Fulltext
A 5 year old boy was admitted due to insidious onset of fever, lethargy, malaise and oral lesions from 20 days ago and then lost consciousness and had two generalized tonic-clonic seizures after hospitalization in ICU. The cerebrospinal fluid (CSF) and blood evaluation was not remarkable except for triglyceride 243 mg/dl, cholesterol 264 mg/dl and lactate de-hydoganse 641 mg/dl, blood and CSF lactate was normal.
Brain MRI showed diffuse bilateral basal ganglia involvement (Fig. 1). After discharge the patient had sequels of the disease as spasticity, loss of speech, generalized dystonia, and difficulty in sucking and swallowing.
Brain MRI one month later showed that involvement of the basal ganglia was increased and clinical signs and symptoms had not changed.
What is the best diagnosis?
A) Bilateral striatal necrosis
B) Wilson disease
C) Leigh’s disease
D) Glutaric aciduria type 1
Remarks
Most disorders of mitochondrial function will cause lesions in the basal ganglia. Leigh’s syndrome typically causes a speckled pattern indeep nuclei but in this patient CSF lactate was not elevated and involvement progress of basal ganglia elucidated over one month[1].
In Wilson disease signal changes in basal ganglia is seen most often secondary to hepatic failure. Abnormal MRI findings are bilateral high-signal, T2-weighted abnormalities in the basal ganglia (particularly putamen, caudate head, ventral thalamus, dentate nucleus of the brainstem and cerebellum, and atrophy of the cortex and cerebral white matter. in this patient,
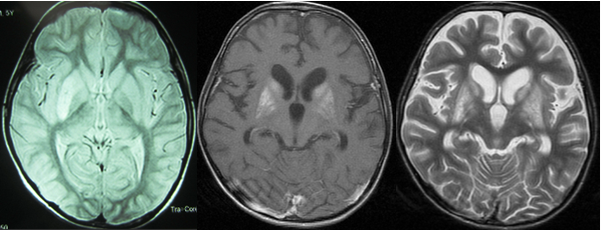
Fig. 1: (Left) first Axial T2WI imaging shows hyperintensity in right putamen nucleus. (Middle and right): Axial FLAIR and T2WI imaging, respectedly, after one month, show bilateral symmetrical hyperintensities in caudates, putamina and globi pallid nuclei at the same patient.
hepatic failure was not seen and the patient’s age was not typical for neurologic presentation of Wilson disease.
In glutaric aciduria type 1 imaging findings include fronto-temporal atrophy and dilatation of Sylvian fissures (bat wing sign) and in T2WI and FLAIR increased signal in caudate/putamina >globus pallidus are seen. In this patient, we did not find bat wing sign and macrocephally.
Symmetric basal ganglia involvement is a pathognomonic neuroimaging finding of some neurometabolic disorders, especially mito-chondrial and organic acidemia. Infantile bilateral striatal necrosis should be considered in differential diagnosis when biochemical study of neurometabolic disorders was not remarkable.
Infantile bilateral striatal necrosis (IBSN) presents phenotypically as three clinical syndromes. One form has insidious onset and most of these cases have mitochondrial disorders. The second form presents as an acute encephalopathy and usually following a febrile illness with nausea and vomiting. The main features are dystonia and tremor. Some patients recover spontaneously and others have permanently sequels. The presentation of the patient is compatible with this form[3].
The third form starts usually between 3 and 5 years of age. The first symptoms are confusion, dysarthria, and dysphagia. Dystonia, rigidity, cranial nerve palsies, and quadriparesis may follow the initial presentations.
Correct Answer: A