1. Context
Neonatal mortality rate is declining globally and fell from 40 to 33 deaths per 1,000 live births between 1990 and 2013. In Iran it fell from 27 to 10 in this time period and accounts for more than half of the under-5-year child mortality (1-3). Evidences from trend studies show that neonatal mortality decline has slowed down and neonatal deaths account for a larger share of U5MR (4).
The office for neonatal health in Iranian ministry of health developed and implemented various plans to improve the healthy and also sick newborn care. Availability and access to care is essential but not sufficient to get desirable outcome. The quality of care plays crucial role.
Health care systems seeking quality and accountability need to assess the performance of facilities and monitoring changes to display trends in measures. Assessments are needed at every level of health care from community setting to level III referral hospitals. The point is to identify what should be assessed. An author introduced “quality black box” because it is extremely difficult to exactly measure what must be measured as a quality indicator (5). Donabedian’s categorization of measurement of quality consisting of indicators for structure (personal characteristics and institutional features), process (activities in providing care), and outcome (result of care) is an accepted approach (6).
2. Evidence Acquisition
Nine bibliographic data bases, 4 Iranian (SID, IranDoc, Magiran, medlib) and 5 international (Pubmed, scienceDirect, googlescholar, Scopus and Cochrane), were searched. It was limited by publication time 1990 - 2013. Multiple combinations of keywords were used: neonatal care, perinatal care, newborn care, quality, quality indicators, evaluation, evaluation mechanism, assessment, quality assessment and performance. Gray literature search was done on the world health organization (WHO), American academy of Pediatrics and Iranian Ministry of Health websites. Manual search was carried out for unpublished materials simultaneously. Researchers reviewed the title and abstracts independently and in a sitting selected abstracts which did not met exclusion criteria for full text review. Exclusion criteria were: not reporting neonatal care measures and non-Persian/English language. At the next stage, full texts were reviewed. References cited in retrieved articles were also searched and screened. Those papers that actually met the inclusion criteria were included in the study (Table 1).
3. Results
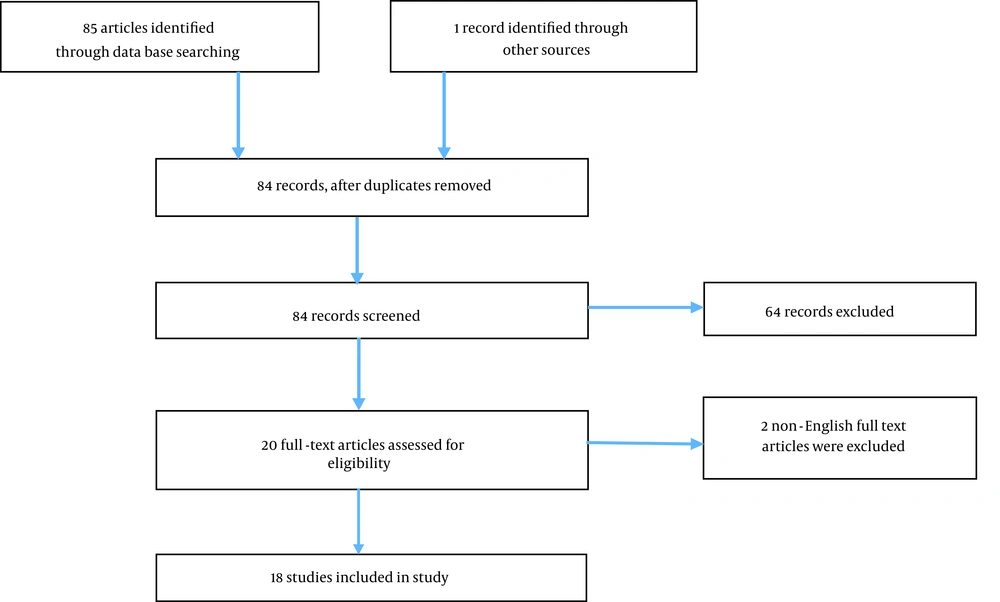
The process of searching bibliographic data bases, selection and number of papers retrieved in each phase is shown in Figure 1.
