1. Background
Poor nutritional status during infancy and in utero has effects on health outcomes and susceptibility to chronic diseases during adulthood (1-4). Growth monitoring is a critical component of the medical and nutritional evaluation of infants. Growth charts mainly belong to two types: growth standards and growth references. The latter explains how children are growing instead of how they should be, it is represented by standard charts (5, 6). Studies have revealed that both nutritional status and genetic diversity may influence an infant’s growth pattern. Growth assessment in children can be improved by considering the ethnic variations. Thus using a reference growth chart to evaluate children from different populations and different ethnicities seems to be inaccurate. In line with this, several studies assessed the nutritional status of children in different ethnicities. Some studies reported the growth patterns to be more affected by environmental factors such as diet and health services rather than genetic background (7). Nguyen et al. demonstrated that growth pattern of infants with Vietnamese immigrant parents residing in Australia was nearly similar to those in the United States (8). Comparing growth curves from the US, France, the United Kingdom, Netherlands and Belgium with World Health Organization (WHO) standards revealed that during the first 3 months of life, depicted values for length, weight and body mass index (BMI) in growth reference curves were considerably lower than WHO standards. However, after the age of 6 months, growth indices were reversely higher in growth reference curves (9).
Interpreting children’s growth pattern is a critical step in assessing their health status, subsequently if growth charts were adjusted for ethnicity and nationality, the assessment would have been more accurate. Although WHO growth standards were comprised based on data from different populations it did not encompass information about premature and very low birth weight infants (less than 1.5 kg); the growth pattern of these infants is different from term infants (10). Alternative charts to evaluate growth of preterm and low birth weight infants are: Fenton’s for following growth from weeks 22 of gestational age (GA) to week 10 of post-term (11), and the infant health and development program charts for evaluating growth from two months to 38 months (12). In Iran, Fenton growth chart is used to track growth of newborn babies whether term, preterm or very low birth weight. Therefore, the aim of the current study was to present a revised version of infancy’s growth chart based on Iranian newborns in a large population.
2. Methods
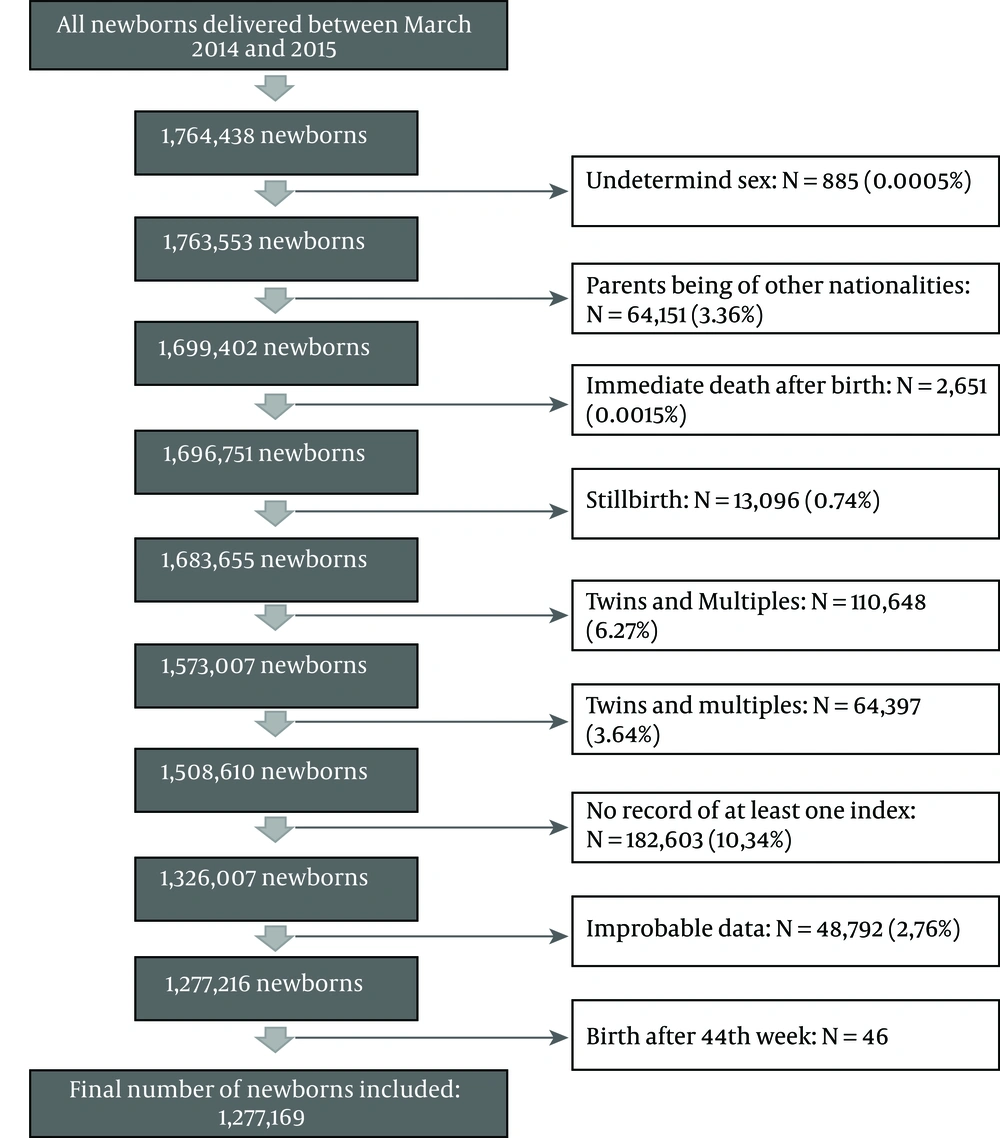
Data of all neonates delivered between March 2014 and March 2015 was collected from Iranian national data centre, ministry of health. Totally, 1.764.438 infants were registered. Birth weight (g), length (cm), head circumference (cm) and sex were recorded by a midwife immediately after birth. Information regarding nationality was also registered. Those with Iranian nationality were included in the study. Other inclusion criteria were singleton boys and girls and term, preterm and post-term delivered infants. Exclusion criteria were stillbirth, congenital anomalies such as neural tube defects (NTDs) and multiple births. Finally, anthropometric data of 1.277.169 (72%) infants were used for analysis (Figure 1).
2.1. Statistical Analysis
To control for errors in measurement and recording data extreme outliers were computed. In previous similar studies, extreme outliers were defined as values 2 times the interquartile range (25th to 75th percentiles) below the first quartile and above the third quartile for each GA (13). Consequently, infants with physiologically improbable growth measurements (“extreme outliers”) were excluded from the gender-specific samples.
Centiles were analyzed by three methods. The first method was LMS (lambda, mu, sigma) method which performs the Box-Cox power transformation to evaluate normally distributed data in a group, for this purpose three values for gestational age groups were estimated i.e. L the power transformation performed to get normality, M the median of birth weight and S the coefficient of data variation. For all gestational ages the L, M and S variables are evaluated. The second performed model was LMST (i.e. lambda, mu, sigma, assuming Box-Cox t distribution) method, which takes into account skewness and leptokurtosis; and third one, LMSP (lambda, mu, sigma, assuming Box-Cox power exponential distribution) method, considers skewness, platykurtosis, and leptokurtosis. The LMST and LMSP methods are extensions of the LMS method. LMS method allows for scale, location and skewness but not for kurtosis in the data.
