1. Introduction
Fournier’s gangrene, an infective necrotizing fasciitis of the perineal region, was first described by French venerologist Alfred Fournier (1, 2) in 1883. This aggressive and life threatening disease is uncommon in children and very rare in neonates and has a mortality rate of near 50% in this age group (3, 4). Prematurity, diaper rash, poor hygiene, trauma, anorectal diseases, urethral catheterization, circumcision, insect bite, strangulated hernia, omphalitis, systemic infections, immunocompromised status and hematologic malignancies are some predisposing factors in children (1, 4, 5). Congenital leukemia defined as leukemia diagnosed in the first 28 days of life, is quite rare with an incidence of 4.7 cases per million births (6, 7). The prevalence of acute myeloid leukemia (AML) is more than acute lymphoblastic leukemia (ALL) in neonates, with acute myelomonocytic (M4) and monocytic (M5) being the most common subtypes. AML has better prognosis than ALL in neonates (8). The presentation of leukemia is typically with hepatosplenomgaly, leukemia cutis and/or hyperleukocytosis. Leukemia as an immune-suppressed condition is an extremely rare risk factor for necrotizing fasciitis in neonates. Here we describe a rare case of the simultaneous occurrence of acute myeloid leukemia and Fournier’s gangrene in a neonate.
2. Case Presentation
Our patient was a 4-day-old female with a birth weight of 3,100 grams and a gestational age of 39 weeks born from non-consanguineous parents. Her birth history was unremarkable. She was first admitted to a local hospital for hyperbilirubinemia started at the third day of life. There was no history of poor feeding and fever. She was not ill or toxic on primary examination. After one day of hospitalization, fever started and she was referred to our hospital for further evaluation. Clinical examination at admission revealed an axillary temperature of 39°C, jaundice, hepatosplenomegaly and a necrotic lesion in perineum with swelling of the left labium major. Sharp margins of the lesion medially distended to the fourchette and anus and laterally to the origin of left thigh (Figure 1). There was no history of trauma or other predisposing condition. Initial diagnosis of necrotizing fasciitis and sepsis was made and she was treated by vancomycin and meropenem to cover both aerobic and anerobic organisms, in addition to other supportive measures.
Laboratory study showed; direct hyperbilirubinemia (total bilirubin 17.6 mg/dL, direct bilirubin 5.9 mg/dL), blood cell count abnormality (WBC 2,160, neutrophil 5% lymph 88%, mono 7%, Hb 12.8 gr/dL, Plt 21,000) and elevated CRP 41.9 mg/L. TORCH study was negative. Blood and wound culture grew Pseudomonas aeruginosa sensitive to meropenem and amikacin.
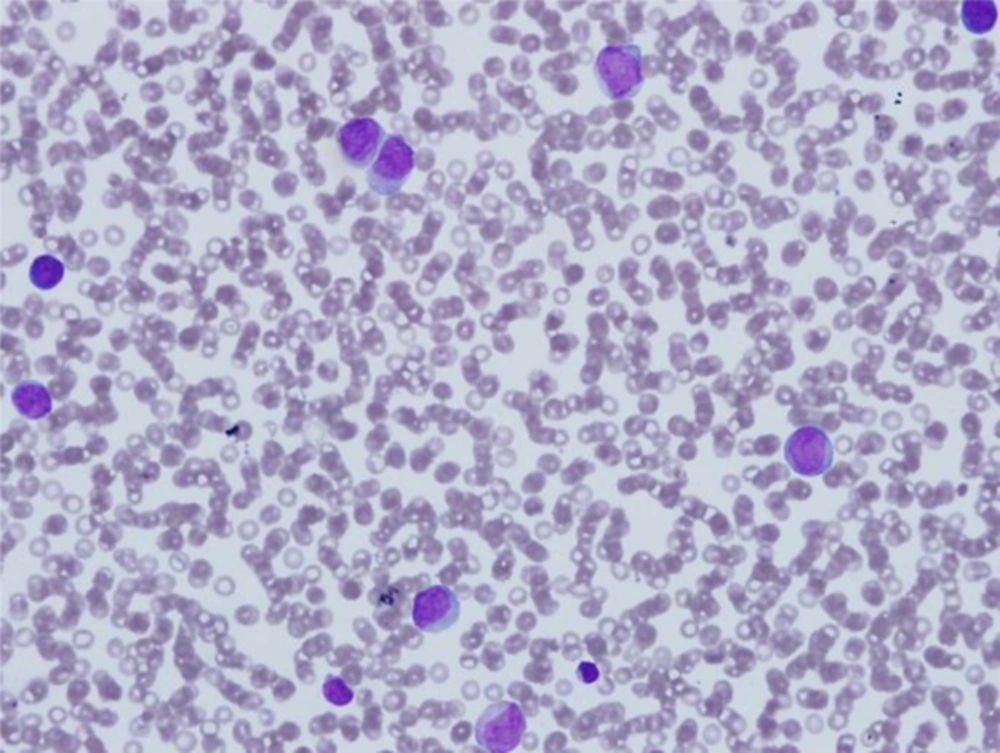
In the course of treatment, by repeating CBC we found leukocytosis with a high percentage of blast cells and persistent thrombocytopenia (WBC 18,490, neut 5.7%, lymph 15.1%, mono 26%, blast 52%, myelocyte 1%, RBC 2,800,000, Hb 8.8, Plt 29,000) despite proper antibiotic therapy. So a pediatrics hematologic consultation was requested to rule out malignancies. Bone marrow aspiration and flow cytometry was performed according to his suggestion. The result was; AML-M4 (Figure 2).
