1. Background
Anemia is one of the most common health problems in the whole world and has affected about one-fourth of the worlds’ population. Undesirable health outcomes of anemia impact all different groups of people within a society especially children and women in fertility ages (1, 2).
Based on the estimations of World Health Organization, prevalence of anemia in women aged 15 - 59 years is 10.3%, while in developing countries, the prevalence of anemia for the same age groups and among pregnant women, as an at risk group, has been estimated to be 22.5% and 52%, respectively (3). According to the studies in Iran, prevalence of anemia in pregnant women varies from 4.3% to 24.4% (4, 5).
Different risk factors in women of reproductive age such as menstruation, contraception methods, and pregnancy put them at a higher risk for anemia (6). Many factors such as pica, tea consumption, and low eating of red meat, and eggs are associated with anemia in pregnancy (6). Anemia as an important factor in death complicates pregnancy and child birth (6, 7). Other complications of anemia include preterm labor, irreversible mental and physical harms can affect both mother and fetus and also result in a baby with low birth weight (1, 8, 9).
Fetus’s growth occurs in different trimesters but the most mineral deficiency happens in the third trimester. Therefore, studying the effects of anemia on fetus can be greatly helpful. Kumar et al. investigated the effect of anemia on birth weight and preterm delivery in different trimesters (10).
2. Objectives
The present study was conducted to evaluate other fetal and maternal complications of anemia in the various trimesters.
3. Methods
3.1. Study Population
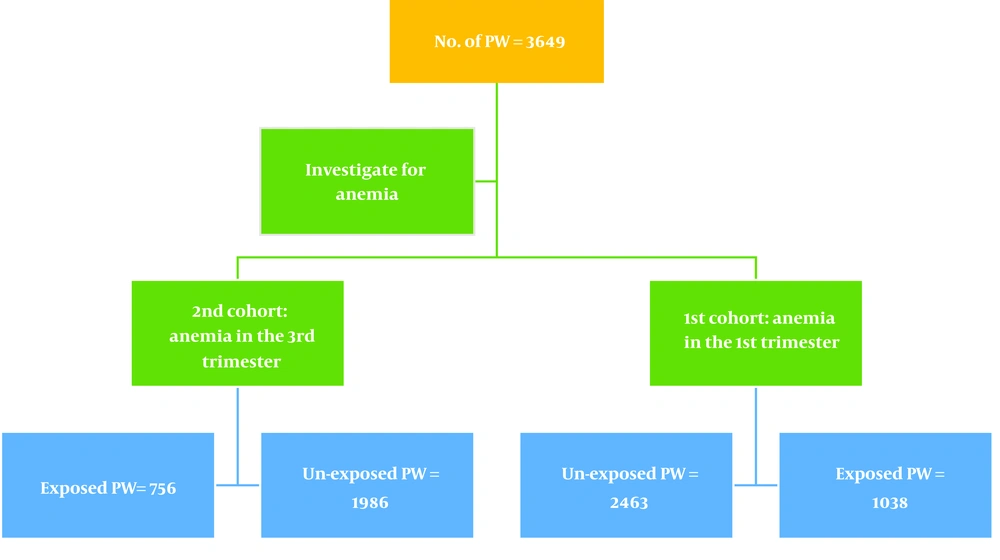
A large retrospective cohort study was conducted on Iranian pregnant women referring to health centers of Fars, Hormozgan, Kermanshah, Hamedan, Kohkiluyeh va Boyerahmad, Yazd, South Khorasan, Golestan, Mashhad, and Zahedan provinces. First study included 1038 exposed PW with hemoglobin level less than 11 g/dL during the first trimester (group 1) and 2463 pregnant women as un-exposed group with hemoglobin level more than 11 g/dL. The second study comprised 756 exposed cases with hemoglobin level less than 11 g/dL during the third trimester (group 2) and 1986 subjects as un-exposed group (Figure 1). Data were collected during years 2015 - 2017. In Iran, a rural health clinic (RHC) is located in a village covering all health houses of the villages of the area. The major tasks of RHC include supporting health houses and monitoring their performance, acceptance of intake referrals as well as establishing communications with higher-level supervisors. An urban health center is located in urban areas covering all health clinics in the area. Health centers in Iran provide care and record information before, during and after the pregnancy. Based on the Iranian National Antenatal Care protocol in the primary health care system, laboratory testing including full blood and urine tests are requested for all pregnant women at two stages, 6 - 10 weeks and 26 - 30 weeks of gestation. Anemia classification was performed based on world health organization guidelines. Subjects with hemoglobin level lower than 11 g/dL were divided in exposed group and subjects with hemoglobin level higher than 11 g/dL were divided into un-exposed group (6, 11).