We used the Akaike information criterion and Bayesian information criterion to compare models within and between different classes of models to explore the best model. Analysis was performed by using the gamlss package under R.3.0.1 software.
3. Results
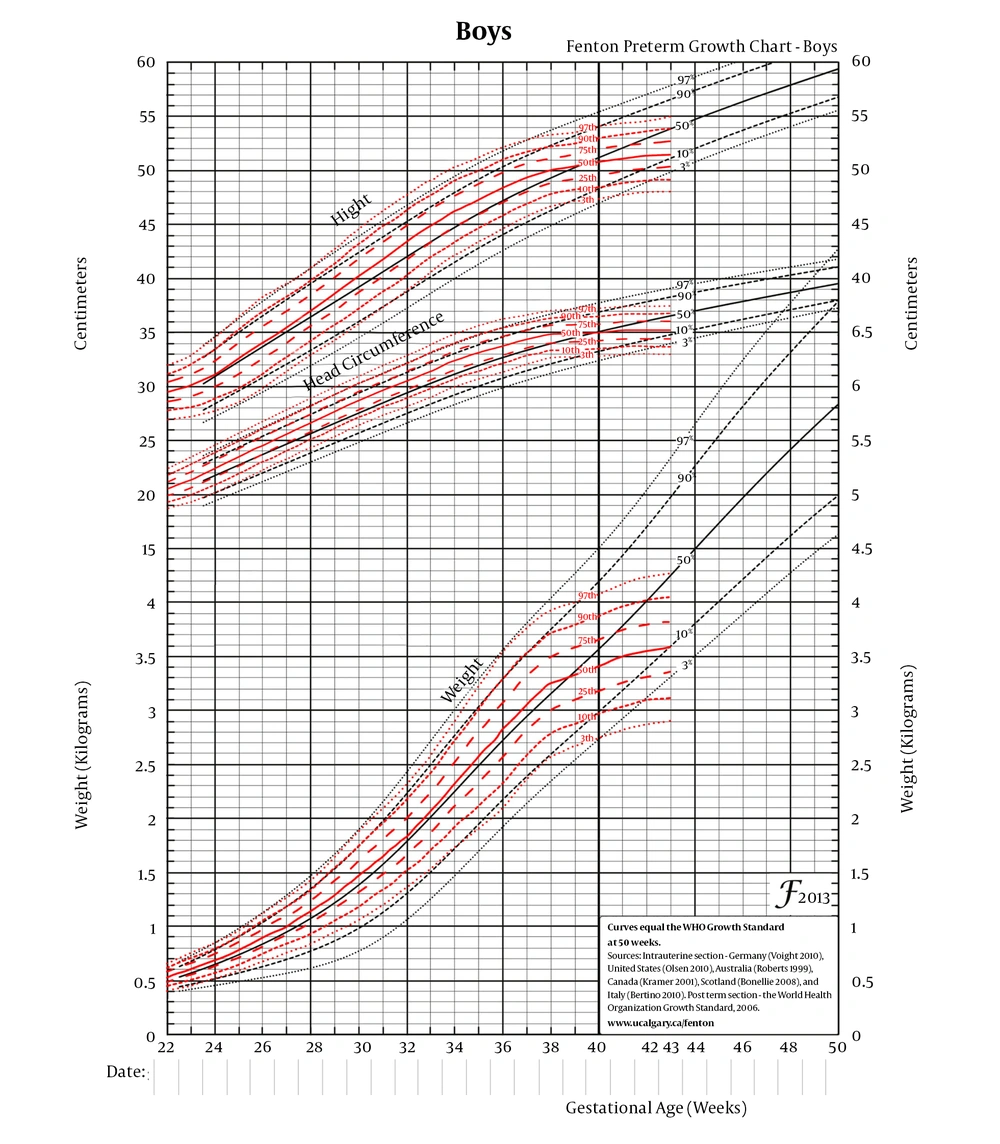
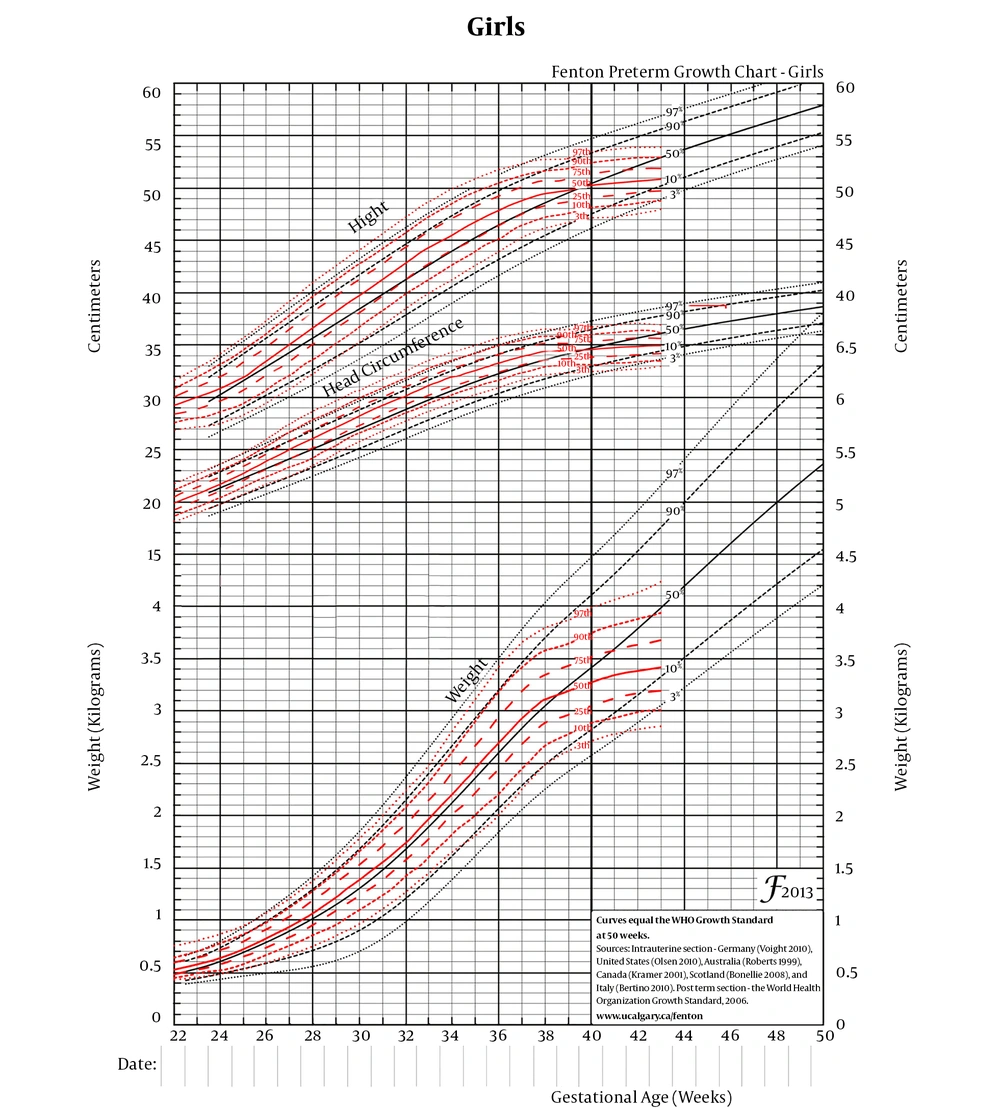
There were 1.764.438 births during the study period (2014 - 2015). 450.991 infants were excluded due to stillbirth 13.096, congenital anomalies 64.397, multiple births 110.648, non-Iranian nationality 64.151, incomplete data 185.603 and infants died before discharge 13.096. A total number of 48.792 of the observations were omitted as outliers. Finally, 1.277.169 infants were introduced to analysis according to the inclusion criteria. Of the eligible infants, 661.507 (51.79%) infants were male and 615.662 (48.2%) were female. The GA was estimated 38.5 ± 1 weeks. Tables 1 and 2 show the mean birth weight, length, and head circumference of Iranian neonates according to criteria of this study. The mean birth weight in total population was 3242 ± 422 g and 3125 ± 422 g for boys and girls respectively. Length at birth was 50 ± 2.2 cm and 49.5 ± 1.2 cm for boys and girls, and mean data for head circumference was reported 35 ± 1.4 cm and 34.2 ± 2.3 cm respectively for studied boys and girls. Similar to weight, mean height was increased by age. The differences of length betweenceoss genders were reported in some weeks. We also found that female newborns had lower weight, length and head circumference in comparison to male newborns. The data for both sexes were reported separately in different centiles because the gender differences were significantly different. Smoothed curves of birth weight, length, and head circumference for a large sample size of Iranian boys and girls are presented in Figures 2 and 3. We plotted height-for-age, weight-for-age and head circumference–for-age curves in eligible newly born girls and boys delivered during 2014 - 2015 in the third, 10th, 25th, 50th, 90th, and 97th percentiles.
