1. Background
Necrotizing enterocolitis (NEC) is a common dangerous gastrointestinal (GI) emergency that can affect premature infants all over the world (1). Despite all developments in neonatology, because of its unknown etiology, the morbidity and mortality of NEC has not been decreased significantly. Its incidence ranges between 3% and 28% in newborns weighing less than 1500 g, 2% - 5% in all admissions, and 5% - 10% in very low birth weight (VLBW) infants (2). The mortality rate of NEC is 10% - 20% (3), and postoperative complications, e.g. short bowel syndrome, affect many of these neonates (4). With regards to white matter injury, neurodevelopmental problems are seen in these patients, as well (4). There is no definite treatment for NEC but some conservative strategies are undertaken to reduce complications. The newborn babies’ GI tract is sterile right after birth, but colonization of bacteria starts in a short while (5, 6). Colonization delay is a result of GI tract prematurity, enteral feeding restriction and wide administration of antibiotics. These factors may cause aberrant bacterial colonization in the preterm infant’s GI tract (7, 8). Recent studies have shown that administration of probiotic components reduces the NEC incidence and mortality rate in preterm infants who weigh less than 1500 g (1, 9-13), but the results are not reliably estimated for extremely low birth weight (less than 1000 g) preterm infants (14-23). These studies have shown that administration of probiotics does not cause systemic infection or any other direct side effects (14-24). The mechanism of action of probiotics is to produce some metabolic byproducts that may modulate the immune system, such as butyrate fatty acid which can predominate over pathogenic microorganisms of the GI tract (25-27). However, choosing the best type of probiotics and the effective dose is still a question (28).
2. Methods
In this study for the first time, a probiotic agent was administered in 8 to 10 separate doses in the form of minimal enteral feeding between two breast milk feedings. This study was designed and conducted in maternal, fetal, and neonatal research center of Tehran University of Medical Sciences as a research proposal. All premature newborns (n = 115) weighting 750 - 1500 g or less than 32 weeks’ gestation who received antibiotics and total parenteral nutrition in NICU of Vali Asr Hospital were included. Premature babies less than 750 and more than 1500 grams and neonates with congenital heart disease, congenital malformations, and immune system deficiency, even in their family members, were excluded from the study. In this double blind randomized clinical trial (RCT), block randomization was used and 60 cases were randomly divided into 2 groups. After vital signs were stable, minimal enteral feeding with a probiotic agent (0.8 - 1 g per day) was started. In the first 10 days of life, the target group received 1 g of multi strain powder probiotic infant formula (Protexin-Restore product) with enteral feeding in 8 to 10 divided doses for at least 7 days. The control group received enteral nutrition without probiotics. Protexin-Restore (Probiotic International Ltd, United Kingdom) is a multi-strain probiotic suitable for children of all ages. Every sachet of this powder contains 990 mg of Fructo-oligosaccharide as prebiotic and 1 billion bacteria. The bacterial species are listed in Table 1. NEC signs (Table 2), stool culture, gastric lavage, and weight were checked every day. Height and head circumstance were checked weekly. Both groups were compared for variables listed in Table 3. The primary outcome was the occurrence of NEC, and secondary outcomes were weight gain, mean days of TPN, mean days of full feeding achievement, mean days of hospitalization, and CRP rise. Data were analyzed with SPSS software version 7.1. Descriptive variables are presented as frequency and percentile as well as mean with and without standard deviation. Chi square and t-test were used to compare variables between the two groups. P values less than 0.05 were considered significant. The power of the study was 80%.
| Species | Subsp. |
|---|---|
| Streptococcus | Thermophilus |
| Lactobacillus | Rhamnosus |
| Lactobacillus | Acidophilus |
| Lactobacillus | Bulgaricus |
| Bifidobacterium | Infantis |
| Lactobacillus | Casei |
Bacterial Species in the Administered Probiotic Substance
| NEC Signs | |
|---|---|
| - | Lethargy |
| - | Feeding residual |
| - | Emesis (bloody and or biliary) |
| - | Ileus (decrease or lack of bowel sounds) |
| - | Persistent abdominal distention over 6 h |
| - | Bloody stool |
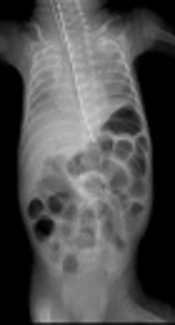
| - | Positive radiographic signs |
NEC Signs Considered in This Study
| Variable | Case Group | Control Group |
|---|---|---|
| Mean Gestational Age, w | 29.47 | 29.63 |
| Mean 5th minute Apgar | 7.07 | 7.33 |
| Resuscitation requirement, % | 93.3 | 96.7 |
| Birth weight, g | 1144.23 | 1162.33 |
| Mean days of oxygen therapy | 34.14 | |
| Mean days of TPN | 32.13 | 31.37 |
| Mean days of full feeding achievement | 20.80 | 19.73 |
| Mean days of hospitalization | 58.37 | 54.97 |
| Mean weight gain, gram per day | 10.54 | 11.85 |
| CRP rise, % | 6.7 | 30 |
| NEC Grade 1, % | 16.7 | 26.7 |
| NEC Grade 2, % | 0 | 20 |
Comparison of Variables Between Case and Control Groups
3. Results
The mean gestational age, 5th-minute Apgar score, and the need for resuscitation were almost similar in both groups (P > 0.05 for all). The mean age at the start of probiotic administration was 13.2 days. The length of hospital admission was not different between the two groups (P > 0.05).
