1. Background
The survival rates of preterm infants has increased over the last years (1-5), but oral feeding difficulties are the most common problems encountered by them (4, 6). These difficulties may negatively affect attainment of independent oral feeding and lead to prolonged hospital stay, family stress, long- term health problems and financial costs (7, 8). Caregivers and speech language pathologists that work in the NICUs may use various oral stimulation techniques to facilitate oral feeding of preterm infants (9). NNS and pre-feeding oral stimulation are among the most common stimulation techniques in use. These interventions have been proved to be beneficial for oral feeding skills, attainment of full oral feeding, weight gaining and reducing the length of hospital stay (10, 11). Due to a lack of empirical evidence, caregivers in NICU, while aware of the feeding difficulties of these infants, are confused about the kind of intervention which is more effective.
2. Objectives
The aim of this study was to compare the effects of NNS and pre-feeding oral stimulation program on feeding performance, length of hospital stays, weight gaining.
3. Patients and Methods
According formula, Thirty-two preterm infants (16 males and 16 females) from NICU at Kamali Hospital (Karaj, IR Iran) participated in the study. In this interventional research with convenience sampling, a random assignment was performed using a simple randomization method. The following inclusion criteria were considered: preterm infants from 26 to 32 weeks of gestational age that fed through a tube and their birth weight were 1000 to 2000 grams. Gestational age is the common term used from the first day of the woman's last menstrual cycle to the current date. Infants were excluded if they had congenital anomalies, chronic medical complications, asphyxia, third or fourth degree intracranial hemorrhages, necrotizing enterocolitis, metabolic disorders, genetic syndromes, oral-motor defects, neurological disorders, umbilical catheter, medication (aminophylin, analgesic), intra uterine growth pattern documented by a neonatologist. The study was performed between January and June 2012. The study was approved by the Institutional Review Board for Human Subjects Research of University of Social Welfare and Rehabilitation Sciences. Informed consent was obtained from parents before their infants entered into the study.
3.1. Procedure
The infants were randomly using a simple randomization assigned into NNS (n = 11), pre-feeding oral stimulation (n = 10) and control (n = 11) group. The NNS program consisted of thrice daily stroking of the palate for 5 minutes to elicit a suck. This intervention delivered by one speech therapist who was blinding to research and was performed through introduction of the little finger in infant’s oral cavity to gently stroke the palate to elicit a suck. NNS stimuli were started during initial 5 minutes of tube feeding and were administered for 10 consecutive days. Details of the program can be found in Harding et al. study (12). Pre-feeding oral stimulation was performed by the same speech therapist. The oral stimulation program consisted of once daily stroking of cheeks, gums and tongue and followed by 3 minutes of non-nutritive sucking for 15 minutes. The exact stimulation program can be found in Fucile et al. study (13). The control group received sham intervention. For this group, the same speech therapist placing her hands in the incubator without touching the infant for 15 minutes and 10 consecutive days. Therefore, all infants received the same duration for each intervention and all interventions were delivered by one person.
3.2. Outcomes
The primary outcome of study was the time needed to attainment of independent oral feeding. Independent oral feeding was defined as introduction to 8 successful oral feeding per day for 48 hours. Furthermore, gestational age of infants was calculated during 1, 4 and 8 oral feeding per day (Feeding parameters of infants). The secondary outcome was length of hospital stay that was defined as date that infant born to date of discharge from the hospital. Weight gaining was another outcome that was measured by recording the weight every day by a nurse in NICU by using a digital balance at 8 am (A digital scale sensitive to 1 g (seca 334, Mobile digital baby scale, CE 0123). Introduction of oral feeding occurred according unit’s routine when the preterm infants were clinically stable.
3.3. Statistical Analyses
Statistical analyses were performed using SPSS16.0 statistical software. Kolmogorov-Smirnov test revealed continuous variables to be normal, so parametric tests were used. An ANOVA was performed followed by Scheffé's method to compare 3 groups (NNS, pre-feeding oral stimulation and control group) for the gestational age at different stage of oral feeding. Repeated measures ANOVA were performed to analyze intra-group changes. A MANOVA was performed to compare the weight gains from birth through weeks between three groups. Statistical significance was considered at α = 0.05.
