased CRP. A chest X-ray showed diffuse opacities with an alveolar pattern in both lungs (Figure 1). CT scans of the chest revealed bilateral diffuse severe pneumonitis with ground glass and alveolar appearance and crazy paving (Figure 2). Bronchoscopy was done. Mucopurulent secretions aspirated then rinsed with saline. After staining the BAL fluid with Sudan III many lipid laden macrophages (grade IV/IV) were seen. Multiple segmental BAL was done weekly, after that BAL fluid became nearly clear and cell counts reached near the normal range values. CT scan which was done after the forth therapeutic BAL, showed dramatic improvement in both lungs (Figure 3). The patient discharged after one month hospitalization and recommended to return to follow up.
The best way to remove the oil is multiple BALs especially in the most severely involved segments (3). According to several surveys, multiple BALs is an effective therapeutic strategy with few risks, and better improvement in the clinical and radiological signs (5). The present study indicates that therapeutic multiple segmental BAL is a successful method in removing intra-alveolar mineral oil with significant resolution of clinical, radiological and laboratory findings.