1. Background
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most common psychiatric disorders in children (1-3). The main symptoms of ADHD include hyperactivity, symptoms must last for 6 months, not match the developmental level of the child, and have appeared before the age of 7 (4, 5). This disorder is 5 folds more common in boys than in girls (6). Stress in family, especially when it is chronic and exists in the early growth period of the child, has harmful effects on the health of the parents and the children as well as the parents' relationship with the child (7). One of the factors related to the characteristics of the family that can cause stress in parents is emotional and behavioral problems in children, the most common of which being ADHD (8).
ADHD is associated with stress and conflict in the family (9). Concerned and watchful parents, especially mothers, can be a source of stress (10). Repeated calls of the parents of the ADHD children with their teacher regarding their children's misbehavior, talking to other parents about their children's behavior, leaving job to care for their hyperactive children, and worrying about the children harming themselves are only a few of the stressors that are commonly reported by the parents of the children with ADHD (11).
Children with behavioral disorders affect the mental health of their parents (12). Studies suggest that maternal depression is associated with behavior problems in children (13). For instance, Swanne and colleagues (2006) reported that 30.62% and 4% of the mothers of the ADHD children had moderate and severe depression, respectively (14). Moreover, dealing with the problems of the ADHD children has a negative impact on the mental health of the parents (15).
Training programs help to improve the parents' mental health. Much evidence indicates that the interaction between the parents and the children and mental health of the parents, especially mothers, are improved when the ADHD children are treated by various methods. Danforth and colleagues showed that various methods of treatment, including medication and parent training, could be effective in improving the maternal mental health (16). Among the educational programs, cognitive behavioral stress management based on four components of increased awareness, assessment, coping resources, and coping reactions, can be a more effective manner in facing the stress and reducing it. Cognitive-behavioral intervention in stress management familiarizes the individuals with stress and coping with it and also neutralizes the stressors' effects and stress responses to help a better physiological and psychological functioning. Intervention can be effective by increasing the sense of control, self-efficacy, self-esteem, adaptive coping, and social support (17).
According to Blumenthal et al. employing stress management techniques improves the individuals' confrontation with stressful situations, increases their control of the physical and emotional states, and consequently improves their health (18).
Despite the impact of children's misbehavior on the mental health of the family members, the importance of the intervention programs in improvement of the mental health of the families of the children with behavioral problems has been neglected (19).
2. Objectives
Therefore, the present study aimed to assess the effect of stress management program using cognitive behavior approach on mental health of the mothers of the children with ADHD.
3. Patients and Methods
This interventional study was performed on 90 mothers of the children with ADHD. The study mothers were randomly assigned to intervention, placebo, and control group. The study population included all the mothers of the ADHD children referring to the psychiatric clinics affiliated to Shiraz University of Medical Sciences in 2012. We selected two psychiatric clinics through random cluster sampling in Shiraz. Cognitive behavioral stress management program consisted of eight 90-minute sessions that were held during 8 weeks. In this study, the participants in the cognitive-behavioral stress management program were placed in four groups of seven or eight mothers who received the same content. In the study, cognitive-behavioral stress management models presented by Antony and colleagues (17) were used. The intervention included needs assessment of the mothers of the children with ADHD, training the mothers about ADHD, understanding stress and its effects, training Benson's relaxation technique, negative thoughts and cognitive distortions, replacing rational thoughts, efficient coping and implementing effective coping responses, anger management, and summary of content. In order to maintain the mothers' attention during the intervention sessions, visual tools, such as Microsoft PowerPoint, graphs, and images associated with hyperactive children, were utilized. The intervention was conducted through lectures, question-and-answer, and group discussions. The first 30 minutes of each session was assigned to summary of the previous session, relaxation techniques, and reviewing homework. The session was continued with new contents, mothers' questions about the new contents, talking about the situations which were related to the upcoming subjects during the session, and new homework. At the end of each session, the mothers were also provided with an educational booklet related to that session.