Sample size was estimated using ratio estimation with double sampling based on the results of the previous studies (P0 = 0.3, P1 = 0.44, Z0.95 = 2, Z(1-β) = 0.8) and maternal age over 35 years was determined as a major risk factor (12). The design effect was estimated at 2 and sample size was calculated 370. Given the number of losses and technical issues during the study period, 16 subjects were added to each of the 17 studied factors and the final sample in each group was estimated 650.
Multistage sampling was performed and a total of nine provinces were selected based on geographical location. Then, four cities were selected from each province. At the next stage, one rural and one urban health clinic were selected in each city. Data were collected through medical record review and conducting interviews using researcher-made questionnaire. The questionnaire was comprised of demographic data on mother’s age, mother’s education (illiterate, elementary, guidance school, high school, and college education), location of residence (city or village), pregnancy intervals (year) and pregnancy outcomes such as neonatal mortality (child deaths within the 28 days of birth), type of delivery (vaginal or caesarean section), birth weight (low birth weight = under 2500 g, high birth weight = over 4000 g), fasting blood sugar (FBS), glucose tolerance test (GTT), gestational diabetes (yes, no), premature births (birth prior to 37 weeks of gestation), and abortion. As such, a checklist was distributed among health experts in all selected health clinics to collect required data based on a similar guideline through medical record review.
3.2. Data Analysis
Descriptive analyses were performed by percentage and frequency statistics. Logistic regression analysis was used to evaluate the relationship between maternal anemia with different pregnancy outcomes. After adjusting for pregnancy interval, variables with P value less than 0.2 were entered to the model using backward elimination. All analytical tests were two-tailed and the P value of less than 0.05 was considered significant. Data were analyzed using STATA software (version 13.1; Stata Corp, Texas, USA).
4. Results
4.1. Characteristics of Pregnant Women During the First Trimester
The present study showed that there was a significant relationship between anemia and mother’s education, type of delivery, gestational diabetes and birth outcome during the first trimester. In comparison of PW with and without anemia, PW with under diploma (49.32 vs. 47.8%, P = 0.002), with vaginal delivery (72.8 vs. 65.5%, P < 0.001) and with neonatal mortality (56.83 vs. 50.6%, P = 0.009) had higher frequency of anemia. In addition, PW with anemia had lower gestational diabetes compared with healthy PW (2.65 vs. 4.37%, P = 0.01). In other side, there was no significant relationship between anemia and mother’s age, living location, birth weight, pregnancy intervals, abnormal FBS, abnormal GTT, gestational age and abortion during the first trimester (Table 1).
