1. Background
Clonal proliferation of histiocytes was reported in Langerhans cell histiocytosis (LCH) by Willman et al. in 1994 (1). Langerhans cells are a type of nonlymphoid mononuclear cells involved in inflammatory responses and also in neoplastic processes. They are immature dendritic cells which express lysosomal enzymes CD1a and S-100 protein and ultrastructurally contain racket shaped organelles of Birbeck granules (2).
The etiology is unknown; however, environmental agents and viruses, especially epstein-barr virus (EBV), or vaccination, have been proposed to play a role in the pathogenesis of LCH (3, 4). The role of EBV as the etiologic agent of several malignancies is known and herpes viruses are shown to be responsible for persistent infection (5, 6). In addition, EBV and cytomegalovirus (CMV) are considered to be responsible for hemophagocytic syndromes in human with several inherited immunodeficiencies (7, 8). One study showed 30% positivity for CMV in LCH (9); however, others have failed to show any association with adenovirus, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, human herpes virus type 6, human immunodeficiency virus, human T-cell leukemia virus types I and II, and parvovirus using PCR (10-12).
2. Objectives
In this study, we have investigated the presence of CMV in LCH by qualitative PCR method. Our study is the first study performed on this subject in Iranian children.
3. Patients and Methods
3.1. Patients and Controls
Formalin-fixed, paraffin-embedded (FFPE) tissue samples of 30 patients with pathologic diagnosis of LCH were extracted from archive of pathology department of Mofid children’s hospital in Tehran (one of the referral centers from all over the country) for a ten year period (2002 to 2012). The diagnosis of LCH was made by a pediatric pathologist, using the histological criteria mentioned in the pathology textbooks, i.e. granulomas composed of Langerhans cells with typical grooved nuclei mixed with eosinophils and other inflammatory cells. The diagnoses were confirmed using immunohistochemical technique for CD1a, S-100 protein and CD68 when available. All patients were Iranian and the age ranged between 2 months and 10 years. Thirty tissue samples with non LCH diagnoses were also selected (between the years 2002 and 2012) as age and site-matched controls to LCH cases.
