1. Context
Premature birth is an unexpected event, which can cause parental distress. Depending on the degree of prematurity and the severity of the disease, the infant may have to be hospitalized for a long time in a neonatal unit (1). Concerns about the health and survival of the baby, in addition to the complexity of medical care and technology employed in the neonatal ward, can deeply distress parents (2). In fact, the appearance and behavioral response of the infant causes stress in parents; besides, the experience of developmental challenges of parental role increase their stress because their baby is taken care by the medical staffs and in a strange environment. At the same time, it is expected that parents support not only their sick baby, but also other family members including other children (3). Feeling of stress and problems of role playing as a normal parent can continue long after the infant has been discharged from the hospital. Longitudinal studies of families with preterm infants have shown that long after the baby’s discharge, families were faced with many problems in daily life and in compliance with the ongoing situation (4). Thus, from both medical and social perspectives, it is important to provide the best nursing and medical care, as well as social support for families in the neonatal ward, which should be continued even after discharge (5), and comprehensive care plans should be continued, which cover hospital care, information about baby care, and community-based care, including home visits by medical staff, and the development of supportive groups (6).
Despite numerous investigations, the insights gained from research were not sufficient for agents who have dedicated themselves to the establishment of family-centered care, and incompatibility and heterogeneity of understanding the needs of parents still exist (7).
Proper accountability of the needs of preterm infants’ parents requires recognition of these needs and how they change in various conditions and regions. In this regard, the classification of needs is a useful tool for planning and providing appropriate interventions.
The aim of this study was to review studies that discussed the needs and supportive requirements in different stages from the perspective of parents of preterm infants in Iran and other regions of the world.