Skin lesion progressed from a superficial necrotic lesion to a deep soft tissue involvement in external genital area (Figure 3). Abnormal coagulation profile and poor patient’s condition banned the surgeon from performing any surgical procedure for skin lesion, so local treatment with N/S irrigation and sterile dressing continued. Parents refused chemotherapy and she was discharged against medical advice. Bleeding and DIC was the cause of her death in a local hospital few days later.
3. Discussion
Fournier’s gangrene (FG) is a fulminant form of infective necrotizing fasciitis that involves external genitals and perineal region. It is more common in adults but more than 56 pediatric cases have been reported so far, most of them being under 3 months of age (1, 2, 9). Although the male to female ratio is reported to be 10: 1, our patient is a female. FG affects females as well as males and cases of vulvar necrosis have been reported (10). Predisposing factors vary with age. Diabetes mellitus, chronic alcoholism, malnutrition and immunosuppressive therapy are underlying disorders for affected adults whereas predisposing and etiological factors differ in neonates including prematurity, trauma, poor hygiene, systemic infections, insect bite, burns, circumcision, disorders of immune system, anorectal and periurethral diseases, strangulated hernia, phimosis, omphalitis, varicella infection, procedures in perineal region, instrumentation of urethra and hematologic malignancies (1, 2, 5, 11). Acute myeloid leukemia, M4, was the etiology of FG in our case. About 35 cases of FG associated with hematologic malignancies have been reported while about 88% of cases were complications of treatment and in few cases FG was the first sign of hematologic malignancies (12). Simultaneous occurrence of FG and congenital leukemia in neonates is very rare. Immune deficiency caused by leukemia could be the predisposing factor for FG. Lo reported an extensive necrotizing fasciitis in a neonate with AML (13). FG should be considered as the first sign of AML.
The cause of FG can be identified in approximately 95% of cases (1, 11). There are two types of necrotizing fasciitis depending on the responsible organisms. Type 1 is usually polymicrobial including aerobic and anaerobic bacteria. Type 2 is monomicrobial and often caused by group A Streptococcus alone or in combination with Staphylococcus aureus (10). The usual organisms that cause Fournier gangrene in children are streptococci, staphylococci and anaerobes (1). In our patient, blood and wound culture yielded Pseudomonas aeruginosa. Cases of necrotizing fasciitis with Pseudomonas aeruginosa in pediatric patients affected by acute leukemia was reported by some researchers (13). Fustes-Morales et al. described P. aeruginosa as the most common organism isolated in 85% of necrotizing fasciitis cases. Association of P. aeruginosa and necrotizing fasciitis was also demonstrated by Al-Fifi et al. (14) in two cases and Rouzrokh et al. (15) in seven cases. Pseudomonas seems to be an important causative pathogen in neutropenic patients with a rapid and fatal course. Early diagnosis and prompt appropriate treatment is essential in FG. Treatment includes early IV-fluid therapy, hemodynamic stabilization, broad-spectrum antibiotics and surgical debridement of necrotic tissues. Although literature suggest aggressive debridement of wound but a recent study showed successful outcome by using more conservative and selective surgical methods (5). Hyperbaric oxygen is also used in some selected cases for the treatment of Fournier’s gangrene (16). We started with a combination of broad spectrum antibiotics (meropenem and vancomycin) regimen and then modified it to meropenem and amikacin when culture results were available. Our patient was not a surgical candidate for debridement because of coagulopathy state and her poor condition, so we could only wash and keep the wound sterile. Mortality rate of Fournier’s gangrene is ranged from 3 to 45 percent which is mostly due to severe sepsis, renal failure and coagulopathy (9). Despite all the medical and surgical advances in treatment the mortality remains high. We planned to start chemotherapy but the parents refused any type of treatment and the baby was discharged against medical advice.
Neonatal FG is extremely rare and there is a need for high index of suspicion to make the prompt diagnosis and early appropriate treatment. The physicians should consider Leukemia in the differential diagnosis of a newborn with clinical features of sepsis and necrotizing fasciitis.