| Birth Week | N | Weight | Length | Head Circumference | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | 10 | 25 | 50 | 75 | 90 | 97 | 3 | 10 | 25 | 50 | 75 | 90 | 97 | 3 | 10 | 25 | 50 | 75 | 90 | 97 | ||
| 22 | 107 | 401 | 441 | 482 | 527 | 572 | 613 | 653 | 27 | 7/27 | 5/28 | 4/29 | 3/30 | 1/31 | 9/31 | 7/18 | 3/19 | 9/19 | 5/20 | 1/21 | 7/21 | 3/22 |
| 23 | 95 | 449 | 497 | 545 | 598 | 651 | 699 | 747 | 2/27 | 1/28 | 29 | 30 | 31 | 9/31 | 8/32 | 3/19 | 20 | 6/20 | 3/21 | 22 | 7/22 | 3/23 |
| 24 | 133 | 507 | 561 | 615 | 676 | 737 | 792 | 846 | 7/27 | 8/28 | 8/29 | 31 | 2/32 | 3/33 | 3/34 | 2/20 | 9/20 | 6/21 | 3/22 | 1/23 | 8/23 | 5/24 |
| 25 | 191 | 575 | 636 | 697 | 765 | 833 | 895 | 955 | 5/28 | 7/29 | 31 | 4/32 | 8/33 | 1/35 | 3/36 | 2/21 | 9/21 | 6/22 | 4/23 | 1/24 | 8/24 | 5/25 |
| 26 | 266 | 663 | 732 | 802 | 880 | 958 | 1029 | 1098 | 7/29 | 31 | 4/32 | 9/33 | 4/35 | 8/36 | 1/38 | 2/22 | 9/22 | 6/23 | 4/24 | 1/25 | 9/25 | 6/26 |
| 27 | 271 | 743 | 821 | 905 | 995 | 1086 | 1168 | 1248 | 3/31 | 7/32 | 34 | 4/35 | 9/36 | 2/38 | 5/39 | 2/23 | 9/23 | 6/24 | 4/25 | 2/26 | 9/26 | 7/27 |
| 28 | 469 | 827 | 921 | 1016 | 1122 | 1228 | 1323 | 1418 | 9/32 | 2/34 | 5/35 | 9/36 | 3/38 | 6/39 | 9/40 | 2/24 | 9/24 | 7/25 | 5/26 | 3/27 | 28 | 8/28 |
| 29 | 475 | 929 | 1041 | 1154 | 1279 | 1405 | 1518 | 1630 | 2/34 | 5/35 | 9/36 | 4/38 | 9/39 | 3/41 | 6/42 | 2/25 | 9/25 | 7/26 | 5/27 | 3/28 | 1/29 | 8/29 |
| 30 | 793 | 1040 | 1170 | 1302 | 1448 | 1594 | 1726 | 1856 | 7/35 | 1/37 | 5/38 | 40 | 6/41 | 43 | 4/44 | 3/26 | 27 | 7/27 | 6/28 | 4/29 | 1/30 | 8/30 |
| 31 | 943 | 1174 | 1317 | 1462 | 1624 | 1785 | 1931 | 2074 | 1/37 | 6/38 | 40 | 6/41 | 2/43 | 7/44 | 1/46 | 2/27 | 9/27 | 7/28 | 5/29 | 3/30 | 1/31 | 8/31 |
| 32 | 1777 | 1338 | 1491 | 1646 | 1818 | 1990 | 2145 | 2298 | 7/38 | 1/40 | 5/41 | 1/43 | 7/44 | 1/46 | 6/47 | 28 | 8/28 | 6/29 | 4/30 | 3/31 | 32 | 8/32 |
| 33 | 2538 | 1519 | 1684 | 1851 | 2037 | 2223 | 2390 | 2555 | 4/40 | 9/41 | 1/43 | 7/44 | 2/46 | 6/47 | 49 | 9/28 | 7/29 | 5/30 | 3/31 | 2/32 | 33 | 8/33 |
| 34 | 4974 | 1710 | 1892 | 2077 | 2283 | 2488 | 2673 | 2856 | 42 | 3/43 | 7/44 | 1/46 | 6/47 | 9/48 | 2/50 | 8/29 | 6/30 | 4/31 | 2/32 | 1/33 | 9/33 | 7/34 |