3.2. Nucleic Acid Extraction
Paraffin was removed from the FFPE samples after undergoing xylene treatment, followed by two washes with pure ethanol. Total DNA was extracted from the air-dried pellet tissues according to the RTP® DNA/RNA virus mini kit procedure (Stratec molecular, Berlin, Germany). The extracted nucleic acid was stored at -20°C until it underwent PCR.
3.3. PCR
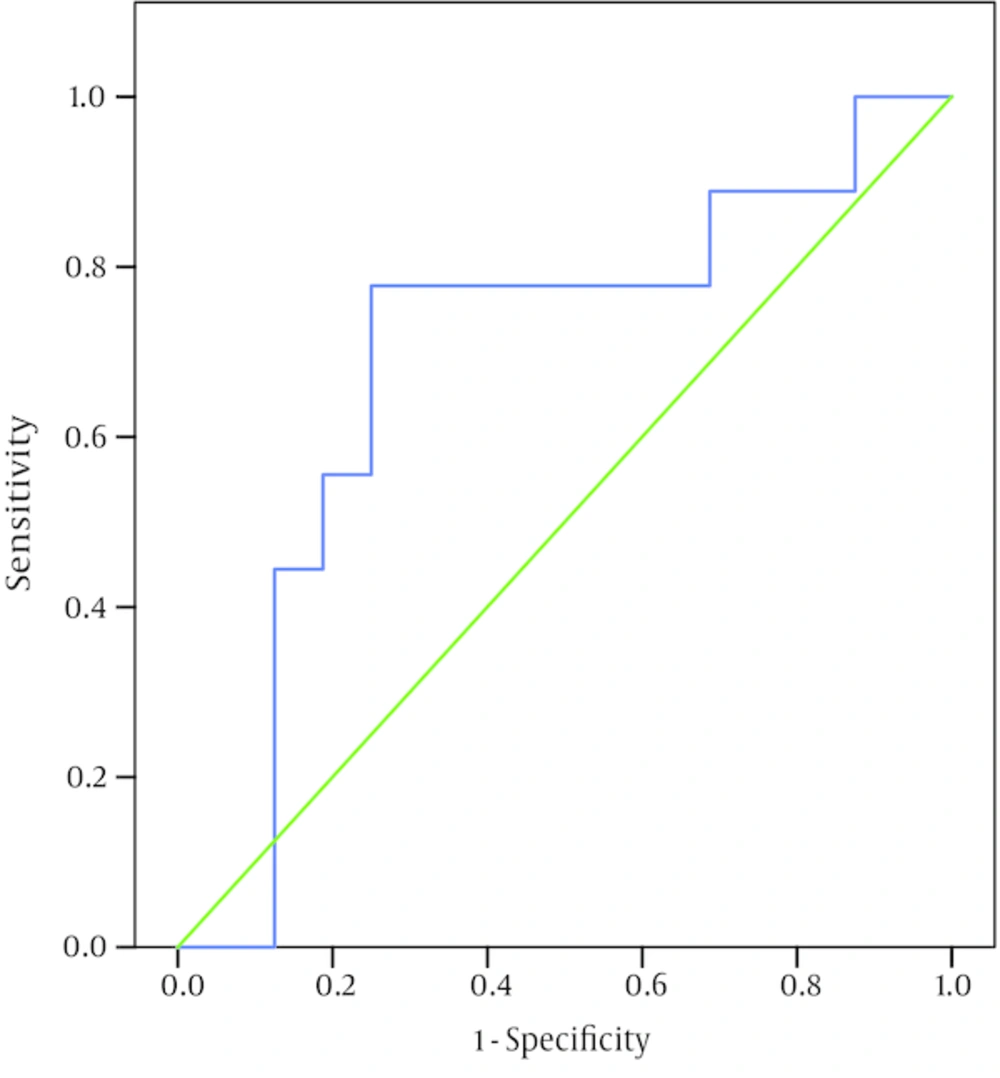
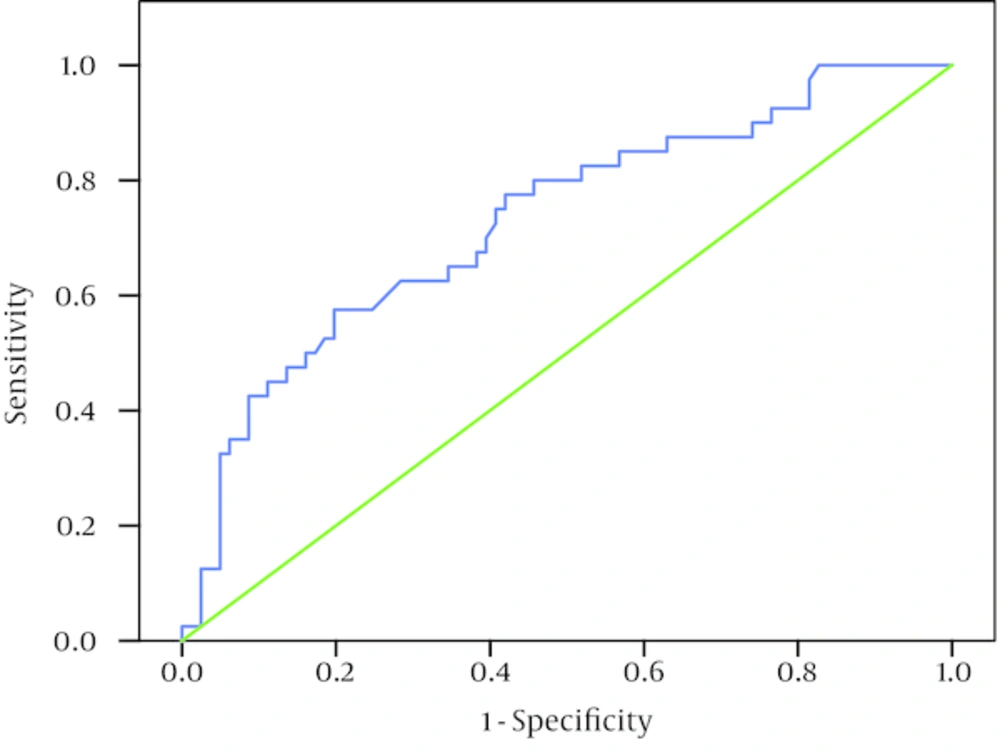
To assess the quality of the extracted genome, as well as inhibition of PCR test, all extracted and stored nucleic acid underwent beta-globin PCR, using the PCO3/PCO4 primer set, as described previously with modifications in method (13). The beta-globin PCR was performed in syber green real-time PCR-melting curve format (Figure 1). To detect CMV, real-time PCR was performed using envelope glycoprotein B (gpUL55) gene primer sets amplifying 116 bp gene region of the virus genome (CMV-r ; 5’-AAGTACCCCTATCGCGTGTG-3’), CMV-f; 5’-ATGATGCCCTCRTCCARGTC -3’, with an internal probe, CMV-P ; 5’-FAM-TGGCCCAGGGTACGGATCTTATTCG-BHQ1-3’) (14). Amplification of CMV gpUL55 genes was performed in reaction volumes of 20 μL under the following conditions: first the samples underwent denaturation at 94°C for 10 minutes, followed by denaturation at 94°C for 10 seconds, followed by annealing and extension at 60°C for one minute, 50 cycles (Figure 2). Real-time PCR system CFX-96 (BIO-Rad, USA) with HS prime taq premix TaqMan reagent (GENETBIO, Korea) was used in real-time PCR assay. The limit detection of 5 genome copies of CMV per reaction was determined by the real-time assay, using the serial dilutions of AmpliRun® CYTOMEGALOVIRUS DNA CONTROL (Vircell, Spain).
3.4. Statistical and Ethical Considerations
The achieved data were compared by chi-square (or Fisher’s exact test if appropriate). P value of less than 0.05 was considered to indicate statistical significance.