4. Results
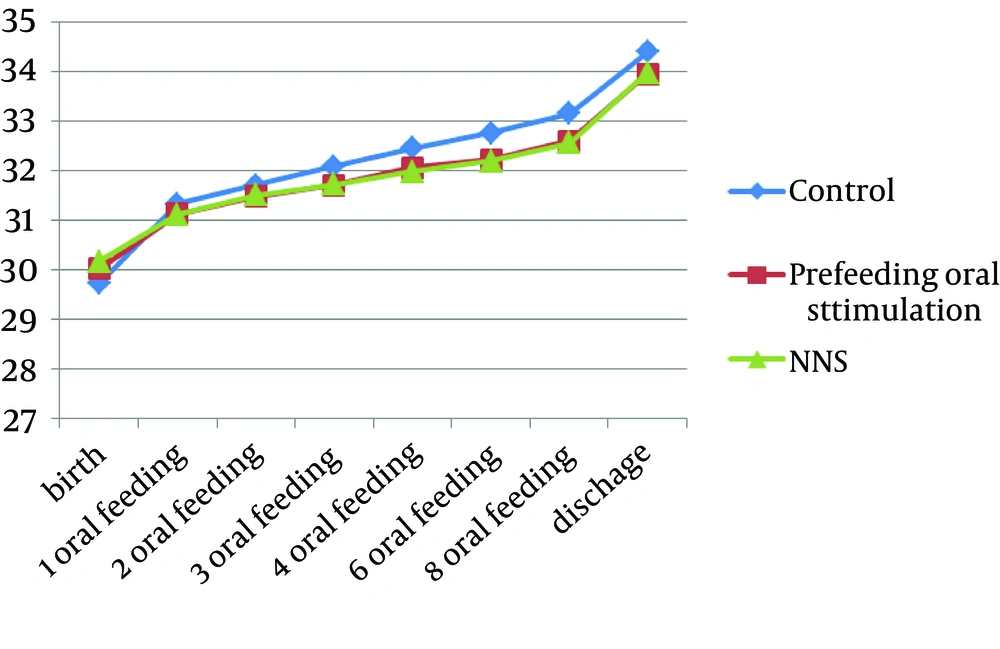
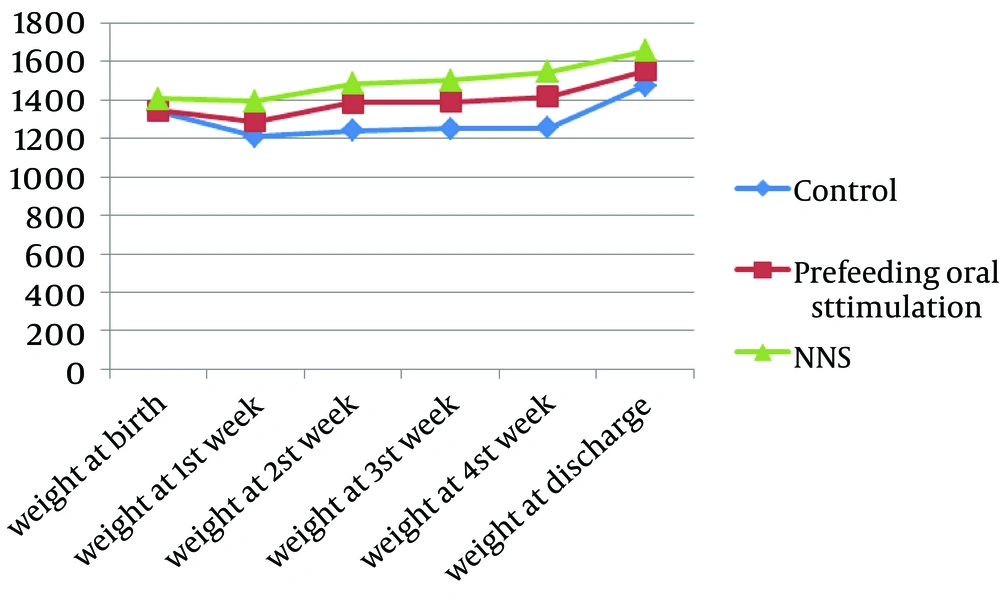
There was no significant difference in regard to gestational age, birth weight, gender distribution and Apgar score between 3 groups (Table 1) in pre-test stage. While the gestational age of independent oral feeding in both intervention groups was lower than control group (Figure 1), the analyzes revealed no significant difference in the gestational age between three groups (P > 0.05). Also weight of the groups obtained through time (Figure 2). The average days of life for independent oral feeding in NNS and pre-feeding oral stimulation were 16.72 ± 8.94 and 18.20 ± 9.18 day respectively, while the control group was 24.27 ± 9.42 day. Although the NNS and pre-feeding stimulation groups reached 7.55 and 6.07 days sooner to independent oral feeding than in the control group, but the difference did not reach statistical significance. Preterm infants in the intervention (NNS and pre-feeding oral stimulation) and control groups did not differ statistically in regard to attainment of 1, 4, and 8 oral feeding per day (P > 0.05).