The mean duration of oxygen therapy, TPN, full feeding achievement, and hospitalization were compared between the two groups but the differences were not significant. Comparison of weight gain also showed no significant difference between these groups (P > 0.05).
The incidence of NEC and C-reactive protein (CRP) rise showed a significant difference between case and control groups (P = 0.02). In the case group, CRP increased in two patients. One suffered from sepsis and the other one had feeding intolerance that was treated with continuing probiotic administration. In the control group, CRP increased in 9 patients (Table 3). In four neonates the reason for it was not clear, one case had many WBCs in U/A, one had Staphylococcus epidermidis in B/C, one had Klebsiella in U/C, one had Candida albicans in U/C, and one had occult blood in stool, Base excess showed an average decrease of 3.1. NEC and/or enteral dysmotility was seen in 5 infants in the case group and 14 infants in the control group (Table 3); in 4 out of 5 infants in the case group the ailment improved with continuing the probiotic feeding (P = 0.013).
4. Discussion
The rate of mortality in premature infants is affected by different factors and administration of probiotics has only a preventive role. Variation in the GI tract bacterial flora in addition to the use of antibiotics and delayed enteral feeding may lead to NEC in preterm infants (29, 30). Although clinicians are unanimous in the benefits of probiotics administration, there are no guidelines available for clinicians yet (14-28, 31). The effective dose of probiotics varies in different sources but clinicians agree on administration of multi organisms instead of a single species (15). Deshpande et al showed that probiotics could decrease NEC in newborns weighing over 1000 g (24). On the other hand, it is still a concern whether live organisms in probiotics can potentially colonize in the gastrointestinal system of newborns, especially those under 750 g (4). Although 9 RCT studies in several years showed that administration of probiotics did not cause systemic infection or other direct side effects, the benefit of probiotics for infants weighing less than 1000 g is a matter of controversy and more investigations are required to clear this (14-23). Thus, we decided to administer probiotics to newborns weighing 750 to 1000 g. Instead of 1 - 2 doses of probiotics which can increase milk osmolarity, we fed newborns with probiotics between two breast milk feeding in 8 to 10 divided doses for the first time. Similar to the results of a study by Li et al. (31), our study showed positive preventive effects of probiotics on enterocolitis and its complicated forms in very low birth weight and premature infants and a decrease in the NEC severity in the case group, so we observed no second grade NEC in the case group (P = 0.013) (Table 3). We administered probiotics to premature infants < 1000 g without any complications, although Deshpande et al administered it cautiously in this group (24). The probiotic substance (Protexin) used in the present study contained lactobacillus and bifidobacterium which according to various studies, are the most effective species for premature infants (18, 19, 26). In our study, the duration of probiotic administration was at least 13 days. According to Crittenden et al, after discontinuing probiotic, its effect will remain for 2 - 3 weeks (32). All newborns were treated primarily with antibiotics. Since postbiotics are the remaining agents of probiotic organisms, we decided to administer probiotics despite antibiotic treatment. This could stop invasive GI organisms and prevent septicemia, urosepsis, and entrocolitis. One of the by-products of postbiotics is lactic acid; therefore, the effectiveness of probiotics and postbiotics was examined with blood pH and base excess via the ABG measurements.
4.1. Limitations
In our study, we had some limitations, including the number of cases and restriction not to include complicated cases. However, we hope that the results pave the way in future for more comprehensive clinical trials on the effect of probiotics on NEC in preterm infants.
4.2. Conclusions
These results showed positive effects of probiotics on preventing and treating NEC, which is a serious disease in ELBW and VLBW neonates. We showed that probiotics could be administered in divided doses in breast milk feeding intervals. Many RCTs have found that probiotics can be used as a routine therapy for preterm infants (9), So we focused on a suitable type of probiotics, its dosage, and its administration interval to prevent NEC.