| 35 | 9172 | 1886 | 2093 | 1203 | 2536 | 2770 | 2980 | 3187 | 3/43 | 6/44 | 8/45 | 2/47 | 6/48 | 9/49 | 1/51 | 6/30 | 4/31 | 1/32 | 33 | 9/33 | 7/34 | 5/35 |
| 36 | 19757 | 2071 | 2298 | 2528 | 2784 | 3039 | 3269 | 3496 | 5/44 | 7/45 | 9/46 | 3/48 | 7/49 | 9/50 | 1/52 | 2/31 | 32 | 8/32 | 7/33 | 6/34 | 4/35 | 1/36 |
| 37 | 52274 | 2332 | 2556 | 2782 | 3034 | 3286 | 3512 | 3736 | 7/45 | 8/46 | 9/49 | 2/49 | 5/50 | 6/51 | 8/52 | 32 | 7/32 | 4/33 | 2/34 | 35 | 8/35 | 5/36 |
| 38 | 209585 | 2558 | 2774 | 2993 | 3236 | 3479 | 3698 | 3913 | 7/46 | 7/47 | 8/48 | 9/49 | 1/51 | 2/52 | 2/53 | 6/32 | 3/33 | 34 | 8/34 | 6/35 | 3/36 | 37 |
| 39 | 196064 | 2662 | 2873 | 3087 | 3325 | 3562 | 3776 | 3987 | 1/47 | 4/48 | 1/49 | 3/50 | 4/51 | 4/52 | 4/53 | 6/32 | 3/33 | 1/34 | 8/34 | 6/35 | 3/36 | 1/37 |
| 40 | 135168 | 2734 | 2947 | 3164 | 3404 | 3644 | 3861 | 4074 | 3/47 | 8/48 | 5/49 | 7/50 | 9/51 | 53 | 54 | 7/32 | 4/33 | 1/34 | 9/34 | 7/35 | 4/36 | 1/37 |
| 41 | 24752 | 2820 | 3035 | 3252 | 3494 | 3736 | 3953 | 4168 | 7/47 | 4/48 | 8/49 | 51 | 3/54 | 2/53 | 3/54 | 9/32 | 6/33 | 3/34 | 1/35 | 9/35 | 6/36 | 3/37 |
| 42 | 1607 | 2871 | 3287 | 3305 | 3548 | 3791 | 4010 | 4226 | 47/6 | 5/48 | 50/1 | 51/1 | 6/54 | 53/4 | 7/54 | 9/32 | 6/33 | 4/34 | 1/35 | 9/35 | 6/36 | 4/37 |
| 43 | 96 | 2903 | 3118 | 3336 | 3579 | 3821 | 4039 | 4255 | 47/4 | 4/48 | 50/2 | 51/2 | 8/54 | 53/5 | 55 | 9/32 | 6/33 | 3/34 | 1/35 | 36 | 7/36 | 4/37 |
| Birth Week | N | Weight | Length | Head Circumference | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | 10 | 25 | 50 | 75 | 90 | 97 | 3 | 10 | 25 | 50 | 75 | 90 | 97 | 3 | 10 | 25 | 50 | 75 | 90 | 97 | ||
| 22 | 57 | 437 | 459 | 486 | 524 | 576 | 644 | 753 | 8/26 | 5/27 | 3/28 | 1/29 | 9/29 | 7/30 | 5/31 | 18 | 6/18 | 2/19 | 8/19 | 5/20 | 21 | 6/23 |
| 23 | 95 | 463 | 493 | 528 | 576 | 637 | 709 | 803 | 1/27 | 28 | 9/28 | 9/29 | 9/30 | 8/31 | 7/32 | 9/18 | 5/19 | 1/20 | 7/20 | 4/21 | 22 | 6/22 |
| 24 | 120 | 492 | 532 | 579 | 638 | 706 | 777 | 859 | 4/27 | 5/28 | 5/29 | 7/30 | 9/31 | 9/32 | 34 | 7/19 | 3/20 | 21 | 6/21 | 3/22 | 9/22 | 5/23 |
| 25 | 124 | 534 | 588 | 647 | 717 | 792 | 865 | 941 | 2/28 | 4/29 | 5/30 | 8/31 | 1/33 | 3/34 | 5/35 | 7/20 | 3/21 | 22 | 6/22 | 3/23 | 24 | 6/24 |