2. Evidence Acquisition
Using standard tools, all quantitative studies that considered the parental needs of preterm infants and parental supports were included in the study. Qualitative and interventional studies were excluded from the study. Two independent researchers selected English and Persian articles from Iranian databases (Iran Medex, Magiran, and SID) and international databases (PubMed, Scopus, and Google Scholar), without time limitations to 5 October 2014. As some of the Iranian databases showed no sensitivity to search operators (AND, OR, NOT), the search was done in the local database only through the keyword premature baby to achieve accurate results. In the search of the international databases, the researchers used the general keywords preterm OR premature and family OR mother OR father OR parent to ensure high sensitivity. Resources were investigated by two browsers independently. At the beginning of the study, to identify studies with the inclusion criteria, the researchers reviewed the title and abstracts of the obtained articles. Full-text articles were reviewed, and the required data were extracted. In addition, the reference lists of the selected articles were screened to identify relevant studies. Moreover, for access to certain additional information (exact standard deviation) communicated with some authors.
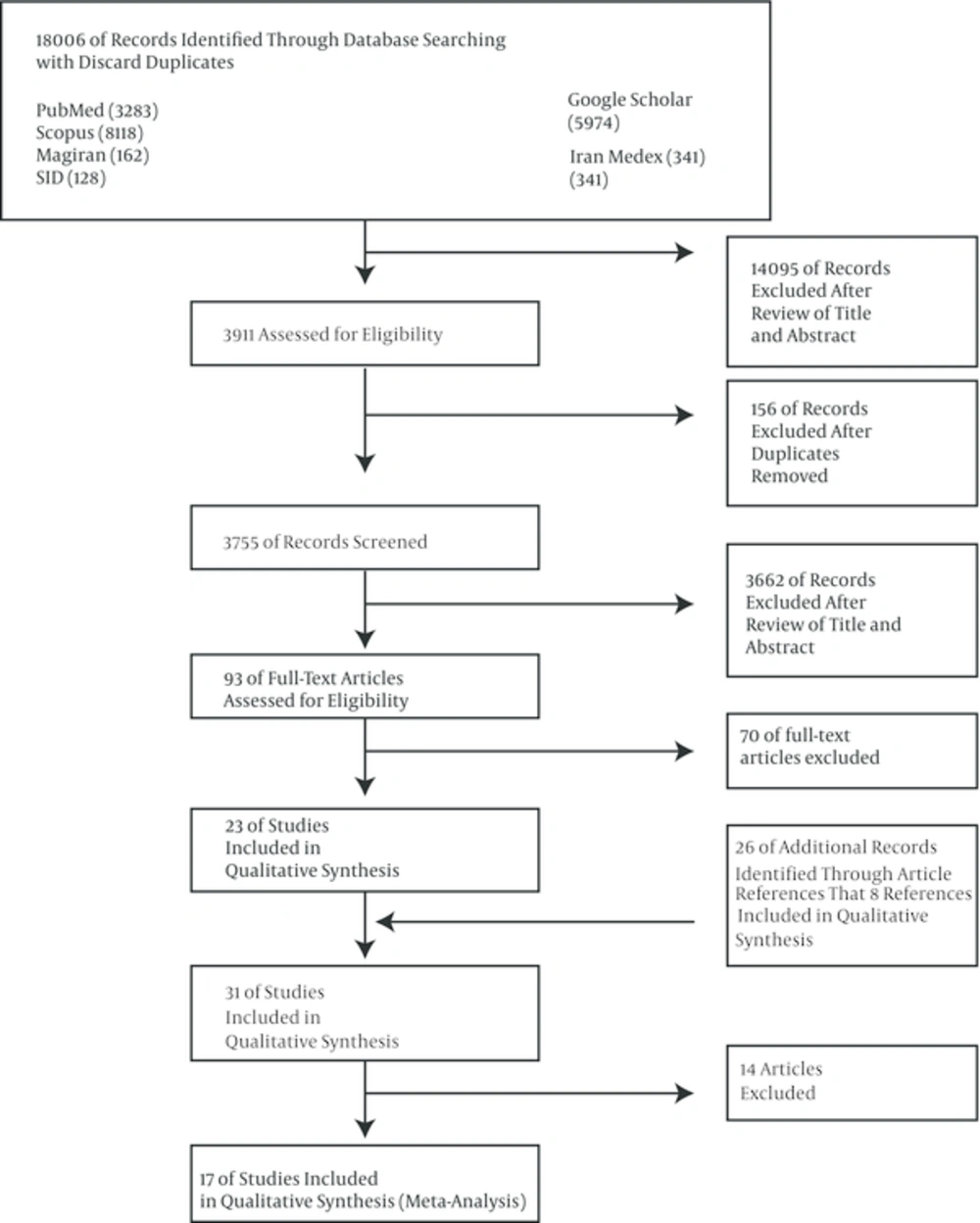
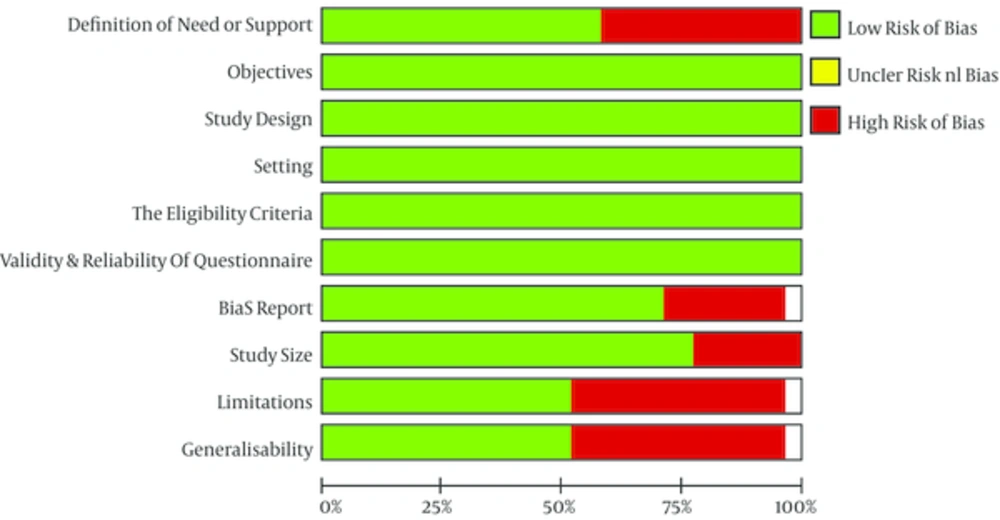
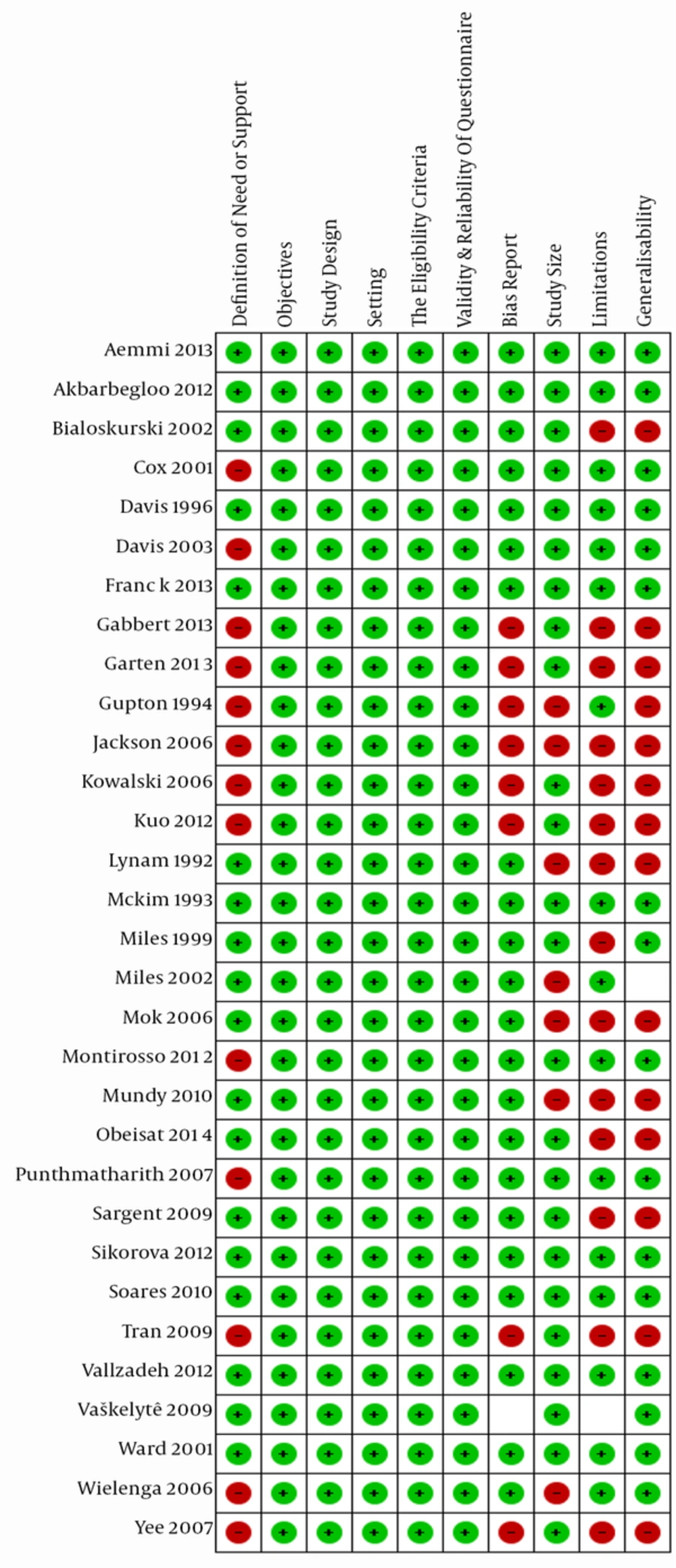
Figure 1 shows a summary of the selection process. Ten items of the STROBE (strengthening the reporting of observational studies in epidemiology) list were used for evaluating the studies (8). The items were: a precise definition of the need or support, an accurate explanation of the purpose of the study, an explanation of the key components of the study design, a detailed description of the time and location of the study, a detailed description of the inclusion criteria and methods for the selection of the study participants, an explanation of the validity and reliability of the instruments, attention to sources of bias and insufficient numbers of samples, attention to limitations of the study, and the possible generalization of the study.