| Author/s | Country | Study Design | Quality Measure | Publication Date | Reference |
|---|---|---|---|---|---|
| USA | Delphi | Antenatal steroids, timely retinopathy of prematurity exam, late onset sepsis, hypothermia on admission, pneumothorax, growth velocity, oxygen at 36 weeks postmenstrual age, any human milk feeding at discharge, in-hospital mortality | 2011 | ( | |
| USA | HIS data analysis | Surfactant use rate for premature babies | 2011 | ( | |
| India | Cross sectional survey | Nurse: bed ratio, Doctor: bed ratio, Reported time (months) for repair of essential equipment, Asepsis score, Average duration (days) of stay, Bed Occupancy rate | 2011 | ( | |
| USA | Cross sectional survey | Regulation of regionalization programs, data surveillance, review of adverse events | 2012 | ( | |
| Estonia | Population based reports | Proportion of infants born by cesarean, received antenatal corticosteroids, maternal antibiotics, and surfactant | 2012 | ( | |
| India | Review | Regionalization of perinatal care, staff: bed ratio, existence of residential medical staff, NMR | 2012 | ( | |
| UK | Population-wide observation | Volume of neonatal specialist care (≥ 2000 neonatal intensive care days annually), having an acute transfer (within the first 24 hours after birth) and/or a late transfer (between 24 hours and 28 days after birth) to another hospital, assessed by change in distribution of transfer category (“none,” “acute,” “late”), and babies from multiple births separated by transfer | 2012 | ( | |
| Switzerland | Neonatal mortality data base 0f 38 countries | NMR trends | 2011 | ( | |
| Italy | Survey | Existence of basic amenities, existence of essential drugs and equipment, hygienic practice, existence of surveillance system | 2011 | ( | |
| UK | Review | skilled care before/during/after birth and maternal/newborn mortality/morbidity | 2013 | ( | |
| Italy | Before-after observational study | No. of nurses, doctors, drugs, equipment: bed, normal delivery/ section proportion, thermal control, use of Apgar score, promotion of breastfeeding, neonatal resuscitation, mothers more involved in neonatal care, training more staff in effective perinatal care | 2013 | ( | |
| USA | Record linkage | The percentage of very-low-birth-weight deliveries in level 3 hospitals, mortality: volume of NICU | 2007 | ( | |
| UK | Retrospective observational | Mortality of VLBW before discharge to home in each hospital level | 2004 | ( | |
| Norway | Review | Regionalization implementation, promotion of breast feeding, investing in equipment and staff, evidence-based treatment, training programs | 2011 | ( | |
| Sweden | Retrospective observational | Fetal mortality rate, neonatal mortality rate, infant mortality rate. Distribution of birth weight, distribution of gestational age, prevalence of congenital anomalies, distribution of Apgar score at 5 min | 2004 | ( | |
| USA | Retrospective observational | NICU mortality rate, standardized mortality ratio, standardized NICU length of stay ratio | 2000 | ( | |
| IR Iran | FGD | Advanced resuscitation certificated staff attendance rate during resuscitation, pediatrician/pediatric resident attendance rate during resuscitation, neonatologist/neonatology fellow attendance rate during resuscitation, existence of residential pediatrician/neonatologist, FHR monitoring during labor, partograph filling for vaginal deliveries, parent’s training before discharge, resuscitation form filling for performed ones, fetomaternal transfer rate, neonatal transform organized by transfer guide, hypoxia on admission, mean/median duration of NICU stay, mean/ median duration of mechanical ventilation in NICU, proportion of newborns who receipt required follow up, perinatal mortality rate, primary c/s rate, repeat c/s rate, mother readmission rate | 2010 | ( | |
| USA | Multiple center cohort | Bronchopulmonary dysplasia (BPD), periventricular/intraventricular hemorrhage or periventricular leukomalacia (PIVH/PVL), and retinopathy of prematurity (ROP). duration of hospital stay and days on a ventilator for those infants who received mechanical ventilation, organizational measures: quality of teamwork and leadership, degree of relationships and communications within the NICU, degree of coordination, perceived unit/team effectiveness, authority, quality of conflict resolution, job satisfaction | 2003 | ( |
Overview of the Included Studies
Reviewing the papers, 87 indicators were extracted. Among them, 13 were duplicates. Remaining measures were classified in input (n = 14), process (n = 31), and outcome measures (n = 29). Assessing the hand searched documents 25 indicators were derived of which 7 were duplicates. Considering the 18 input indices, 41 process and 34 output indices were obtained (Table 2).