| 26 | 209 | 592 | 661 | 733 | 815 | 899 | 977 | 1055 | 3/29 | 6/30 | 9/31 | 2/33 | 7/34 | 9/35 | 2/37 | 7/21 | 3/22 | 23 | 7/23 | 5/24 | 2/25 | 8/25 |
| 27 | 250 | 664 | 748 | 834 | 931 | 1028 | 1115 | 1202 | 7/30 | 32 | 4/33 | 9/34 | 4/36 | 7/37 | 1/39 | 4/22 | 2/23 | 24 | 9/24 | 7/25 | 5/26 | 3/27 |
| 28 | 415 | 743 | 854 | 947 | 1059 | 1171 | 1271 | 1370 | 1/32 | 5/33 | 9/34 | 5/36 | 38 | 4/39 | 8/40 | 3/23 | 1/24 | 25 | 9/25 | 9/26 | 7/27 | 6/28 |
| 29 | 419 | 841 | 959 | 1078 | 1207 | 1335 | 1448 | 1559 | 6/33 | 35 | 5/36 | 38 | 6/39 | 41 | 4/42 | 5/24 | 3/25 | 1/26 | 27 | 9/27 | 7/28 | 5/29 |
| 30 | 719 | 959 | 1093 | 1226 | 1372 | 1517 | 1645 | 1770 | 1/35 | 5/36 | 38 | 6/39 | 1/41 | 6/42 | 44 | 7/25 | 4/26 | 2/27 | 1/28 | 29 | 8/29 | 5/30 |
| 31 | 804 | 1094 | 1239 | 1384 | 1544 | 1703 | 1845 | 1984 | 7/36 | 1/38 | 5/39 | 41 | 6/42 | 44 | 4/45 | 7/26 | 5/27 | 3/28 | 1/29 | 30 | 8/30 | 6/31 |
| 32 | 1389 | 1261 | 1410 | 1562 | 1732 | 1902 | 2056 | 2209 | 3/38 | 7/39 | 1/41 | 6/42 | 2/44 | 6/45 | 47 | 7/27 | 4/28 | 2/29 | 1/30 | 9/30 | 7/31 | 4/32 |
| 33 | 2123 | 1454 | 1606 | 1765 | 1945 | 2130 | 2301 | 2473 | 8/39 | 2/41 | 6/42 | 2/44 | 7/45 | 1/47 | 5/48 | 6/28 | 4/29 | 1/30 | 31 | 9/31 | 7/32 | 5/33 |
| 34 | 4090 | 1637 | 1804 | 1979 | 2179 | 2386 | 2577 | 2771 | 2/41 | 5/42 | 9/43 | 5/45 | 47 | 4/48 | 8/49 | 4/29 | 2/30 | 31 | 5/32 | 7/32 | 5/33 | 2/34 |
| 35 | 7193 | 1801 | 1993 | 2193 | 2421 | 2654 | 2869 | 3085 | 5/42 | 9/43 | 2/45 | 7/46 | 2/48 | 5/49 | 8/50 | 1/30 | 9/30 | 6/31 | 2/33 | 3/33 | 1/34 | 8/34 |
| 36 | 17005 | 1982 | 2193 | 2412 | 2661 | 2919 | 3151 | 3387 | 8/43 | 1/45 | 3/46 | 7/47 | 1/49 | 4/50 | 7/51 | 8/30 | 6/31 | 3/32 | 8/33 | 34 | 8/34 | 6/35 |
| 37 | 47161 | 2227 | 2438 | 2657 | 2907 | 3163 | 3399 | 3637 | 1/45 | 3/46 | 4/47 | 7/48 | 50 | 1/51 | 3/52 | 6/31 | 3/32 | 33 | 3/34 | 7/34 | 4/35 | 1/36 |
| 38 | 194542 | 2478 | 2668 | 2868 | 3099 | 3341 | 3566 | 3797 | 1/46 | 2/47 | 2/48 | 4/49 | 6/50 | 7/51 | 7/52 | 1/32 | 8/32 | 5/33 | 4/34 | 1/35 | 8/35 | 5/36 |
| 39 | 182561 | 2605 | 2775 | 2958 | 3176 | 3408 | 3632 | 3867 | 6/46 | 6/47 | 6/48 | 7/49 | 8/50 | 8/51 | 8/52 | 4/32 | 33 | 7/33 | 5/34 | 1/35 | 8/35 | 4/36 |