Stress management program utilizing cognitive behavior approach was conducted by a psychiatrist or psychiatric nurse. The inclusion criteria of the study were obtaining moderate to severe score in depression-anxiety-stress scale, having hyperactive children aging 6 to 12 years, and mothers not suffering from mental illnesses (according to a self-report form). On the other hand, the exclusion criteria of the study were unwillingness to continue participation in the study, having received similar training interventions before the study, mothers who take any medications for mental health problems, mothers who themselves suffer from any medical or mental health problems and the presence of mental or physical illness in a family member that prevents mothers from doing homework at home.
In this study, no intervention was performed in the control group. Besides, the mothers in the placebo group only participated in meetings. In the meetings, they talked about children's behavior and problems at school and home such as low performance in school, repeated calls of the teachers of the ADHD children regarding the children's misbehavior, their resistance in taking medication, lack of support and cooperation of other family members. Also, they expressed feelings about this behavior but did not receive any interventions.
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran. Also, written informed consents were obtained from all the study participants. It should be noted that the participants were informed about the purpose of the study as well as about their right to withdraw at any time. They were also assured that their personal information would remain confidential.
In this study, the data were collected using strength and difficulties questionnaire (parent – report), depression-anxiety-stress scale, and general health questionnaire.
SPSS statistical software (v 18) was used for statistical analysis. At baseline, the socio-demographic characteristics of the three groups were compared using the chi-square test. In addition, inter-group comparisons of the variables were made through one-way ANOVA and Tukey's post-hoc test. Besides, within group comparisons of the variables were made using one-sample repeated measurement ANOVA in the intervention, the placebo and the control groups.
4. Results
A total of 90 mothers completed the study. Overall, 4 participants (two from the intervention group and two from the control group) dropped out before completion of the study for different reasons unrelated to the study. Also, 5 participants in the placebo group dropped out because they realized that the program was useless. The study results revealed no significant difference among the three groups regarding the socio-demographic characteristics. The mean age of the children was 8.85 ± 1.61 years in the intervention group, 8.88 ± 1.62 years in the placebo group, and 9.03 ± 1.60 years in the control group (P < 0.905). Also, no significant difference was found among the three groups concerning the mothers' mean age (33.51 ± 7.00, 34.11 ± 5.36, and 34.59 ± 5.67 years in the intervention, placebo, and control groups, respectively; P < 0.806). Most of the study mothers had high school diploma degrees and 76.5% of the 81 children were boys. In addition, the majority of the mothers in the three groups were housewives and none of the mothers had a history of physical or mental illness.
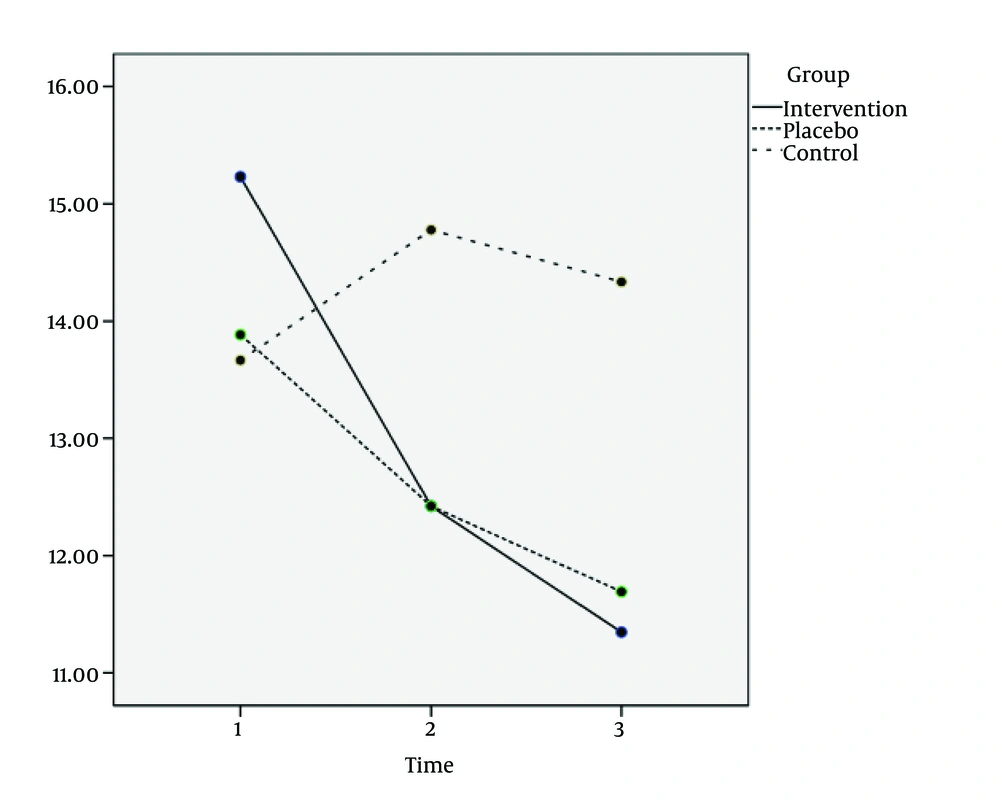
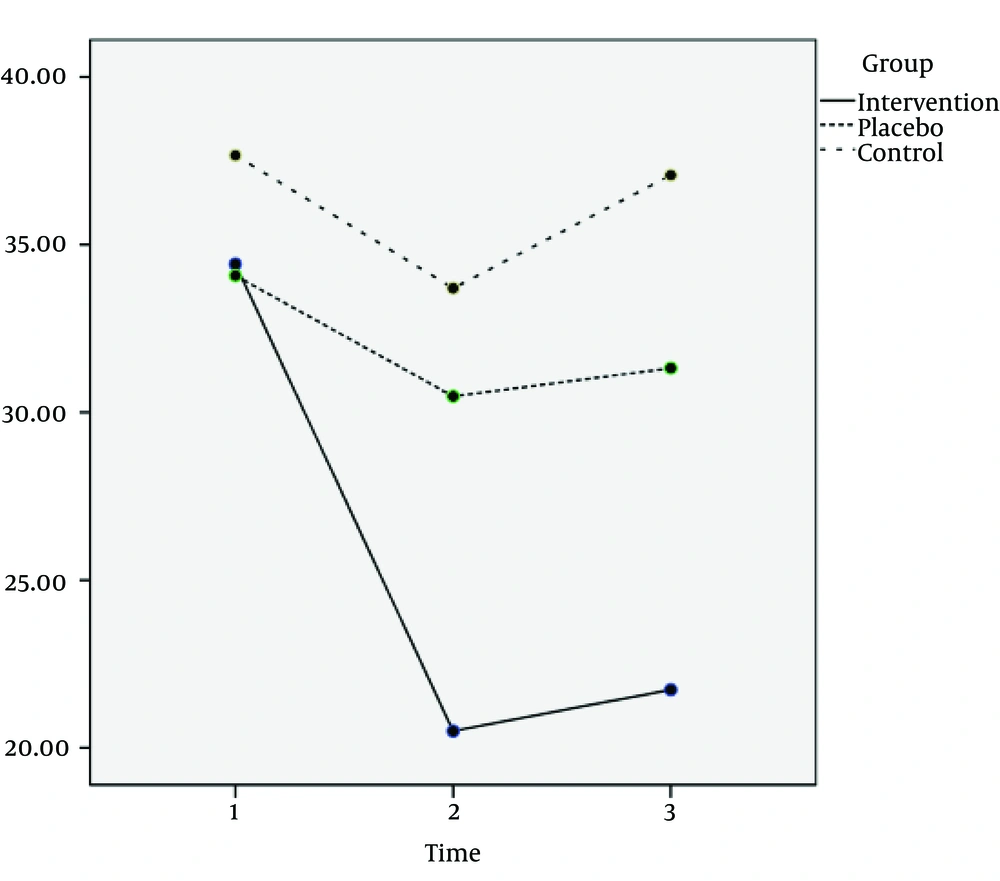
The mean stress and mental health scores in the three groups have been presented in Figures 1 and 2. The mean mental health and depression-anxiety-stress scores in separate groups at baseline, immediately after, and one month after the intervention are shown in Table 1. Also, the mean stress and mental health variables in Tukey's post-hoc test in separate groups immediately after the intervention are shown in Table 1.
