1. Context
Breast milk contains all the necessary nutrients for infants’ growth and development. During the prehistoric era, breastfeeding was among the priorities for mothers. It remained important through ancient times when the mother goddesses were statues with nude breasts. Despite the attention to the formula in the developed countries, the benefits of breast milk are still emphasized in the current world (1). Breast milk can save babies' lives, reduce maternal and infant disease burden (2), fulfill the nutritional needs of infants, improve infants’ cognitive function and immunity, facilitate infants’ nervous system development, decrease the incidence of diabetes 1 and 2, allergies, and sudden infant death syndrome (3).
According to the World Health Organization (WHO), premature infants should be definitely breastfed as breast milk can effectively decrease their morbidity and mortality rates (4). Therefore, a global campaign was initiated to increase awareness about the advantages of breastfeeding both for the baby and the mother. Consequently, a number of slogans, e.g. “Breastfeeding, a Life-saver” and “Breast Are the Best”, are now well-known throughout the world (2). The WHO and the United Nations Children’s Emergency Fund (UNICEF) advise mothers to start breastfeeding within the first hour after delivery (to stimulate milk production) (5), exclusively breastfeed their infants for six months, and continue breastfeeding for two years to provide additional nutrition (6). As a result of all these efforts, 75% of nurses in the US in 2013 considered getting the baby latched to her mother’s breast as a norm (2). However, some mothers stop breastfeeding in the first weeks or months after giving birth to their babies and put themselves and their babies at risk of developing negative health effects. Studies on Iranian nursing mothers identified having a job, inadequate breast milk, and infant’s crying as the most important barriers to continue breastfeeding (7). Meanwhile, ethnicity and fissures were reported as the most significant factors preventing continued breastfeeding in females in the US (8). Therefore, considering the countless benefits of breastfeeding and the complications of early cessation of breastfeeding occurring both for the mother and the newborn, the use of complementary medicine to increase breast milk encourage continued breastfeeding, and decrease the incidence of common breast conditions such as mastitis, nipple fissures, and breast engorgement. Complementary medicine uses herbal, animal, and mineral medicines, spiritual treatments, and practical techniques either alone or in combination to prevent, diagnose, and treat diseases or to maintain health (9). In some cases, there is little scientific evidence about the safety and efficacy of the methods applied in complementary medicine. However, a survey by the National Prescribing Service in Australia revealed that 65% of Australians used at least one supplementary medicine within a 12-month period (10). The US citizens spent nearly US$32 billion on dietary supplements in 2012. As estimated by the WHO, the global market for traditional medicine reaches US$83 billion each year (9). Various studies, thus, investigated the use and effects of complementary medicine on continued breastfeeding. Some of the evaluated methods include point massage of liver and stomach channel (11), the Oketani breast massage (to relieve breast pain, increase milk pH, improve milk taste, and increase the sucking speed of the neonates) (12), acupressure (to enhance milk production) (13), and the Guoshu acupoint pressure therapy (to treat acute mastitis during breastfeeding) (14). Some dietary methods such as potato and carrot soup consumption (11), taking vegetable supplements containing black cohosh, ginseng, garlic (15), Aloe vera, ginger, and blueberries, and flaxseed oil (to increase the omega-3 fatty acid content of breast milk) (10) are also investigated in a number of studies. Several studies also evaluated the role of postpartum care by health personnel (16) in mothers’ tendency toward continued breastfeeding. Traditional and complementary medicine in breastfeeding has lower side effects than modern medicine and is more cost-effective for families, and their benefits are proved in many studies. Increased attention paid by health care providers to the physiologic nature of childbirth and postpartum period leads them to consider complementary methods in breastfeeding problems. Most of these studies reported that the tested methods had positive impacts on the process and continuation of breastfeeding. The current review article aimed at collecting evidence about the impacts of complementary medicine as a safe method without any side effects on successful breastfeeding and breastfeeding problems in the postpartum period.
2. Data Sources
2.1. Search Strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were observed in the current study. A number of key terms, including “reflexology” OR “zone therapy” OR “massage therapy” OR “massage point” OR “massage” OR “complementary medicine” OR “alternative medicine” OR “complementary therapy” AND “breastfeeding”, OR “breast abscess” OR “nipple fissure” OR “plugged ducts” OR “engorgement” OR “mastitis” were selected and searched in valid databases of ISI Web of Science, MEDLINE, PubMed, Scopus, Embase, ProQuest, and ScienceDirect.