| 40 | 130169 | 2703 | 2866 | 3045 | 3262 | 3501 | 3737 | 3992 | 1/47 | 1/48 | 1/49 | 2/50 | 4/51 | 4/52 | 4/53 | 4/32 | 1/33 | 8/33 | 5/34 | 3/35 | 36 | 7/36 |
| 41 | 24516 | 2771 | 2933 | 3113 | 3332 | 3574 | 3815 | 4078 | 2/47 | 2/48 | 3/49 | 4/50 | 6/51 | 6/52 | 7/53 | 5/32 | 2/33 | 9/33 | 7/34 | 5/35 | 1/36 | 8/36 |
| 42 | 1614 | 2821 | 2982 | 3161 | 3381 | 3628 | 3876 | 4149 | 5/47 | 5/48 | 5/49 | 6/50 | 8/51 | 8/52 | 8/53 | 6/32 | 3/33 | 34 | 8/34 | 6/35 | 3/36 | 37 |
| 43 | 87 | 2845 | 3004 | 3183 | 3408 | 3666 | 3933 | 4235 | 9/47 | 8/48 | 8/49 | 8/50 | 9/51 | 9/52 | 8/53 | 9/32 | 5/33 | 1/34 | 9/34 | 6/35 | 2/36 | 9/36 |
3.1. Comparing Male Growth Chart with Fenton Growth Chart
For GA up to 39 weeks, the average birth weight in third percentile of studied population was strikingly higher than third percentile of Fenton curve (even more than 10th percentile of Fenton curve). Nearly the same trend was observed in 10th percentile. GA 22 - 39 weeks in 50th centile presented a higher mean birth weight than Fenton curve. However the 90th and 97th percentiles of Iranian growth chart were placed subjacent to the same curves in Fenton charts (Figure 2).
GA 22 - 39 weeks showed higher head circumference in our study compared with Fenton curve. In addition, similar trend was observed for 10th percentile. Mean of head circumferences among 50th percentile of Fenton curve was equal to 25th percentile of our population.
Third, 10th and 50th percentiles of body length at birth in our study were higher than the same curves in Fenton chart although body length in 90th and 97th percentiles would be less than Fenton chart after GA 37 and 36 respectively.
3.2. Comparing Female Growth Chart with Fenton Curves
We also revealed differences between Iranian girl growth chart and Fenton chart. Data showed that 3rd and 10th percentiles of birth weight in GA 41 and 40 weeks were higher than those in Fenton curves and declined in later weeks. Similarly, 50th and 90th percentiles showed the same trend. However, mean birth weight was less than Fenton curve in 97th percentile in all gestational ages (Figure 3).
A similar trend of variations in length and head circumference was observed between our chart and Fenton’s. However, the mean head circumference in Iranian babies was the same as Fenton chart for 75th percentile.