Comparisons of the baseline scores of the study variables (stress, anxiety, depression, and mental health) revealed no significant differences among the three groups. However, immediately after, and one month after the completion of the stress management program utilizing cognitive behavioral approach, a statistically significant difference was found among the three groups regarding stress and mental health. The mean score of stress reduced in both intervention and the placebo group, but the mean mental health score improved only in the intervention group. The results of one-way ANOVA showed that the mean score of stress immediately after the intervention was 12.29 ± 4.32 in the intervention group and 12.33 ± 3.75 in the placebo group (P = 0.033).
Also, the mean mental health score was 20.50 ± 10.56 in the intervention group immediately after the intervention (P = 0.001).
One month after intervention, improvement in the mean mental health score was detected only in the intervention group. The results of one-way ANOVA showed that the mean mental health score was 21.73 ± 9.43 in this group (P < 0.001).
The mean anxiety and depression scores were statistically significant in the intervention and the placebo groups. It is shown in Table 1.
Within group comparisons of the variables were performed using one-sample repeated measurement ANOVA in the intervention group. The placebo and the control groups were not changed. The changes in the scores of mental health and depression-anxiety-stress at baseline, immediately after, and one month after the intervention are presented in Table 2.
| Experimental | Times | P Value |
|---|---|---|
| 0-1 | 0.006 | |
| 0-2 | 0.001 | |
| 2-1 | 0.089 | |
| 0-1 | 0.999 | |
| 0-2 | 0.077 | |
| 2-1 | 0.004 | |
| 0-1 | 0.999 | |
| 0-2 | 0.070 | |
| 2-1 | 0.210 | |
| 0-1 | < 0.001 | |
| 0-2 | < 0.001 | |
| 2-1 | 0.999 |
aTime 0, baseline; Time 1, immediately after the intervention; and Time 2, one month after the intervention.
| Variables | Time | Intervention group | Placebo group | Control group | P Value | P Value (post-hoc test) |
|---|---|---|---|---|---|---|
| Stress | ||||||
| 0 | 15.23 ± 3.36 | 13.88 ± 3.21 | 13.66 ± 3.90 | 0.181 | Intervention control: 0.057; Placebo control: 0.067 | |
| 1 | 12.29 ± 4.32 | 12.33 ± 3.75 | 14.77 ± 3.69 | 0.033 | Intervention control: 0.017; Placebo control: 0.040 | |
| 2 | 11.34 ± 4.39 | 11.69 ± 3.51 | 14.33 ± 3.66 | 0.012 | ||
| 0 | 10.22 ± 4.97 | 10.23 ± 4.72 | 11.11 ± 4.22 | 0.700 | Placebo control: 0.014 | |
| 1 | 10.33 ± 4.72 | 9.11 ± 3.53 | 12.25 ± 3.98 | 0.018 | Intervention control: 0.001; Placebo control: 0.006 | |
| 2 | 8.29 ± 4.47 | 8.88 ± 2.84 | 12.35 ± 3.88 | 0.001 | ||
| 0 | 8.14 ± 3.69 | 8.74 ± 3.98 | 8.88 ± 5.56 | 0.815 | Intervention control: < 0.001; Placebo control: 0.001 | |
| 1 | 7.74 ± 4.51 | 7.96 ± 4.44 | 10.37 ± 5.00 | 0.078 | ||
| 2 | 6.59 ± 4.27 | 7.03 ± 4.15 | 11.29 ± 4.25 | < 0.001 | ||
| 0 | 34.42 ± 13.22 | 34.08 ± 15.71 | 37.66 ± 14.64 | 0.484 | Intervention placebo: 0.047; Intervention control: 0.001 | |
| 1 | 20.50 ± 10.56 | 30.48 ± 12.94 | 33.70 ± 12.60 | 0.001 | Intervention placebo: 0.012;Intervention control: < 0.001 | |
| 2 | 21.73 ± 9.43 | 31.32 ± 13.59 | 37.03 ± 11.73 | < 0.001 |
aTime 0, baseline; Time 1, immediately after the intervention; and Time 2, one month after the intervention.