| Variables | Study 1 | P Value | Study 2 | P Value | ||
|---|---|---|---|---|---|---|
| Anemia in 1st trimester | No Anemia | Anemia in 3rd trimester | No Anemia | |||
| Mother’s age | 0.32 | 0.02 | ||||
| < 20 | 129 (12.52) | 321 (13.22) | 88 (11.81) | 236 (12.01) | ||
| 21 - 25 | 303 (29.42) | 763 (31.43) | 203 (27.25) | 639 (32.52) | ||
| 26 - 35 | 505 (49.03) | 1114 (45.88) | 371 (49.8) | 925 (47.07) | ||
| 36 - 40 | 65 (6.31) | 177 (7.29) | 59 (7.92) | 125 (6.36) | ||
| > 41 | 28 (2.72) | 53 (2.18) | 24 (3.22) | 40 (2.04) | ||
| Living location | 0.12 | < 0.001 | ||||
| Urban | 487 (47.9) | 1077 (45) | 286 (38.39) | 896 (46.47) | ||
| Rural | 530 (52.1) | 1316 (55) | 459 (61.61) | 1032 (53.53) | ||
| Education | 0.002 | 0.003 | ||||
| Illiterate | 68 (6.56) | 125 (5.09) | 45 (6) | 72 (3.63) | ||
| Under diploma | 511 (49.32) | 1175 (47.8) | 364 (48.21) | 935 (47.2) | ||
| Diploma | 383 (37) | 885 (36) | 260 (34.44) | 792 (40) | ||
| Academic | 74 (7.14) | 273 (11.11) | 86 (11.4) | 182 (9.19) | ||
| Type of delivery | < 0.001 | 0.05 | ||||
| Vaginal | 752 (72.8) | 1597 (65.5) | 475 (63.42) | 1325 (67.3) | ||
| Cesarean | 281 (27.2) | 841 (34.5) | 274 (36.6) | 644 (32.71) | ||
| Birth weight, g | 0.12 | 0.09 | ||||
| < 2500 | 362 (42.24) | 965 (46.24) | 240 (37.85) | 746 (42.46) | ||
| 2500 - 4000 | 476 (55.54) | 1084 (51.94) | 384 (60.57) | 977 (55.61) | ||
| > 4000 | 19 (2.22) | 38 (1.82) | 10 (1.58) | 34 (1.94) | ||
| Pregnancy intervals, y | 0.1 | 0.001 | ||||
| 0 | 0 (0.0) | 1 (0.04) | 1 (0.13) | 0 (0.0) | ||
| 1 | 70 (6.83) | 156 (6.47) | 45 (6.06) | 130 (6.6) | ||
| 2 | 323 (31.51) | 662 (27.47) | 223 (30.05) | 573 (29.37) | ||
| 3 | 281 (27.41) | 674 (27.97) | 248 (33.42) | 518 (26.55) | ||
| 4 | 351 (34.24) | 917 (38.05) | 225 (30.32) | 730 (37.42) | ||
| Abnormal FBS | 0.06 | 0.37 | ||||
| No | 845 (94.41) | 2002 (92.56) | 635 (92.57) | 1731 (93.57) | ||
| Yes | 50 (5.6) | 161 (7.44) | 51 (7.43) | 119 (6.43) | ||
| Abnormal GTT | 0.3 | 0.001 | ||||
| No | 780 (92.09) | 1849 (90.9) | 608 (89.28) | 1727 (93.15) | ||
| Yes | 67 (7.91) | 185 (9.1) | 73 (10.72) | 127 (6.85) | ||
| Gestational diabetes | 0.01 | 0.66 | ||||
| No | 993 (97.35) | 2321 (95.63) | 707 (96.19) | 1897 (96.54) | ||
| Yes | 27 (2.65) | 106 (4.37) | 28 (3.81) | 68 (3.46) | ||
| Gestational age, wk | 0.13 | < 0.001 | ||||
| > 37 | 329 (58.54) | 825 (62.17) | 271 (59.96) | 813 (73.51) | ||
| < 37 | 233 (41.46) | 502 (37.83) | 181 (40.04) | 293 (26.49) | ||
| Abortion | 0.32 | < 0.001 | ||||
| No | 895 (86.22) | 2154 (87.45) | 633 (83.73) | 1775 (89.38) | ||
| Yes | 143 (13.78) | 309 (12.55) | 123 (16.27) | 211 (10.62) | ||
| Birth outcome | 0.009 | 0.01 | ||||
| Live birth | 275 (43.17) | 726 (49.4) | 243 (49.7) | 704 (56.0) | ||
| Neonatal mortality | 362 (56.83) | 744 (50.6) | 246 (50.3) | 552 (44.0) | ||
Abbreviations: FBS, fasting blood sugar, GTT, glucose tolerance test.