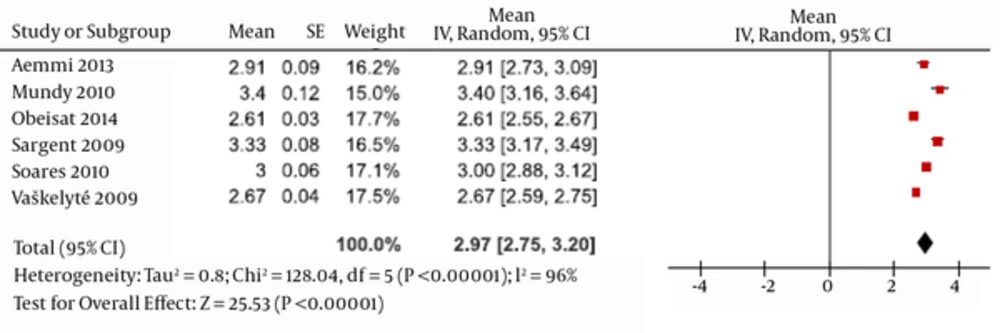
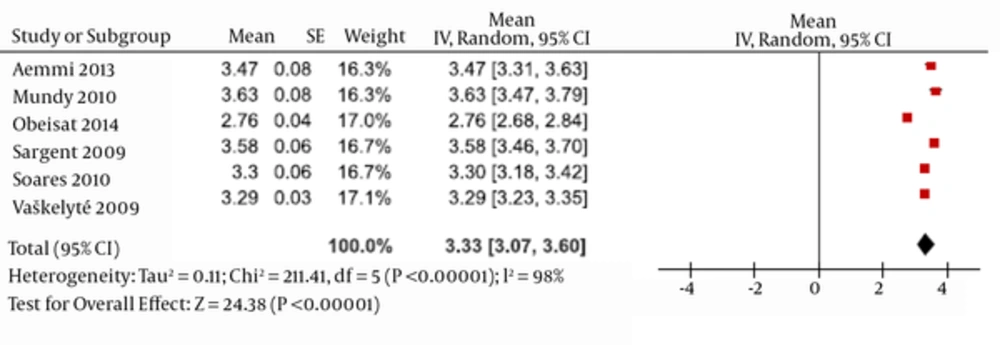
Two independent researchers were responsible for all stages of the evaluation of the articles. In cases of disagreement between the two researchers, an article was judged by a third researcher. Table 1 presents a summary of the extracted data and properties of the studies, Figures 2 and 3 display the assessment related to the quality of studies.
Review Manager 5 software was used for the data analysis (9). Statistical heterogeneity was investigated using the chi-square test at a significance level of 5% (P < 0.05). Lack of consistency between studies was examined using I2 statistics (10). The variance between studies was estimated using tau-squared (Tau2) (11). A meta-analysis was done to capture summary of amount of support and needs. The data were reviewed, and the results were analyzed using a random-effect model and a 95% confidence interval (CI) (12).
3. Results
Thirty-one studies were included in the qualitative evaluation, among which 17 studies were selected for the meta-analysis according to the study’s objectives and inclusion criteria. The nurse-parent support tool (NPST) (3) instrument was used in 11 studies, and the neonatal family needs inventory (NFNI) (13) tool was implemented in seven studies In the remainder, the postpartum support questionnaire (14), critical care maternal needs inventory (7), critical care family needs inventory (15), quality of care from the patient’s perspective questionnaire (QPP) (5), five anonymous instruments (16-20), premature labor needs questionnaire (PLNQ) (21), preterm birth learning needs questionnaire (PBLNQ) (22), parenting needs questionnaire (6), and antenatal consultation questionnaire (ACQ) (23) were used. In 31 of the studies in this review, 15 studies included only mothers, 15 studies included both fathers and mothers, and one study focused specifically on the needs of fathers.