2.2. Inclusion and Exclusion Criteria
Only the studies published in English and Persian that used a case-control, observational, quasi-experimental, randomized controlled trial (RCT), or prospective descriptive cohort design were searched. The study time limit ranged 1999 to 2018 in order to include the newer and more updated articles due to the large volume of articles in this field and the increasing attention paid by people to complementary medicine than the past. Studies were included if they focused on exclusive breastfeeding, recruited females with no medical conditions or breast anomalies with a singleton pregnancy and gave birth to a baby without mouth and jaw disorders. Papers with full texts in languages other than Persian and English, case reports, and studies with incomplete data were excluded.
2.3. Study Selection
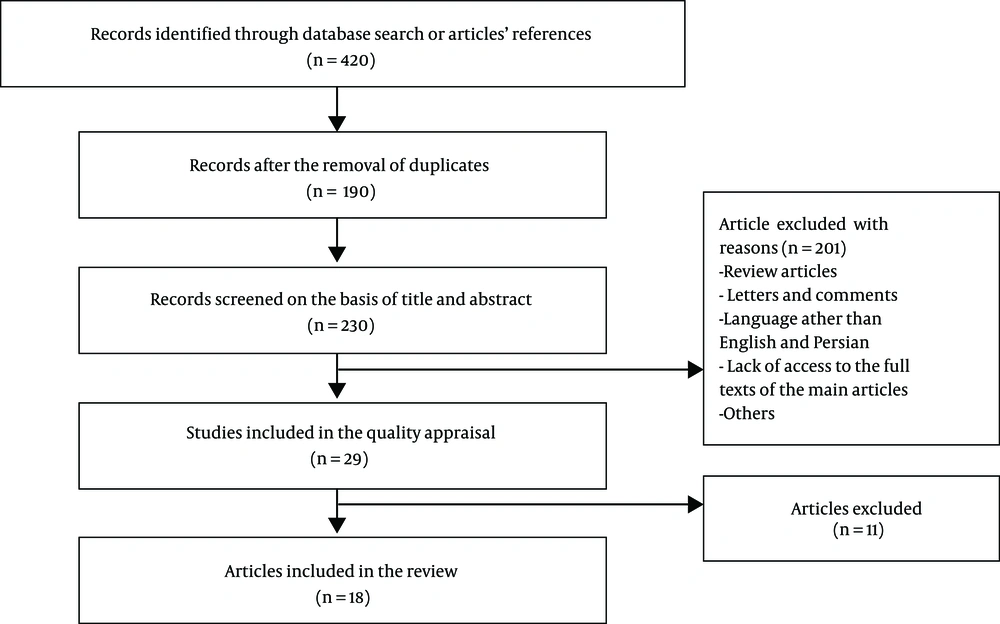
Two authors independently evaluated the eligibility of the extracted papers and resolved discrepancies through consensus. Of the initial search results, 190 papers were excluded due to irrelevance or duplicity. The evaluation of the titles and abstracts of the remaining articles resulted in the exclusion of 230 more papers. The full texts of the remaining papers were reviewed and 11 more articles were excluded accordingly. Finally, 18 articles were found eligible and entered the review process (Figure 1).
2.4. Quality Assessment
Based on the adherence to the STROBE checklist (17), quantitative studies were categorized as low-, moderate-, and high-quality (adherence to items 2 - 5,6, and 7, respectively).
2.5. Data Extraction
Study selection and validity assessment were conducted by two independent authors. A third author was consulted if any disagreement arose. After identifying the eligible papers, the first author’s name, publication year and country, study design, sample size, the participants’ main complaint, the intervention and control groups` characteristics, and measures and outcomes were extracted and entered the analysis.