4.2. Characteristics of Pregnant Women During the Third Trimester
The results showed that there was significant relationship between anemia and mother’s age, living location, mother’s education, abnormal GTT, gestational age, abortion and birth outcome during the third trimester. Comparing PW with and without anemia, PW in age group of 26 - 35 years (49.8 vs. 47.07%, P = 0.02), living in rural area (61.61 vs. 53.53%, P < 0.001), with under diploma education (48.21 vs. 47.2%, P = 0.003), with three years pregnancy interval (33.42 vs. 26.55%, P = 0.001), with abnormal GTT (10.72 vs. 6.85%, P = 0.001), with gestational age < 37 weeks (40.4 vs. 26.49%, P < 0.001), with abortion (16.27 vs. 10.62%, P < 0.001), with neonatal death (50.3 vs. 44.0%, P = 0.01) had higher frequency of anemia during the third trimester. Nevertheless, there was no significant relationship between anemia and type of delivery, birth weight, abnormal FBS, and gestational diabetes during the third trimester (Table 1).
4.3. Association of Anemia and Related Pregnancy Outcomes Using Univariate and Multiple Logistic Regression Models
After adjusting for the potential confounding factors, the odds of neonatal mortality (OR = 1.63; CI 95%, 1.25 - 2.13) were significantly higher and the odds of cesarean delivery (OR = 0.6; CI 95%, 0.46 - 0.75) were significantly lower in women who had anemia during the first trimester than those without anemia. In other side, adjusted analysis revealed that the variables of birth weight, FBS, gestational diabetes and gestational age did not remain significantly associated with anemia during the first trimester (Table 2).
| Variables | Anemia in 1st Trimester | Anemia in 3rd Trimester | ||
|---|---|---|---|---|
| Crude OR | Adjusted OR | Crude OR | Adjusted OR | |
| Birth outcome | ||||
| Live birth | 1 | 1 | 1 | 1 |
| Neonatal mortality | 1.28 (1.06 - 1.54) | 1.63 (1.25 - 2.13) | 1.29 (1.04 - 1.6) | 1.08 (0.82 - 1.44) |
| Type delivery | ||||
| Vaginal | 1 | 1 | 1 | 1 |
| Cesarean | 0.7 (0.6 - 0.8) | 0.6 (0.46 - 0.75) | 1.18 (1 - 1.41) | 1.07 (0.83 - 1.4) |
| Birth weight, g | ||||
| 2500 - 4000 | 1 | 1 | 1 | 1 |
| < 2500 | 0.85 (0.72 - 1) | 0.82 (0.6 - 1.1) | 0.81 (0.67 - 0.98) | 0.66 (0.46 - 0.93) |
| > 4000 | 1.13 (0.64 - 2) | 1.91(0.9 - 4.08) | 0.74 (0.36 - 1.52) | 0.6 (0.23 - 1.54) |
| FBS | 0.73 (0.53 - 1.02) | 0.51 (0.25 - 1.02) | 1.16 (0.83 - 1.64) | - |
| GTT | 0.85 (0.64 - 1.14) | - | 1.63 (1.2 - 2.2) | 1.38 (0.9 - 2.15) |
| Gestational diabetes | 0.6 (0.38 - 91) | 0.84 (0.34 - 2.08) | 1.1 (0.7 - 1.73) | - |
| Gestational age, wk | ||||
| > 37 | 1 | 1 | 1 | 1 |
| < 37 | 1.16 (0.95 - 1.42) | 1.19 (0.9 - 1.6) | 1.85(1.47 - 2.33) | 2.15 (1.6 - 2.91) |
| Abortion | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.11 (0.9 - 1.37) | - | 1.63 (1.28 - 2.07) | 1.68 (1.11 - 2.53) |
Abbreviations: FBS, fasting blood sugar; GTT, glucose tolerance test; OR, odds ratio.
The chance of pre-term delivery (< 37 weeks; OR = 2.15; CI 95%, 1.6 - 2.91) and abortion (OR = 1.68; CI 95%, 1.11 - 2.53) were significantly higher in women who had anemia during the third trimester, while the chance of low birth weight (< 2500 kg) (OR = 0.66; CI 95%, 0.46 - 0.93) was lower in anemic women during the third trimester than in those without anemia. Adjusted analysis showed that no significant association remained between anemia and birth outcome, type of delivery, birth weight, and GTT during the third trimester (Table 2).