3.1. Meta-Analysis Results
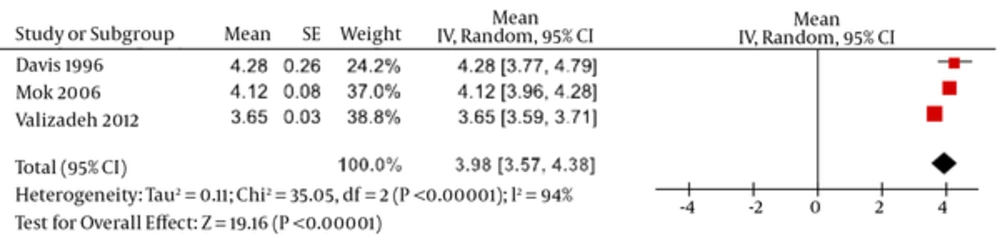
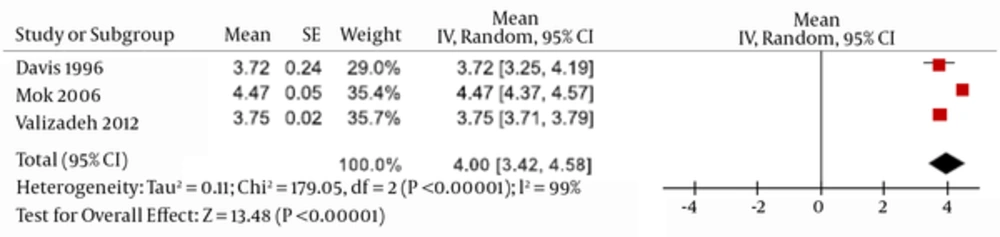
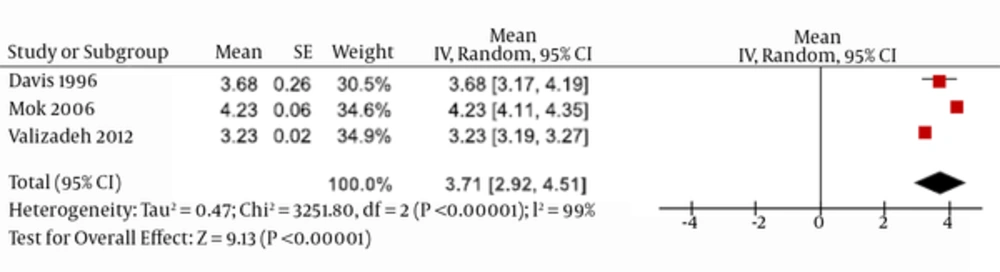
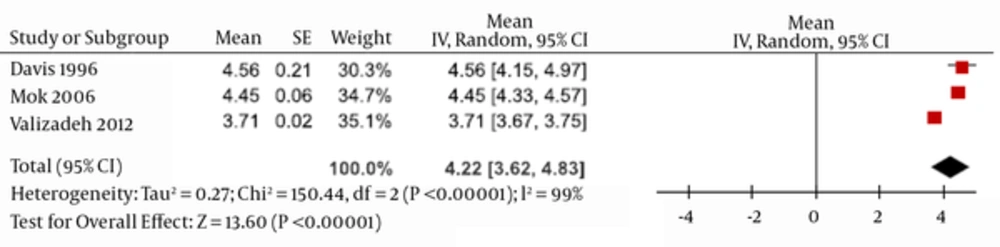
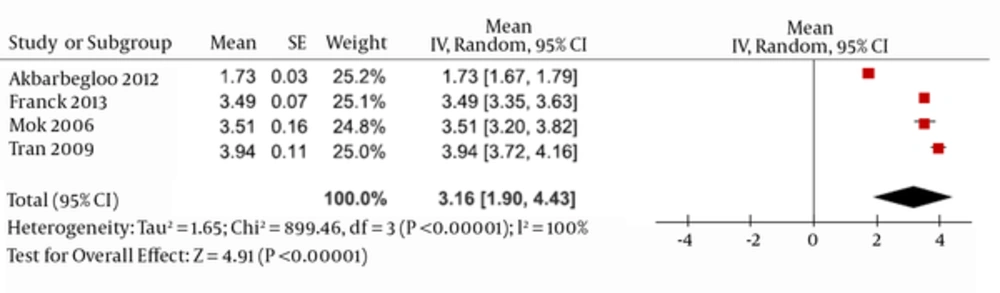
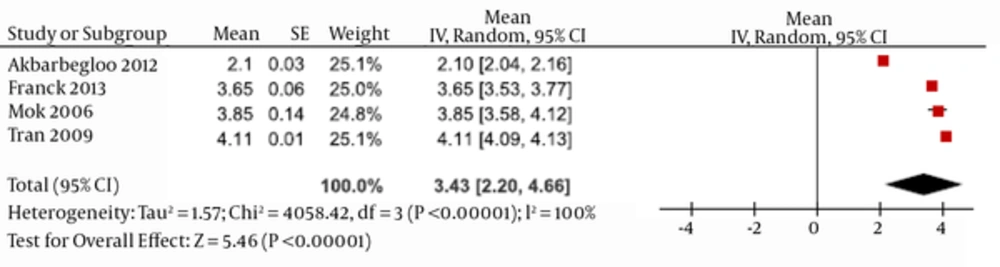
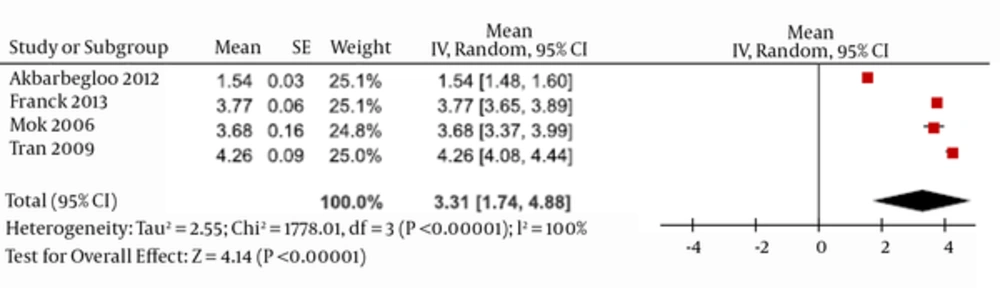
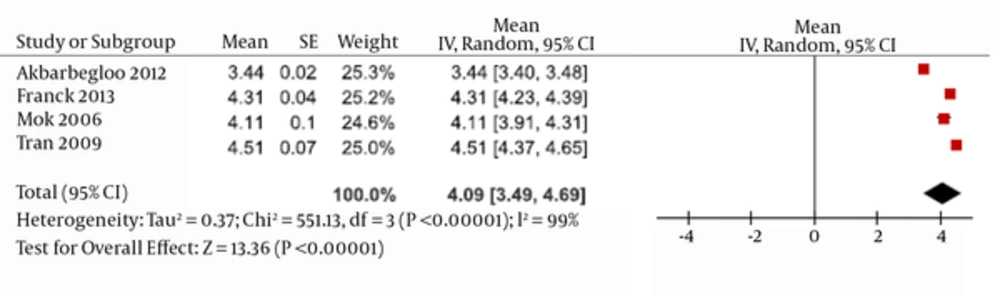
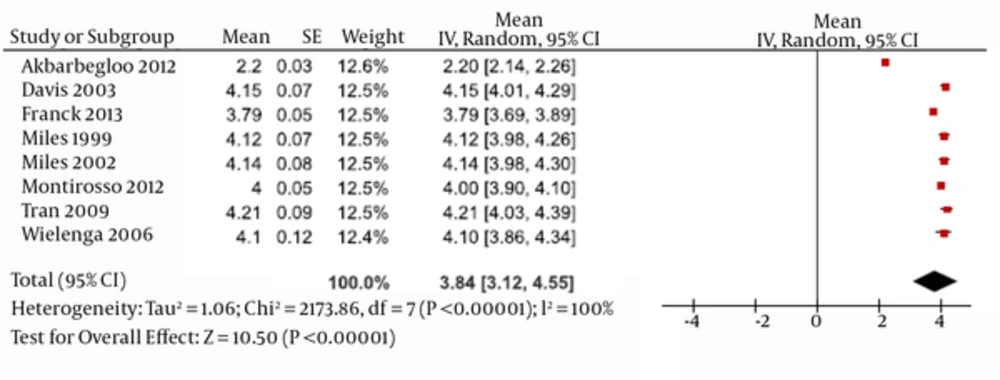
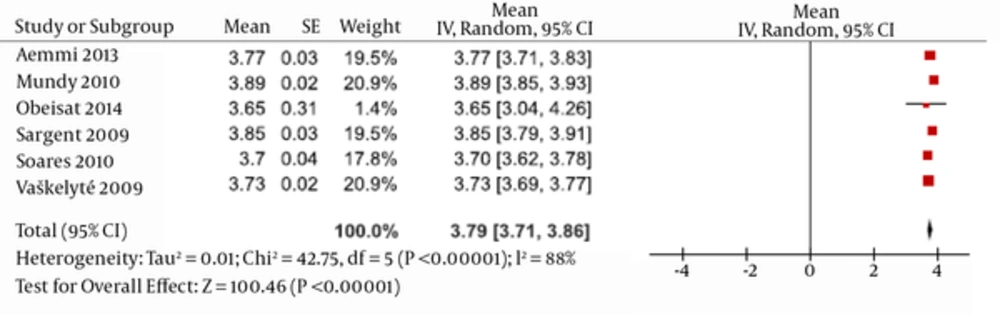
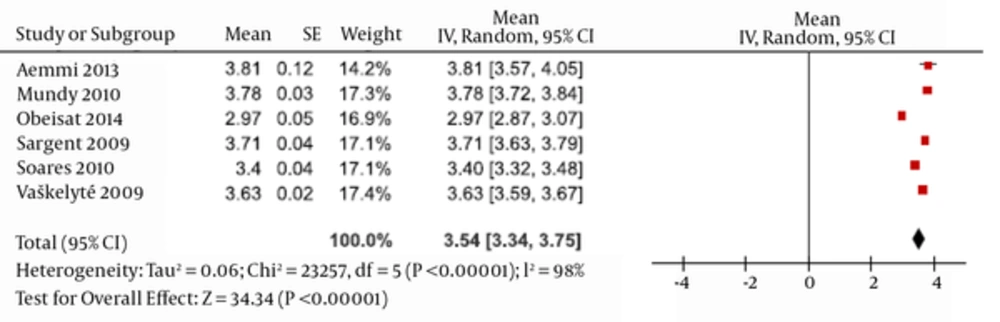
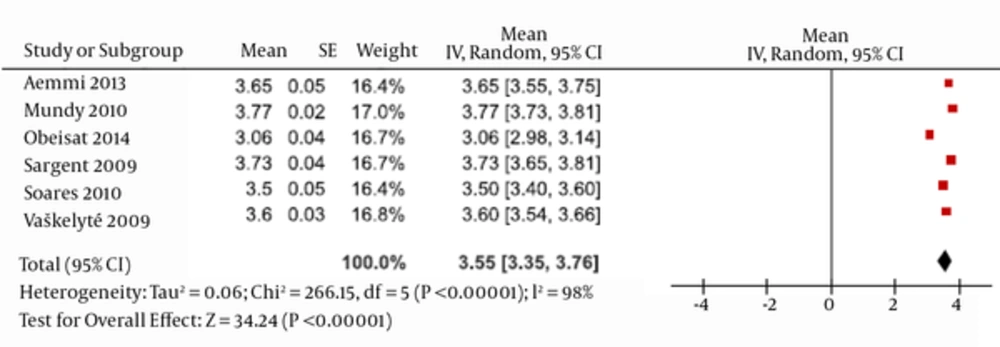
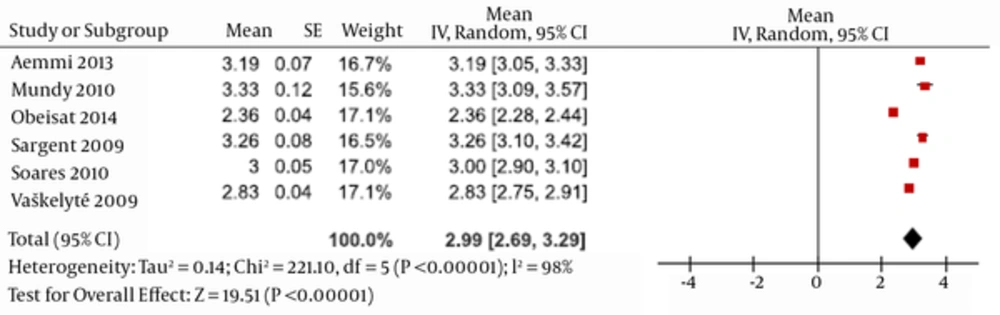
Seventeen articles were included in the meta-analysis, and the results were arranged in two fields of support and need, separately. Figures 4 - 12 present the results that were obtained using the NPST. The NPST questionnaire consisted of 21 items. Answers were ranked based on a 5-point Likert scale, with a score of 1 and 5 indicating minimum and maximum support in different situations, respectively. With regard to ranking support, 1 - 2.59 denoted a low rate, 2.6 - 3.59 indicated an intermediate level, and 3.6 - 5 signified a high rate (24).