4. Discussion
The aim of this study was to construct a reference growth chart for Iranian neonates using anthropometric indices of growth in a large sample and to compare this growth chart with Fenton charts frequently used by Iranian pediatricians. Our research goal was: a) to examine the available collected data of newborns across the country for accuracy and applicability to draw reference growth charts; and b) if there are any differences between our reference growth charts and well-established Fenton growth charts to find out what they are attributed to.
These are our main findings:
i. A significant difference between two sexes was observed with all growth indices being larger in male newborns.
ii. In comparison to Fenton’s growth chart, small values (3rd, 10th) were considerably larger in our plot and large values (90th, 97th) were larger in Fenton growth chart, this trend was observed almost similarly in all growth parameters.
iii. A plain decline in our plot’s trajectories were seen after GA week 38, consistent with all growth indices in both sexes and in contrast to Fenton’s reference curves.
Data related to birth weight, length and head circumference were extracted from a national data center and consequently there was no prospective methodology to control for measurement errors unlike the WHO multicenter growth reference study (MGRS) (14, 15). Yet there are reasons that support the validity and reliability of our results. First, we recruited a considerably large sample of newborn infants to reduce random errors, second we implemented a criterion to exclude extreme values probably produced by errors in measurement and recording, third we compared our results to Fenton growth charts that are based on studies with similar methodology to ours (16).
As reported in a previous study GA, gender and ethnicity have influence on growth parameters (17); consistently we found a gradual increase in growth parameters with GA and a significant sex difference with male neonates having larger values for birth weight, length, and head circumference. A growing body of evidence demonstrated the influence of ethnicity and nationality on infant growth parameters. Thomas et al speculated that relying on growth curves, not been adjusted for ethnicity and sex, may lead to inaccurate estimate of GA (17). In line with this, another study compared birth weight between infants of Asian immigrant parents with infants of white American parents, their results were suggestive of influence of ethnicity and nationality on birth weight (18).
Fenton’s growth chart has been widely used as a reference for evaluating newborn infants, especially preterm neonates admitted to NICU. We compared our growth chart with Fenton’s and found a considerable difference between all growth parameters, more prominent in smaller values (3rd, 10th). It may be argued that observed difference may be due to inaccurate measurements, as we did not control the measurement process. There is little known about the accuracy of weight and height measurements in child health records, yet a previous study that addressed the issue had found no systematic bias in routinely collected child health records other than a slightly overestimation of heights in tall children and underestimation in short children (19) which is in contrast to our findings, we found larger values for lower percentiles (3rd, 10th) and smaller values for higher percentiles (90th, 97th). Although there is no definite evidence to defy the role of systematic bias in our results it seems unlikely to have influenced them majorly.
Another reason for observed differences may be that unequal environmental factors have caused the divergence in growth patterns (20) because Fenton’s growth chart is indicator of an intra-uterine growth status, while our data were from born infants; however, since we implemented a cross-sectional study, not a longitudinal one and sizes of infants were measured right after birth, such an effect seems improbable.
We also found a decline in growth curves after week 38, consistent in all parameters and both sexes. This observation maybe intrinsic to current fetal-infant growth references, particularly Fenton’s, as a growth disjuncture is obvious around week 40 gestation overlapping where the fetal and infant growth references are combined (21, 22). It may also be suggestive of restrictive effects of factors affecting Iranian mothers and/or their fetuses in last months of pregnancy, preventing infants to reach their optimum growth. Further studies are necessary to investigate this possibility.
Finally, we think that observed differences between our growth chart and Fenton’s are valid and can be attributed to ethnicity and socioeconomic factors e.g. nutrition. Because reference curves are important tools for both clinicians and epidemiologists to assess individual/ society’s health status, they should be developed as accurate as possible; hence we encourage further similar studies in Iranian population to establish national growth reference curves.
4.1. Conclusions
In conclusion, we observed differences between age-gender specific growth chart in Iranian newborn infants with Fenton growth chart that may be attributed to the ethnicity, regional and socioeconomic factors, mother-fetus health and nutrition status during pregnancy. Because growth reference curves have been used to assess health status of each individual in clinical practice or societies in epidemiologic studies these observed variations between our results and Fenton’s reference curves should highlight the importance of creating growth reference curves for Iranian newborn infants in particular and Iranian children in general.
4.2. Limitations
One limitation of the current study was the discrepancy in measurements, which might have caused systematic bias, but was inevitable in this project as we used a considerably large sample. In addition, there was no record of the method used for assessing gestational age (nor documentation of the last menstrual period (LMP) neither early ultrasound results) in birth certificates collected in National Data Centre of Ministry of Health. At last our data was related to a short period during 2014-2015 and our study was cross sectional, therefore we suggest further, particularly longitudinal, studies and beyond fetal-neonatal period.