5. Discussion
In univariate analysis there was a significant relationship between neonatal (0 - 28 days after birth) mortality, caesarean delivery, and gestational diabetes with anemia during the first trimester. The variables neonatal mortality, caesarean delivery, low birth weight, GTT, prematurity, and abortion had a significant relation with anemia during the third trimester. However, in multivariate analysis, there was a significant correlation between variables neonatal mortality and caesarian delivery with anemia in first trimester and variables low birth weight, prematurity, and abortion with anemia in the third trimester of pregnancy.
In the current study a significant relationship was found between mother’s anemia in the first trimester and neonatal mortality. Based on the literature review, no study was found that assessed the relation between mother’s anemia in the first trimester and neonatal (0 - 28 days) Mortality. Most studies considered the correlation between mother’s anemia not merely in first trimester and prenatal death which includes still births and deaths within the first few weeks of life. According to some of these studies, there is a significant relationship between mother’s anemia and prenatal death (13, 14). Tomashek et al. also found a remarkable relationship between stillbirths and mother’s anemia (15).
Maternal anemia can result in weak outcome of pregnancy including infant mortality (7). A literature review showed significant relationship between mother’s anemia in the beginning of pregnancy with small for gestational age and low birth weight (16-18). On the other hand, low birth weight increases the risk of infant mortality (19, 20).
The present study showed a statistically significant relationship between mother’s anemia and caesarean delivery in the first trimester. Pregnant women who had anemia in the first trimester had lower chance to undergo caesarean section. In literature review, no study was found showing the relationship between mother’s anemia in first trimester and caesarian. Caesarian section compared to natural vaginal birth is associated with more bleeding that is a critical factor for creation of anemia and its complications (21). Therefore, appropriate and educational planning to replace caesarian with natural birth can at least decrease the number of selective caesarians.
In univariate analysis, there was a significant relationship between mother’s age and occurrence of anemia in the third trimester (Table 1). Rajabzadeh et al. didn’t find any remarkable relationship between age and anemia in pregnant women which may be due to their smaller sample size and type of their study (22). However, in other studies an increase in age over 35 was associated with more anemia frequency (23, 24). In Rasheed et al.’s study in Saudi Arabia, increase in age has been reported as a factor causing anemia (25). So, the necessity of anemia preventing education of young girls is quite obvious, because in older ages, due to different reasons such as previous pregnancies and childbirths, women lose their resources of iron (23).
The present study revealed a significant relationship between low birth weight and mother’s anemia in the third trimester. The study of Kumar et al. didn’t show a significant relationship between anemia in the first and second trimesters with low birth weight and only the difference was statistically significant when the mothers had anemia during the third trimester of pregnancy (10). A retrospective cohort study showed no statistically significant relationship between low birth weight and anemia in the first trimester (10). Several studies point out a significant relationship between low birth weight and mother’s anemia, all of which considered hemoglobin level in third trimester or childbirth time (10, 26-28). So, it can be concluded that hemoglobin in third trimester is a vital element in determining low birth weight. It is clear that fetus grows faster in the third trimester and more iron and micronutrients are needed and this physiologically explains the relationship between hemoglobin level in the third trimester and low birth weight.
Another finding of our study was a significant relationship between prematurity and mother’s anemia in the third trimester. Kumar et al. showed that except for the first trimester, anemia in other trimesters increases the risk of preterm birth and this relationship is stronger in the third trimester (10). Many other studies point out a similar relationship between anemia and preterm outcome (26, 29). There are some studies that couldn’t confirm a remarkable relationship between anemia in the first trimester and preterm birth which is to see in our study (10, 16). But in another study carried out in China, a relationship between preterm birth and anemia in all three trimesters has been reported with an opposite trend (a strong relationship between anemia in first trimester and preterm birth, compared to anemia in third trimester) (30). This was also reported in another similar study (31). It seems that more studies are needed in this area.
5.1. Conclusions
Pregnant women who experience anemia in both first and third trimesters of pregnancy have different unpleasant pregnancy outcomes. Since anemia is preventable during pregnancy, many of these outcomes such as neonatal mortality, low birth weight, preterm and cesarean delivery, and abortion could be prevented and decreased by providing health education before pregnancy.