3.2. The Importance of Different Types of Support
Figures 4 - 7 illustrate the importance of support in different fields from the parents’ point of view. As shown, all issues were ranked high (> 3.6), and instrumental, informational, emotional, and appraisal supports were considered important.
Figures 8 - 12 show the parents’ assessment of the support received. Parents generally evaluated received support to be high (< 3.6). However, regarding their assessment of the different types of support they received, only instrumental support was ranked high. In other areas, the informational, emotional, and appraisal supports were separately rated to be medium (2.6 - 3.59), and the lowest rate related to emotional support. The mean scores for the parents’ assessments of the provision of emotional, information, appraisal, and instrumental support in Iran compared to those in other countries were 1.73 ± 0.06 vs. 3.18 ± 1.34, 2.1 ± 0.06 vs. 4.11 ± 0.5, 1.54 ± 0.6 vs. 4.26 ± 0.18, and 3.44 ± 0.04 vs. 4.51 ± 0.14.
3.3. Parental Evaluation of Needs
Figures 13 - 18 illustrate the parents’ evaluation of needs using the NFNI tool (13). The total score for needs in Obeisat’s study in Germany was significantly lower than that in the other countries (i.e., Iran, U.S. Brazil, and Lithuania). Thus, the results of Obeisat’s study were disregarded when calculating the heterogeneity. When this study was excluded, the heterogeneity decreased from 98% to 88%.
4. Conclusions
4.1. NPST
This tool focuses on four areas of instrumental, emotional, appraisal, and informational-communicational support (3). In the present study, the NPST focused on the importance of the support provided and the actual received support from the perspectives of both the parents and medical staff. With regard to the mothers’ perspective, the results showed that all fields of support were ranked as very important. In this regard, instrumental, informational, emotional, and ultimately appraisal supports achieved some degrees of importance, respectively. In Iran, compared with other regions (i.e., the U.S. and Hong Kong), all the fields of support, except information, received lower scores. This field was close to instrumental support and was located on the top. Despite the importance that parents considered for different aspects of support, they were not satisfied with various fields of support, except with instrumental support. The received supports in other aspects were assessed as intermediate, with emotional support being considered as the most neglected field. In Iran, other than instrumental support, which was evaluated as medium, the received supports in other parts got a low score. The scores for received support in Iran were much lower than those in other countries (i.e., Italy, the U.S., Australia, and the Netherlands). When the results of the Iranian studies were disregarded, and the heterogeneity was calculated, the I² scale decreased from 100% to 82%.
4.2. Instrumental Support
This type of support refers to any action specifically associated with infant care (25, 26). Interestingly, both in rating fields and in rating the amount of received supports, instrumental support was located in highest point of importance. In fact, parents’ stress reduce when they feel their babies received skilled care (27). Although nurses and other health team members provided highly specialized care for premature infants, many mothers were engaged with their maternal role restrictions. Unfortunately, severe conflicts have been reported between parents and nurses that often were due to deterrent actions of nurses in order to marginalize parents and keep their role and authority as experts (28). Mothers were aware of the imbalance of power (29). Although they tended to be involved in their infant’s care, they also accepted the nurses’ role in facilitating and supporting the development of the parental role (7, 13, 25, 26). The findings indicate that the health team should have knowledge of their duties and have positive, open, and reliable communication with parents, without any judgment. Practical standard should indicate the health team’s commitment to support open communication with parents in an effort to help parents reduce their anxiety, and staff training should be based on establishing positive relationships and supporting family-centered care (30).
4.3. Informational-Communicational Support
This type of support focuses on providing information regarding the infant’s disease, treatment, care, and development needs, in addition to emotional and behavioral responses and parental rights and responsibilities during hospitalization. In the current study, informational-communicational support was ranked as the second most important type of support. Research has shown that the provision of continuous and appropriate information to parents about the condition of their infant helps to ensure that the parents become more active partners in taking care of their infants (26).
4.4. Emotional Support
Emotional support includes listening to the feelings and concerns of parents, showing concern about the health of the parents, as well as that of the infant, and taking practical measures to protect them and help them cope with the impact of disease and other aspects of the infant’s life (31-33). The third area of support that parents sought was emotional support, although it was located in the lowest step in terms of received supports, and from the parents’ view point, the highest gap between claimed and received support related to this field, especially in Iran.
4.5. Appraisal Support
This field is defined as reinforcement for parental role and is the next field of support that parents would have focused on. The identity-oriented performance of the medical team that leads to both empathy with parents and respect of their dignity, involves them in the process of caring for their baby, and promotes the medical-technical capabilities of caregivers, creates a socio-cultural atmosphere, which can strengthen the confidence of parents in taking parental roles (5). To fill the gap between the perceived and received support, the health team should be encouraged to consider whether the type and amount of support provided are in accordance with the needs and views of parents. Adopting various family-centered strategies, such as family centered rounds and facilitating the participation of parents in decision making, can be effective in reducing this gap (25, 34).
4.6. NFNI
This tool focuses on the needs in five areas: assurance, proximity, awareness, support, and comfort (13). Average scores given for each field of needs, with scores higher than the average indicating the perceived importance of each area. In the present study, generally, the parents believed that needs within the field of assurance were the most important issues the fulfillment of which can persuade parents to continue their infant’s admission in NICU. After this issue, awareness, proximity, support, and finally comfort were located, respectively.