3. Results
The process of the literature search is depicted in Figure 1. The abstracts and titles of the initial search results were evaluated. After the review of the full texts of potentially eligible papers, 18 papers that met the inclusion criteria and adhered to all seven items of the STROBE checklist (i.e. had high quality) entered the analysis. Table 1 summarizes the characteristics of the selected studies. As observed, the sample size of the selected studies ranged 11 to 3497, and a total of 5141 females were recruited by the selected studies. The studies were performed in different countries including Iran (n = 7), China (n = 3), the US (n = 2), Italy (n = 2), Brazil (n = 1), Taiwan (n = 1), Indonesia (n = 1), and Japan (n = 1) and examined females of different ages. While most studies (n = 13) used an RCT design, two observational, one case-control, one prospective cohort, and one quasi-experimental studies were also reviewed. As described above, the quality of the studies was assessed based on their adherence to the STROBE checklist (Table 2).
| Author, Year | Country | Study Type | Chief Complaint | Sample Size | Intervention Group | Control Group | Measure | Outcome |
|---|---|---|---|---|---|---|---|---|
| Luo, 2017 (11) | China | RCT | Normal breastfeeding | 320 | Point massage group + pith and trotter soup group | No interventions | Time of lactation | Point massage in the health center can promote milk supply, prevent delayed start of lactation, and increase the exclusive breastfeeding rate. |
| Witt, 2016 (16) | The US | Prospective cohort | Breast engorgement | 73 | Therapeutic breast massage in lactation (TBML) to manage engorgement, plugged ducts, and mastitis | No interventions | Engorgement severity | Physicians can apply TBML in their offices to decrease acute breast pain caused by milk stasis. Mothers reported that TBML was useful immediately after its application in the office, and also during the future episodes at home. |
| Meng, 2015 (18) | China | RCT | Milk stasis | 200 | Massages with cactus and Aloe cold compresses | Massage treatment or cactus and Aloe cold compresses | Feeding patterns, hardness, and pain after treatment | A combination of massage with cactus and Aloe cold compress could more effectively decrease breast hardness and pain compared with either cactus and Aloe or cold compress alone. |
| Heberle, 2014 (19) | Brazil | RCT | Breast engorgement | 16 | Treatment by means of massage and pumping | No interventions | Compared the differential patterns of temperature, before and after the treatment by means of massage and pumping | Thermography suggested massage and electromechanical pumping more beneficial than manual methods. |
| Chiu, 2010 (20) | Taiwan | RCT | Breast engorgement | 54 | The Guasha protocol selected appropriate acupoint positions, including ST16, ST18, SP17, and CV17 | Hot packs and massage for 20 minutes in accordance with recommendations given in an obstetrical technique textbook | Body temperature, breast temperature, breast engorgement, pain levels, and discomforting levels | The Guasha therapy could efficiently improve breast engorgement. |
| Foda, 2004 (21) | Japan | Case- control | Normal breastfeeding | 39 | Milk samples were obtained immediately before and after the massage from healthy, exclusively breastfeeding mothers at two different periods of lactation | No interventions | Total solids, lipids, casein | Breast massage significantly increased total solids, lipids, and casein content, as well as the gross energy of breast milk, and thus, improved its overall quality. |
| Khosravan, 2017 (22) | Iran | RCT | Breast engorgement | 40 | Routine interventions and warm compress before nursing and a cold compress after nursing + hollyhock compress | Routine interventions and warm compress before nursing and a cold compress after nursing | Breast engorgement severity | A combination of routine interventions and hollyhock leaf compress could decrease the severity of breast engorgement. |
| As’adi, 2017 (23) | Iran | RCT | Nipple fissure | 50 | Pistacia atlantica resin ointment | No interventions | Levels of nipple fissure and pain | Nipple fissures and breast pain were more effectively treated by Pistacia atlantica resin ointment compared with breast milk. |
| Marrazzu, 2015 (24) | Italy | Observational prospective | Nipple fissure | 40 | Silver cap | Standard of breastfeeding care | Painful symptoms | The painful symptoms of nipple fissures were more effectively resolved by the application of silver caps compared with standard care. |
| Zhao, 2014 (25) | China | Prospective observational | Plugged ducts | 3497 | SSRMT | SSRMT could be used as a safe and low-cost method to treat plugged milk ducts after delivery. | ||
| Akbari, 2014 (26) | Iran | RCT | Nipple fissure | 110 | Peppermint group applied four drops of menthol essence on their nipple and areolas after each feeding | 4 drops of their own milk on the nipple and areolas after each feeding | Intensity of pain -The existence or lack of nipple discharge | Lactating females reported the application of menthol essence to improve nipple fissures. |
