1. Introduction
UD is a rare congenital malformation which is more frequently found in males and often associated with other abnormalities of the genitourinary tract, heart, bowel and bones (1, 2). Various theories have been proposed for the embryological development of UD such as incomplete mesodermal fusion, abnormal Mullerian ducts, ischemic events in the embryogenesis and defect in the development of the urogenital sinus (3). It has various clinical types and treatments.
Diagnosis of UD is based on genital examination and will be confirmed by VCUG or retrograde-urethrogram. Management of UD is a challenge for pediatric surgeons and depends on different types of this anomaly (2, 4, 5). We present a case of type IIA1 urethral duplication in a 4-year-old boy with the literature review.
2. Case Presentation
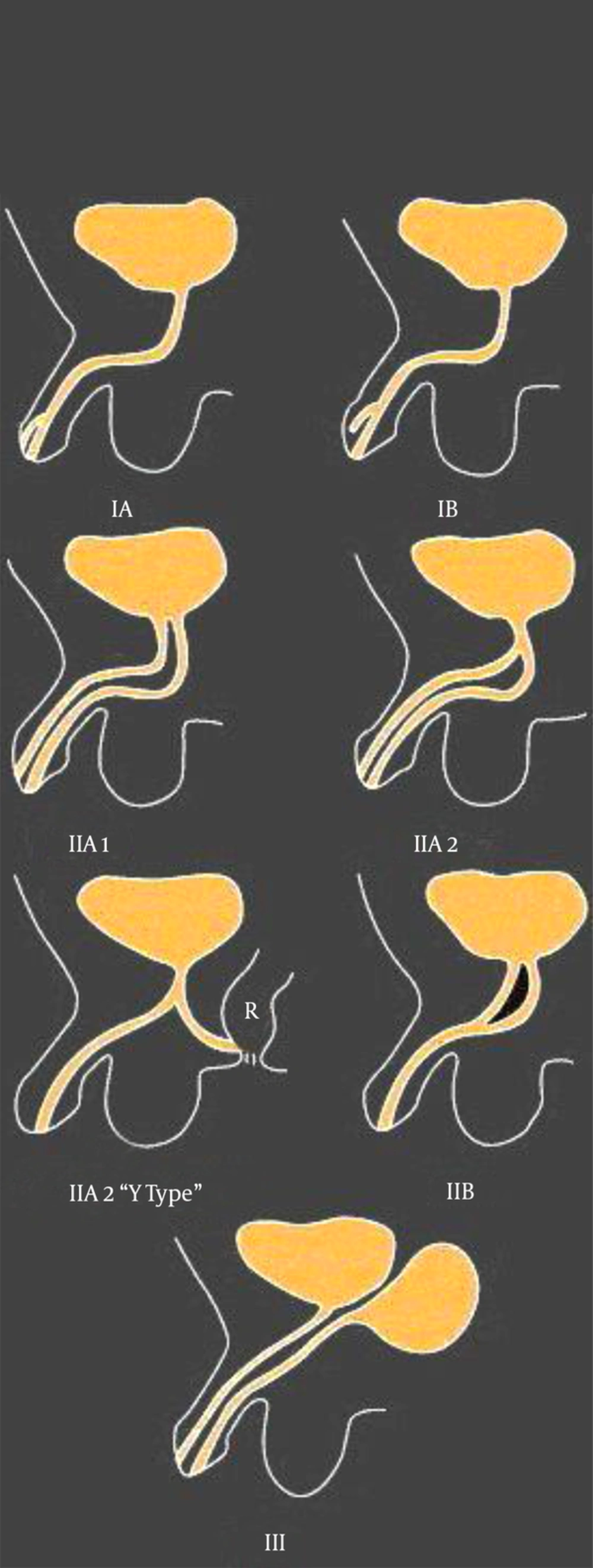
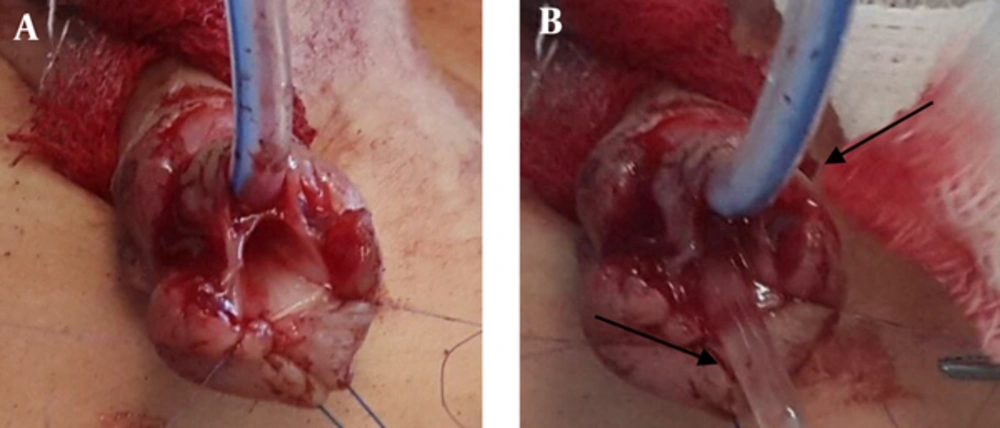
A four year old male child was presented with hypospadias and double meatus since birth. There was a normal meatus at the apex of the glans and a secondary meatus on the ventral aspect of the glans and distal-shaft. External genitalia were well developed, urination was continent and mostly from hypospadiac meatus. Voiding cystourethrogram (VCUG) showed a complete double urethra (Figure 1) as Effmann type IIA1 (Figure 2). Renal ultrasonography and intravenous pyelography revealed normal kidneys and no associated anomalies were seen in upper/lower urinary system. BUN and creatinine were within normal range. External genitalia were normal and the patient was not suspicious of ambiguous genitalia. Distal shaft hypospadias was surgically repaired saving complete UD (Figures 3 and 4). No complication was seen postoperatively.
Choice of surgical procedure in these patients depends on the type of anomaly. In this particular and rare anomaly we believe that this procedure was the appropriate one. The patient was followed up for one year, and no urinary problem was detected. In the recent visit he was in good condition and urine continent.
3. Discussion
UD is a rare anomaly that was first described by Aristotele, mostly in males with genito-urinary and gastro-intestinal anomalies (6). Arena et al. (2) found that in 60% of cases it is accompanied by genito-urinary malformation such as ureteropelvic junction obstruction, extra rotation of the penis, vesicoureteral reflux, renal ectopia, renal agenesis or posterior urethral valves, but we found no associated anomaly in our case. Okur et al. classified UD as a complete second passage from the bladder to the dorsum of the penis or as an accessory pathway that ends blindly on its dorsal or ventral surface, but the most common accepted classification is that of Effmann (7). The most common type of UD is the Y type with a perineal or rectal fistula associated with stenosis of the anterior portion of the normally situated urethra (8). According to this classification our case is type IIA1 in which both urethras have normal anatomical position and normal urinary continence. Diagnosis of UD is based on genital examination and will be confirmed by VCUG or retrograde-urethrogram. Evaluation of the normal functioning of urethra is mandatory (9). Preoperative cystoscopy confirms the apical urethra and shows the presence of the verumontanum (10-12). Surgical treatment of UD depends on the anatomic type of anomaly and also clinical findings and severity of the associated anomaly (13-15). In our case the hypospadias accessory urethra was normal, so it was saved and repaired. The patient had normal and continent urination and the long-term outcome was very good.