5. Discussion
This study was performed using stress management program utilizing cognitive behavioral approach in three experimental, placebo, and control groups. In fact, elimination of the confounding variables and inclusion of a placebo group are important because any change in the experimental group at the end of the intervention can be attributed to the cognitive behavioral stress management intervention. This study assessed the effect of stress management program using cognitive behavior approach on mental health of the mothers of the children with ADHD. The results of this study showed that cognitive behavioral stress management program in the experimental group led to improvement of mental health immediately and one month after the intervention and reduction of maternal stress immediately after the intervention. Previous studies have been mostly conducted on the relationship between maternal mental health and behavioral problems in the children, stress management training for the parents, and determining the degree of stress, anxiety, and depression in mothers of the ADHD children. The results obtained in these studies are compatible with those of the present one. Musa and Shafiee conducted a study in Malaysia in order to determine depression, anxiety, and stress levels among the mothers of the ADHD children and their relationships with ADHD symptoms. The results of that study showed that compared to the control group, the mothers of the ADHD children experienced higher levels of stress, anxiety, and depression resulting from external behaviors in the children (20). Moreover, Lesesne and colleagues in their study found a relationship between mothers’ mental health and behavioral outcomes in children (13). These results suggest that the mothers of hyperactive children need a comprehensive training to increase their information and awareness about ADHD that can, in turn, create changes in attitude and behavior toward children (21). Also, increase in the parents' information and awareness can reduce the maternal concerns and anxiety and reform the parents' false and dysfunctional beliefs. The reformation eventually paves the way to promote the mothers mental and social health (22). Although perception and acceptance of the characteristics and behaviors of the children are hard by mothers, they can more easily explain their children's behavior after participation in the training sessions. Consequently, behavior problems in the children are reduced, the children will obey the maternal orders more, and the mothers will feel less under pressure and stress (21).
Furthermore, the findings of studies have pointed out that the parents' training programs can be effective in improving the relationship between the parents and their ADHD children. Up to now, studies have used different training programs to increase the knowledge and awareness of the mothers of hyperactive children. Prithivirajh and Edwards recommended stress management program for the parents of the ADHD children. The results of their study showed that stress management program helped the parents of hyperactive children as a valuable adjunctive strategy in the overall comprehensive management of ADHD (23).
Regarding the effect of training on mental health of mothers of ADHD children, the results of the present study are in agreement with those of the previous ones. Meftagh and colleagues carried out a research on 95 mothers to determine the effectiveness of different treatment methods for children with ADHD on maternal mental health. That study indicated that maternal behavioral training methods and the medications used for these children improved maternal mental health in post-test and follow-up stages (24). Moreover, Parand and colleagues performed a study which aimed to develop a stress management program for mothers of the children with ADHD and determine its effectiveness in their mental health. The results revealed significant improvement in mental wellbeing of the mothers and diminishing their anxiety and depression (19).
The findings of the current study showed a reduction in stress levels in the placebo group immediately and one month after the intervention. The observed reduction might have resulted from participation in the meetings for talking about and expression of feelings. In addition, the loss rate in the placebo group was higher compared to the other two groups since they believed that expressing their feelings would not lead to any improvement. In the control group, no significant changes were observed regarding mental health and stress, anxiety and depression.
5.1. Limitation
This study had some limitations. First of all, the sample size was relatively small because of inclusion of three groups and lack of facilities. Thus, further studies with three groups and larger sample size are required to confirm the results of this study. Also, the studies are suggested to have follow-up periods of more than 1 month and be repeated over time.
The findings of the present study showed the effectiveness of cognitive behavioral stress management intervention in improvement of the mothers' mental health and stress.
Nonetheless, further studies with longer follow-up periods and in the mothers who have more than one ADHD child are suggested to be done in this area.