| Shahrahmani, 2016 (27) | Iran | RCT | Nipple fissure | 100 | 0.5 mL of Ziziphus jujuba fruit lotion on their nipples and areolas 5 times a day after breastfeeding | 5 drops of their own milk on their nipples 5 times a day | Severity of pain | Ziziphus jujuba fruit lotion decreased nipple pain faster than breast milk. |
| Centuori, 1999 (28) | Italy | RCT | Nipple fissure | 219 | Instructed to avoid the use of nipple creams and other products | Routine nipple care | Sore and cracked nipples and breastfeeding duration | Nipple ointments had no significant effects on sore and cracked nipples and the duration of breastfeeding. |
| Mohammadzadeh, 2005 (29) | Iran | RCT | Nipple fissure | 225 | Lanolin locally on the nipple 3 times a day, and cleaned the nipple with a wet cloth before infant feeding | One group rubbed the hind milk on their nipples at the end of each breastfeeding session, another group did not use anything | Sore nipple | The healing time in the lanolin group was longer than the breast milk group |
| Mirzaie, 2018 (30) | Iran | RCT | Mothers with premature infants | 74 | Foot massage once daily for 7 days 10 min for each foot including general massage of the soles for the first 5 min | Massage in an unrelated area | Milk volume | On the 7th day of massage, a greater increase in milk volume was observed in the intervention group than in the control group [median (Q1, Q3) 7 mL (4.5, 10) vs. 1 (- 1, 2), P < 0.001]. |
| Susilawati, 2017 (31) | Indonesia | Quasi-Experimental | Breast engorgement | 34 | Giving milk with katu leaf and yeast | Massage | Pain, fever, feeling satiety | - Breast engorgement was observed in 82.4% of mothers who used conventional massage methods.- None of the mothers who performed breast treatment with katu and yeast experienced breast swelling, fever, or pain. |
| Dehghani, 2017 (32) | Iran | RCT | Breast engorgement | 94 | The Oketani massage | Routine care | Severity of engorgement | While a reduction in the mean severity of engorgement was observed in the right and left breasts of females in both the Oketani massage and control groups, the reduction was significantly larger in the the Oketani group. |
| Demirci, 2016 (33) | The US | RCT | Mothers with late preterm and early term infants | 11 | Herbal supplement | Meditation | Milk volume, tracked daily breastfeeding behavior | Mothers of late preterm and early term infants who perceived their breast milk insufficient reported the use of herbal supplements (i e, complementary medicine) as safe and useful methods to increase milk supply. |
Characteristics of the Studies Included in the Current Systematic Review
| Study Ref. | Luo (11) | Witt (16) | Meng (18) | Heberle (19) | Chiu (20) | Foda (21) | Khosravan (22) | As’adi (23) | Marrazzu (24) | Zhao (25) | Akbari (26) | Shahrahmani (27) | Centuori (28) | Mohammadzadeh (29) | Mirzaie (30) | Susilawati (31) | Dehghani (32) | Demirci (33) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Title and abstract | ||||||||||||||||||
| a | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| b | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Introduction | ||||||||||||||||||
| Background | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Objectives | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Methods | ||||||||||||||||||
| Study design | - | + | - | + | + | + | + | + | + | + | + | + | - | + | + | + | + | + |
| Setting | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Participants | + | + | + | + | + | + | + | + | + | + | + | + | + | + | - | + | + | |
| Variables | + | + | + | + | + | + | + | + | + | + | + | + | - | + | + | + | + | + |
| Measurements | + | + | + | + | + | + | + | + | + | + | + | + | - | - | + | + | + | + |
| Bias | + | + | - | + | + | + | + | - | - | + | - | + | - | - | + | - | + | - |
| Study size | + | + | + | + | - | + | + | - | + | + | + | + | + | + | + | - | + | + |
| Quantitative variables | + | + | + | + | + | + | + | + | + | - | + | + | + | + | + | - | + | + |
| Statistical methods | + | + | + | + | + | + | + | + | + | - | + | + | + | + | + | - | + | - |
| Results | ||||||||||||||||||
| Participants | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | - | - | + |
| Descriptivedata | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Outcome data | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | - | + | + |
| Main results | + | + | + | + | + | + | + | + | + | + | + | + | - | + | + | + | + | + |
| Discussion | ||||||||||||||||||
| Key results | - | + | + | + | + | + | + | + | + | - | + | + | + | + | + | + | + | + |
| Limitations | - | + | - | - | - | - | - | - | + | - | - | + | - | + | + | - | + | + |
| Interpretation | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | - | + | + |
| Generalizability | + | + | + | + | + | - | + | + | + | + | - | + | - | + | + | + | + | + |
The Adherence of the Selected Studies to STROBE Checklist
The most common breastfeeding problems in the studied females were milk stasis, breast engorgement, nipple fissure, and plugged ducts. A premature infant or an infant without desirable weight gain were also common complaints of breastfeeding mothers (Table 1).