| Nurse: bed ratio |
| Doctor: bed ratio |
| Reported time (months) for repair of essential equipment |
| Existence of residential medical staff |
| Existence of basic amenities |
| Existence of essential drugs |
| Existence of essential equipments |
| Skilled care before birth |
| Skilled care during birth |
| Skilled care after birth |
| No. of equipments: bed |
| No. of drugs: bed |
| Investing in equipment |
| Investing in staff |
| Advanced resuscitation certificated staff attendance rate during resuscitation |
| Pediatrician/pediatric resident attendance rate during resuscitation |
| Neonatologist/neonatology fellow attendance rate during resuscitation |
| Existence of residential pediatrician/neonatologist |
| Antenatal steroids |
| Timely retinopathy of prematurity exam |
| Hypothermia on admission |
| Surfactant use rate for premature babies |
| Regulation of regionalization programs, |
| Data surveillance |
| Review of adverse events |
| Maternal antibiotics |
| Having late transfer (between 24 hours and 28 days after birth) to another hospital |
| Having acute transfer (within the first 24 hours after birth) to another hospital |
| Hygienic practice |
| Thermal control |
| Use of apgar score |
| Promotion of breastfeeding |
| Neonatal resuscitation |
| Mothers more involved in neonatal care, |
| Training more staff in effective perinatal care |
| Evidence-based treatment, |
| Training programs |
| Distribution of apgar score at 5 min |
| Standardized NICU length of stay ratio |
| Duration of hospital stay |
| Gays on a ventilator for those infants who received mechanical ventilation |
| Organizational measures: quality of leadership |
| Organizational measures: quality of teamwork |
| Degree of relationships and communications within NICU |
| Degree of coordination |
| Authority, quality of conflict resolution |
| Job satisfaction |
| Bed occupancy rate |
| Volume of neonatal specialist care (≥ 2000 neonatal intensive care days annually) |
| FHR monitoring during labor |
| Partograph filling for vaginal deliveries |
| Parent’s training before discharge |
| Resuscitation form filling for performed ones |
| Fetomaternal transfer rate |
| Neonatal transform organized by transfer guide |
| Hypoxia on admission |
| Mean/median duration of NICU stay |
| Mean/median duration of mechanical ventilation in NICU |
| Proportion of newborns who accept required follow up |
| Late onset sepsis |
| Pneumothorax |
| Growth velocity |
| Oxygen at 36 weeks postmenstrual age |
| Any human milk feeding at discharge |
| In-hospital mortality |
| Asepsis score |
| Average duration (days) of stay |
| Proportion of infants born by cesarean |
| NMR |
| NMR trends |
| Maternal mortality |
| Maternal morbidity |
| Neonatal morbidity |
| Normal delivery proportion |
| Section proportion |
| The percentage of very-low-birth-weight deliveries |
| Mortality: volume of NICU |
| Mortality of VLBW before discharge home in each hospital level |
| Fetal mortality rate |
| Distribution of birth weight |
| Distribution of gestational age |
| Prevalence of congenital anomalies |
| Standardized mortality ratio |
| Bronchopulmonary dysplasia (BPD) |
| Retinopathy of prematurity (ROP) |
| Periventricular/intraventricular hemorrhage |
| Periventricular leukomalacia |
| Perceived unit/team effectiveness |
| Perinatal mortality rate |
| Primary c/s rate |
| Repeat c/s rate |
| Mother readmission rate |
| Case fatality rate for neonatal disease |
Retrieved Neonatal Care Measures, Categorized Using Donabedian Model
4. Conclusions
This is the systematic review with the main aim of providing a tool for evaluating quality of neonatal care in hospitals at any level. Evaluation is essential for improving provided health care and also comparing different settings. We perused the original and reviewed papers for the recommended indicators. We considered infrastructure, equipment and staff as input, admission, treatment, care practices, referral, discharge and follow up as process indices. Newborn health status, care outcome and consequences were categorized as outcome indicators.
The structural factors are essential for quality of care in health care facilities, yet it is clear that these aspects are not sufficient to assure high quality, as currently, process and outcome measures are more emphasized.
As can be seen, much of the proposed or applied indicators are in the process group, indicating the importance of components of good care. According to this criterion, a health care setting should be assessed by reviewing medical records, direct observations and interviews with care provider and recipients to determine to what extent the provided care is acceptable according to the level of facility. Nevertheless there are three noticeable points regarding these indicators. First the measuring, which is more complicated than the other two categories and require assessing multiple sources for data extraction-the accuracy of which is questionable-that lessen the feasibility. The other point is that the standard care is so variable among different areas of the world and in one and the same place would differ over time. Finally they do not indicate whether the patient is better off.
Actually some authors recommend to choose those process measures that scientific evidence illustrates they link to improved outcomes (25, 26).
Outcome measures refer to effectiveness of the care provided. They consist of early (proximal) and late (distal) outcomes. Although such measures have traditionally been mortality and morbidity, outcomes research in recent years has expanded the measures to include patients’ perception of their health status and the services (technical care and also interpersonal relationship) that they receive. The point that must be considered is that determining health care outcome at discharge will miss some complications that appear just after discharge and we should think of recording patient’s data after discharge at follow up care.
Presumably there are some indicators that haven’t been mentioned and some of which do not fit the Iranian settings. Therefore, qualitative studies are required to obtain the expert’s opinion and integrate both results to make a list of appropriate measures for evaluation of quality of perinatal care provided in Iranian settings.