4.7. Assurance
The assurance item was ranked as most important, as infants’ parents are exposed to fear, anxiety, and uncertainty about the fate and future health of their infant in the NICU. It can be implied that the need for being heartened about the survival of the baby was the first priority. Hence, the expression of reciprocal empathy and concern by staff, as well as the use of inspiring and encouraging words along with care, can be very valuable (3).
4.8. Support
The parents ranked the need for support as low. This may be associated with the lack of parental support programs in the NICU where the included studies were conducted. Not having an opportunity to experience the potential benefits of participation in family support groups may affect the priority of needs from the parents’ perspective (35).
4.9. Comfort
Parents ranked the importance of personal comfort as lowest, as their main concern was for their infant (7, 15).
4.10. Proximity
The need to be close to the infant and have physical contact with him/her is important for parents. In Iran, the need for proximity was placed in the first priority. This may be due to the lack of open-door policies and unrestricted presence (36). Parents were so concerned about dangerous situations, such as incorrect care, inadequate attention to the baby, and unskilled care (29).
Special care of parents: There were correlations between maternal and neonatal characteristics and the needs of mothers (35, 37). The results showed that the availability of support programs for parents in the NICU are increasingly being taken into consideration. A special nurse as an interface in neonatal ward and maternal and child health units has been evaluated positively by both fathers and mothers (38, 39). Planning for the activation of outpatient resources at national and local levels, with a focus on creating environments that present the integrated medical care, upgrading the provision of comprehensive family-centered community-based services, and providing tips for parents to access these centers seem necessary (40).
4.11. Conclusion
In general, it can be concluded that the parents prioritized the needs of the infant over their individual needs. To improve services for parents, the needs of both parents and infants should be considered. Frequent and periodic health assessments should be undertaken to determine whether the type and level of support provided are in line with the needs and views of parents. Given the lower scores assigned by Iranian parents in their assessments of the received support, it is important to focus on these specific items in providing interventions to meet parental needs of preterm infants.
| Author | Year | Sample Size/Study Group | Instrument | Age (SD) | Major Findings |
|---|---|---|---|---|---|
| Franck (25) | 2013 | 227 parents (NICU) 192 mothers/35 fathers | NPSTa | 32.02 (6.36) | The difference between nurses’ and parents’ ratings was smallest for instrumental support (0.26, 0.16–0.36; P<0.001) and largest for emotional support (0.82, 0.67 - 0.97; P < 0.001). |
| Akbarbegloo (40) | 2012 | 300 mothers | NPST | 25.57 (5.6) | A comparison of the viewpoints of mothers and nurses revealed a significant difference between four dimensions of nursing support (P < 0.001). |
| Valizadeh (30) | 2012 | 300 mothers | NPST | 25.57 (5.6) | There was a significant difference between the opinions of the nurses and mothers on the importance of support (in all subscales, except for communication and information) and the provision of support (P < 0.05). |
| Tran (41) | 2009 | 62 parents, 56 mothers/6 fathers | NPST | 31 | Instrumental support was rated the highest mean score for both nurse-to-parent support 4.51 (out of 5) and 4.36 for satisfaction. Emotional support was rated the lowest mean score for both nurse-to-parent support at 3.94 and 3.97 for satisfaction. |
| Montirosso (31) | 2012 | 156 mothers | NPST | 33.5 (4.8) | IBAg, a subscale of PSS: NICUh was predicted by NPST (B = -0.074). Mothers who had a higher level of IBA-related stress reported less staff support. |
| Mok (26) | 2006 | 37 mothers | NPST | 26-38 | The findings showed that the largest mean difference between perceived and received nursing support among four aspects of support was for supportive communication and information (0.62). |
| Sikorova (24) | 2012 | 147 mothers (NICU) | NPST | Most (21 - 30) | The greatest source of stress was related to the parental role. Mothers evaluated the support of nursing staff as good in all aspects. There was no relationship between stress relating to the parental role and the support of staff (r = -0.3926). |
| Wielenga (42) | 2006 | 46 parents, 35 mothers/11 fathers | NPST | 31.5 | The results showed that the greater the level of perceived support, the more satisfied the parents were (r = 0.893). |
| Miles (3) | 1999 | 108 parents, 72 mothers/36 fathers | NPST | Mothers: 26, Fathers: 28 | The NPST is an instrument to assess the amount of nursing support that parents receive during a child’s hospitalization. It evaluates four dimensions of support: supportive communication and information provision, parental esteem support, emotional support, and caregiving support. The internal consistency of each dimension is 0.95. |
| Miles (36) | 2002 | 31 black and 38 white mothers | NPST | Black mothers: 26 (6.2), White mothers: 28 (6) | Mothers with lower levels of education were more worried about their child than mothers with higher levels of education (F [1.59] = 4.1, P = 0.47). |
| Davis (43) | 2003 | 62 mothers | NPST | 29 (5.7) | The risk of depression significantly decreased with increased levels of mothers’ education (P < 0.05) and with higher levels of maternal education (P < 0.05) and increased understanding of support from nurses (OR: 1.06, CI: 0.88 – 1.00; P < 0.05). |
| Davis (14) | 1996 | 37 mothers | Postpartum Support Questionnaire | 27 (6) | Women reported that instrumental, emotional, and appraisal supports were more important than they had expected. Moreover, women received less support in all other fields, except appraisal support. |
| Mundy (44) | 2010 | 60 parents, (NICU), 43 mothers/17 fathers | NFNIb | 25.78 (6.91) | Families rated the fields of support in the following order: assurance, proximity, information, comfort, and support. Parents at admission in comparison with parents at discharge ranked the support need to be more important than other needs. Fathers’ and mothers’ needs were not significantly different from each other (P = 0.11). |