According to the results of the current review study, point massage was beneficial to prevent low milk supply postpartum. The Oketani breast massage significantly increased total solids, lipids, and casein content, as well as the gross energy of breast milk and thus improved its overall quality. Reflexology enhanced breast milk supply. The Guasha therapy, the Oketani massage, and hollyhock leaf compress decreased the mean severity of breast engorgement. The six-step recanalization manual therapy (SSRMT) could be used as a safe and low-cost method to treat plugged milk ducts after delivery. Nipple fissures were relieved using Pistacia atlantica resin, silver impregnate medical cap, lanoline, menthol essence, and Ziziphus jujuba fruit.
4. Discussion
According to the reviewed studies, appropriate breast massage during the postpartum period could prevent milk stasis by decreasing the probability of low milk supply and improving milk discharge, and enhance blood circulation in the breasts and stimulate the nipples and mammary gland ducts. It also increases oxytocin release from the anterior pituitary and promote lactation through the reflex spray. Breast massage is also widely applied to relieve breast engorgement in puerperal milk stasis (34).
In Japan, the Oketani breast massage is used to relieve breast pain and engorgement and treat inverted nipples. Studies show the higher efficacy of the Oketani massage compared with conventional care in the reduction of breast engorgement during the first days after delivery (32). When applied before lactation, the Oketani breast massage can promote the secretion of oxytocin and prolactin and improve the overall quality of the produced milk by increasing its total solids, lipids, and casein content, as well as its gross energy. The higher energy supply to the hungry infant enhances their mood and sleep patterns and promotes their physical and mental development (35, 36). The significance of elevated gross energy levels increases as the infant grows and needs greater energy. Higher lipid and total solid contents of milk following breast massage also improves milk taste and increases infants’ satisfaction. Other studies also reported changes in milk composition- e.g. increased concentrations of protein, saccharide, lipids, and trace nutrients- following the Oketani massage (21). In a study on lactating females, Ohno found that the Oketani massage increased the mean level of a small peptide by 22%. Although the potential physiological function of this peptide was not clear, the author suggested that the connective tissue massage probably stimulated a specific protease activity, which resulted in the degradation of a larger peptide or protein into the mentioned small peptide. Ohno also reported a significant reduction in lipoxygenase activity following oketani massage and concluded that this complementary technique could promote infant development (37).
The reviewed studies also highlighted the beneficial effects of point massage of the liver and stomach channel; e.g. Rugen point (ST18), Dan Zhong point (CV17), and Shao Ze point (SI1), on the promotion of lactation initiation. Pressure on the ST18 point, located on the breast, is reported to enhance lactation and resolve other breast issues such as mastitis and pain. Pressure on the CV17 point is known to enhance Qi regulation of Qi, improve blood circulation, and ultimately promote lactogenesis. Pressure on the SI1 point acts as a lactagogue, since it regulates heart Qi and increases milk discharge. These effects can be promoted if both SI1 and CV17 are stimulated (38). Thermography is widely used as a safe and reliable method to diagnose breast engorgement. The application of this method on lactating females with glandular breast engorgement revealed that breast temperature increased with the increasing severity of engorgement and intensity of swelling (19).
Another technique used to treat breast engorgement is the Guasha therapy. This method, developed based on the Chinese principles of meridians and collaterals, is widely used by Asian traditional medicine practitioners to promote external and internal blood flow, improve blood production, and enhance the dissemination of fluids (39). Chang and Chang attributed the pain killing effects of the Guasha therapy and its efficacy in relaxing tight muscles. Moreover, it was observed that the stimulation of skin nerve endings by Guasha evoked the self-reflex of the breasts and thus enhanced partial and overall blood circulation and decreased pain (40). The Guasha therapy can be adopted as a simple, time-effective, and low-cost method to treat lactation-related breast issues with minimum levels of discomfort (20)
A variety of herbal medicines are used to treat breast engorgement (22, 41). The topical application of hollyhock leaves in combination with both warm and cold compresses alleviates the symptoms of breast engorgement during breastfeeding (22). Moreover, adding cactus and Aloe cold compress to a massage intervention enhanced its efficacy in breast hardness and pain reduction. Such beneficial effects could be attributed to the natural active ingredients - e.g. Aloe polysaccharides (42, 43) and cactus alkaloids (44, 45), in these two plants. Due to its ability in detoxification and relief of swelling and stasis, cactus is widely applied as a topical treatment of mumps (46). Meng et al. reported that the use of Aloe and cactus pulp lubricated the skin and improved the efficacy of massage therapy to reduce pain and discomfort (18). Another study reported the application of katu-yeast to eliminate the incidence of breast swelling and pain, fever, and discomfort and decreased breast engorgement (31).