In this study, no ethical issues were involved; only the pathology reports were reviewed retrospectively, and the patients were anonymous. The articles used as references are valid and the information taken are reported unchanged.
4. Results
Thirty patients with pathologic diagnosis of LCH were included in this study. All patients were Iranians (16 males and 14 females) and the age ranged 2 months to 10 years. Age, sex and biopsy site of all patients are shown in Table 1. Thirty tissue samples with non LCH diagnoses were also selected as controls which were age and site-matched to LCH cases. CMV DNA was detected in only 2 (6.66%) LCH patients out of 30 cases (positive results in 6.66% and negative results in 93.34%). In control group, we detected CMV virus in 1(3.3%) sample out of a total of 30 cases (positive results in 3.3% and negative results in 96.7% of controls) with a P value of 1.00 (1.00 > 0.05) and OR: 2.07; 95% CI of OR: 0.18 - 24.15 which shows no significant difference in CMV prevalence results between LCH patients and controls. The LCH patients with positive result for CMV expression were a 2 year old boy with frontal bone lesion and a 1 year old girl with chest skin lesion; the positive control was in a 6 year-old boy with skin biopsy diagnosed as pilonidal fistula.
| Age | Gender | Clinic/Biopsy Site | |
|---|---|---|---|
| Female | Lymph node | - | |
| Male | Mediastinal and neck mass | - | |
| Male | Skin | - | |
| Male | Soft tissue, scalp mass | - | |
| Male | Frontal bone | + | |
| Male | Mastoid bone | - | |
| Female | Skin, chest wall | + | |
| Male | Iliac bone | - | |
| Female | Proximal tibia | - | |
| Male | Skull and soft tissue | - | |
| Female | Parietal bone and soft tissue | - | |
| Male | Skin | - | |
| Male | Soft tissue, scalp | - | |
| Female | Soft tissue, submandibular | - | |
| Male | Vertebral bone | - | |
| Male | Clavicle and soft tissue | - | |
| Male | Abdominal mass | - | |
| Female | Base of skull | - | |
| Female | Right lobe of lung | - | |
| Female | Skin, abdomen | - | |
| Female | Soft tissue | - | |
| Male | Soft tissue, scalp | - | |
| Female | Frontal bone and soft tissue | - | |
| Female | Soft tissue, scalp | - | |
| Female | Metatarsal bone | - | |
| Male | Skin | - | |
| Female | Skin | - | |
| Female | Skin | - | |
| Male | Soft tissue, scalp | - | |
| Male | Soft tissue, perianal | - |
5. Discussion
LCH is a rare disease involving clonal proliferation of bone marrow derived Langerhans cells which mostly affects children, particularly children younger than 5 years with an incidence of about 5 per 1,000,000 (2). Clinically, there are three overlapping clinical syndromes including multifocal multisystemic LCH (Letterer-Siwe syndrome), multifocal unisystemic LCH (hand-Schuller-Christian syndrome) and unifocal LCH (solitary eosinophilic granuloma) (2). Histologically, the findings are the same in various tissues, characterized by granulomas composed of a mixture of Langerhans cells, macrophages, eosinophils, multinucleated giant cells and lymphocytes (15, 16).
The prognosis of LCH is influenced by the involved organs and the age. Most adult patients with lung involvement usually have an indolent course of regress, whereas children need to be treated (17-20).
CMV can infect dendritic cells and Langerhans cells (21-23). Kawakubo et al. (9) detected CMV in lesional Langerhans cells in 30% of 29 patients by immunochemistry, in situ hybridization, and PCR, indicating that release of cytokines stimulates Langerhans cell growth and induction of LCH. Jeziorski et al. (10), however, did not support the hypothesis of the role of EBV, CMV, or HHV-6, in the pathogenesis of LCH in their study. McClain et al. (11) also failed to find evidence of genomes for adenovirus, CMV, EBV, HSV, HHV-6, human immunodeficiency virus, human T-cell leukemia virus types I and II, and parvovirus in 56 cases of LCH employing in situ hybridization and PCR technique.
We detected CMV DNA in only 2 patients with LCH (positive results in 6.66% and negative results in 93.34%). Only one in our control group had CMV virus (positive results in 3.3% and negative results in 96.7% of controls), which could be attributed to a coincidence. The P value of 1.00 (1.00 > 0.05) and OR: 2.07; 95% CI of OR: 0.18 - 24.15 indicates no significant difference in CMV prevalence results between LCH patients and controls. This is in keeping with some other results reported in the literature (10, 12).
In previous studies (9-12) authors declared no limitations and the methods used included serology, immunochemistry, in situ hybridization, and PCR. However, immunochemistry and in situ hybridization for CMV were not available to be employed in our study and the patients were not checked for the evidence of CMV infection serologically (limitations in our study).
5.1. Conclusions
Our study is the first study performed in Iran on this subject and does not support the hypothesis of a role for CMV in the pathogenesis of LCH, in concordance with some other studies in the literature (10-12).