| Aemmi (35) | 2013 | 63 mothers | NFNI | 26.78 (6.26) | Families rated the fields of support in the following order: proximity (95.37%), assurance (94.18%), information (91.15%), support (79.77%), and comfort (72.86%). |
| Sargent (35) | 2009 | 46 mothers(NICU) | NFNI | 28.22 (7.57) | From the perspective of mothers, assurance was the most important item (3.85 ± 0.192), and support was the least important (3.26 ± 0.513) item. A multiple regression analysis showed that there was a significant relationship between annual household income and the mother’s need for support (β =-0.424, P < 0.01), as well as between the length of an infant’s stay in the NICU and mothers’ information needs (β = -0.438, P < 0.05). |
| Obeisat (45) | 2014 | 170/ Parents89 fathers/81 mothers (NICU) | NFNI | 35.2 (8.82) | Parents rated assurance (mean of 3.650), information (mean of 3.05), and proximity (mean of 2.96) as the most important items, and they ranked comfort (mean of 2.61) and support (mean of 2.34) as the least important items. Mothers rated the need for support, information, and proximity as more important than that of the other items compared with fathers (P < 0.05). |
| Ward (13) | 2001 | 52/ Parents, 42 mothers/10 fathers) | NFNI | 26.19 (6.68) | In general, support was ranked as the least important item, and assurance was ranked as the most important item. The needs for support, assurance, and information were more important for mothers than they were for fathers (P < 0.05). Mothers’ and fathers’ ranking of comfort and proximity were the same. |
| Vaskelyte (46) | 2009 | 181 parents, 141 mothers, 40 fathers | NFNI | 27.7 (6.9), 31.2 (6.4) | In this study, parents ranked their needs in the following order: assurance (mean of 3.73), proximity (mean of 3.63), information (mean of 3.60), support (mean of 2.84), and comfort (mean of 2.67). |
| Soares (47) | 2010 | 72 relatives, 38 mothers, 34 fathers | NFNI | 31.6 (10.1) | The findings indicated that the most important needs were those related to safety (3.7 ± 0.3), information (3.5 ± 0.4), and closeness (3.4 ± 0.3). |
| Bialoskurski (7) | 2002 | 209 mothers | Critical Care Maternal Needs Inventory | 27 | In the study, the priority for 93% of mothers was accurate information about their infants. They also valued good communication by experts. The mothers’ needs were a second priority to those of the infants. |
| Cox (15) | 2001 | 100 mothers | Critical Care Family Needs Inventory | NOT | Six fields of needs were determined and rated by mothers, namely information about the infant, communicational support (the need for communication with experts) from specialists, maternal social support systems, maternal priorities, maternal social requirements, and maternal emotional needs. |
| Jackson (5) | 2006 | 21 mothers, 20 fathers | QPPc | 33.4/34.4 | Subjective importance was ranked as more important than perceived reality for babies’ care regarding the dimensions of identity-oriented approach (P < 0.001) and medical-technical competence of staff (P = 0.009). |
| Gabbert (16) | 2013 | 136 parents, 79 mothers, 57 fathers | An anonymous self-reporting questionnaire | Most in their 30s | A total of 79.1% of the participants stated that they would be interested in joining a native language site that provided (1) general information about prematurity, (2) explanations of medical terms commonly used in a hospital setting, and (3) details of common medical problems and their treatment, including the availability of local therapists and follow-up services. Parents also wanted to be in contact with other families and experts to exchange personal issues. |
| Kowalski (17) | 2006 | 101 parents, 71 mothers, 30 fathers | A 19-item questionnaire | 29.7 (6) | Almost all (96%) the parents felt that they received accurate medical information and that they had a good relationship with the experts. However, parents believed that nurses were the ones who were assumed to give explanations about the baby’s condition. They were considered the best sources of information. They considered that nurses were also best able to explain important changes in the baby’s condition. |
| Punthmatharith (18) | 2007 | 420 mothers (NICU), (140 from each hospital) | questionnaire developed by the researcher | 26.69 | This study found significant differences (P < 0.05) between groups of mothers in three NICUs in three hospitals in terms of needs. The results supported the idea of individualized maternal needs. |
| Lynam (21) | 1992 | 14 mothers | PLNQd | 18 - 33 | Mothers reported that interdependence, physical-physiological, and role function needs were their important needs. |
| Gupton (22) | 1994 | 34 hospitalized women at risk of preterm birth | PBLNQe | NOT | Using a 20-point visual scale, some fields that were most important for parents were consequences of prematurity for infants (19.38 ± 1.65) and problems of the newborns associated with preterm birth (19.29 ± 1.66). |
| Kuo (6) | 2012 | 96 parents (NICU) 55 mothers/41 fathers | Parenting needs questionnaire | 32 | In this study, parents who had preterm infants had greater parenting needs than those who did not have preterms. (t = 2.0, P = 0.046). |
| Yee (23) | 2007 | 50 women | ACQf | 29.7 (5.4) | Although the mean state anxiety score was high (47.2, 84th percentile), 78% agreed that the consultation relieved parental anxiety about the baby. Participants wanted information about survival, probable medical problems, and the risk of disability, followed by information about medical treatments and breast-feeding. |
| McKim (48) | 1993 | 56 mothers | 26.85 (4.99) | A total of 48% of mothers believed that the first week after their infant’s discharge was difficult. The presence of a community health nurse during that first week was an important factor in whether parents considered the first week problematic (P = 0.02). | |
| Garten (19) | 2013 | 111/fathers | An anonymous self-report questionnaire | Most (31 -40) | Fathers (64.5%) stated that the support provided by the NICU team was sufficient. However, 54.4% of fathers reported a lack of bedside interventions, such as VLBW, father-specific baby care courses, seminars or workshops, and related networks. |
aNurse-parent support tool.
bNeonatal intensive care unit family needs inventory.
cQuality of care from the patient’s perspective questionnaire.
dPremature labor needs questionnaire.
ePreterm birth learning needs questionnaire.
fAntenatal consultation questionnaire.
gInfant behavior and appearance.
hParental stressor subscale: neonatal intensive care unit.