Since nipple fissures and soreness are the second leading cause of early cessation of breastfeeding and the main cause of tendency toward the use of formula (47), treating these conditions is essential to ensure successful breastfeeding (48) and prevent further problems including mastitis and abscesses (49). Therefore, several studies focused on various methods of alleviating nipple problems. For instance, a comparison between breast milk and Pistacia atlantica resin ointment showed that the latter was more effective in decreasing the severity of nipple fissures. Haghdoost et al. found Pistacia atlantica resin more effective to treat burn wounds. They suggested greater levels of fibroblast and platelet-derived growth factors and enhanced angiogenesis responsible for the observed effects (50). Other studies highlighted the potent anti-inflammatory and anti-microbial effects of menthol essence and its beneficial effects on nipple fissures (51, 52). Menthol exerts its anti-inflammatory effects and releases the intracellular components by attacking and destroying the cytoplasmic membrane of inflammatory agents and microorganisms. It can also prevent cell damage by inhibiting the electron transport process and facilitating nutrient absorption, nucleic acid production, and ATPase activity (53). Marrazzu et al. evaluated the effects of a silver-impregnated medical cap and concluded that the cap could relieve the painful symptoms of nipple fissures more effectively than the standard care (24). A study on ointments containing lanolin, an oily colorless agent comprising lana wool and oleum oil, identified appropriate breastfeeding as the most important factor to treat sore nipples. It also found the positive effects of breast milk on sore nipple treatment to surpass those of lanolin (29). In a study by Shahrahmani et al., the mean intensity of nipple pain on the 4th and 7th days after delivery was significantly lower in the group treated with Ziziphus jujuba fruit lotion than the ones receiving conventional treatment with breast milk. The authors reported the flavonoids, steroids, fatty acids, epicatechin, vitamins A and C contents of Ziziphus jujuba fruit as the cause of its analgesic and anti-inflammatory effects (27).
According to the reviewed studies, SSRMT could be used as a safe and low-cost method to treat plugged milk ducts after delivery. SSRMT is a manual method and an instance of integrative medicine based on a combination of basic traditional Chinese medicine, the anatomy of milk ducts, physiology of milk ejection, and massage mechanics. Although the short-term results in previous studies were promising, a comprehensive review of the terminology, pathophysiology, and diagnosis of plugged ducts and other available therapeutic methods for the condition is required to clarify the strengths, weaknesses, and potential applications of SSRMT (25). Reflexology is another technique reported to enhance milk supply and decrease formula use. Mirzaei et al. observed an increased milk supply following foot reflexology massage in mothers of premature infants (30). Complementary medicine techniques can be used as low-risk and cost-effective methods to resolve breastfeeding-associated issues in mothers with premature infants.
5. Conclusions
Complementary medicine techniques - e.g. the use of herbal supplements, massage/point massage, and reflexology- can be applied as low-risk, safe, and cost-effective methods to encourage exclusive breastfeeding and create an overall sense of well-being. These methods might be able to effectively resolve the breastfeeding-associated issue without the need for any pharmacological or chemical interventions. Nevertheless, further randomized studies are warranted to compare the efficacy and safety of such techniques with those of other available therapeutic methods. It seems that the study tried to reach a conclusion on the benefits of complementary medicine in breastfeeding based on studies conducted in recent years. Authors believe that the fewer side effects and the more cost-efficacy, these methods encourage mothers and families to use these methods and researchers to do more in this field. According to the conditions and culture of Iranian females, the use of herbal remedies such as lanolin, Ziziphus jujube, peppermint, etc., or special massage by husband or relatives of lactating females or health providers are suggested.
5.1. Limitations
The current review study had a number of limitations including its focus on English and Persian articles and the low methodological quality and very small sample size of some of the selected articles.