| NNS | Pre-Feeding Oral Stimulation | Control | P Value | |
|---|---|---|---|---|
| 30.18 ± 1.77 | 30.01 ± 1.76 | 30.29 ± 1.95 | 0.844 | |
| 1406.36 | 1343.01 | 1393.63 | 0.58 | |
| 0.913 | ||||
| Male | 6 | 5 | 5 | |
| Female | 5 | 5 | 6 | |
| 7.85 ± 2.17 | 7.55 ± 1.997 | 7.78 ± 2.24 | 0.58 |
aAbbreviation: NNS, non-nutritive sucking.
Also no significance difference were found in the length of hospital stay between the three groups (P > 0.05), but the average length of hospital stay in the control group was higher than in the intervention groups ( 26.54 ± 12.48 days for NNS group; 27.60 ± 12.57 days for pre-feeding oral stimulation group; and 33.45 ± 13.46 days for control group). In relation to the weight at discharge, ANOVA revealed a significant difference between three groups (F = 5.956, df = 29, P = 0.007) (Table 2). Scheffes method showed that the difference was related to means of NNS and control group.
| NNS | Pre-Feeding Oral Stimulation | Control | P Value | |
|---|---|---|---|---|
| 1654.54 ± 133.29 | 1553.01 ± 140. 55 | 1472.72 ± 94.34 | 0.007* |
aAbbreviation: NNS, non-nutritive sucking.
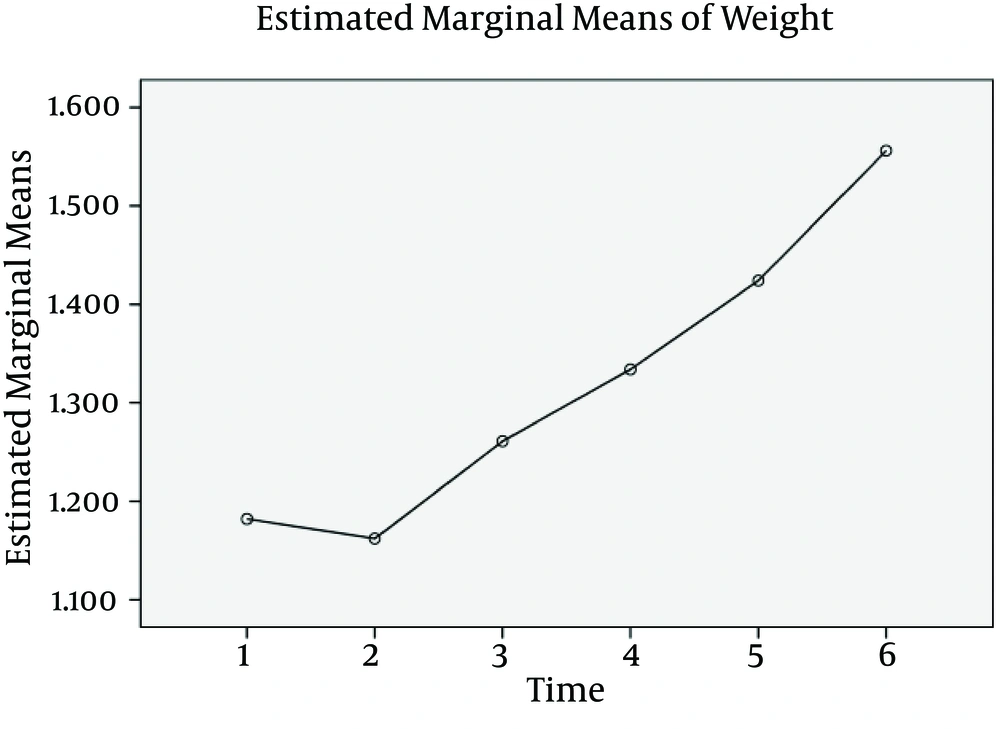
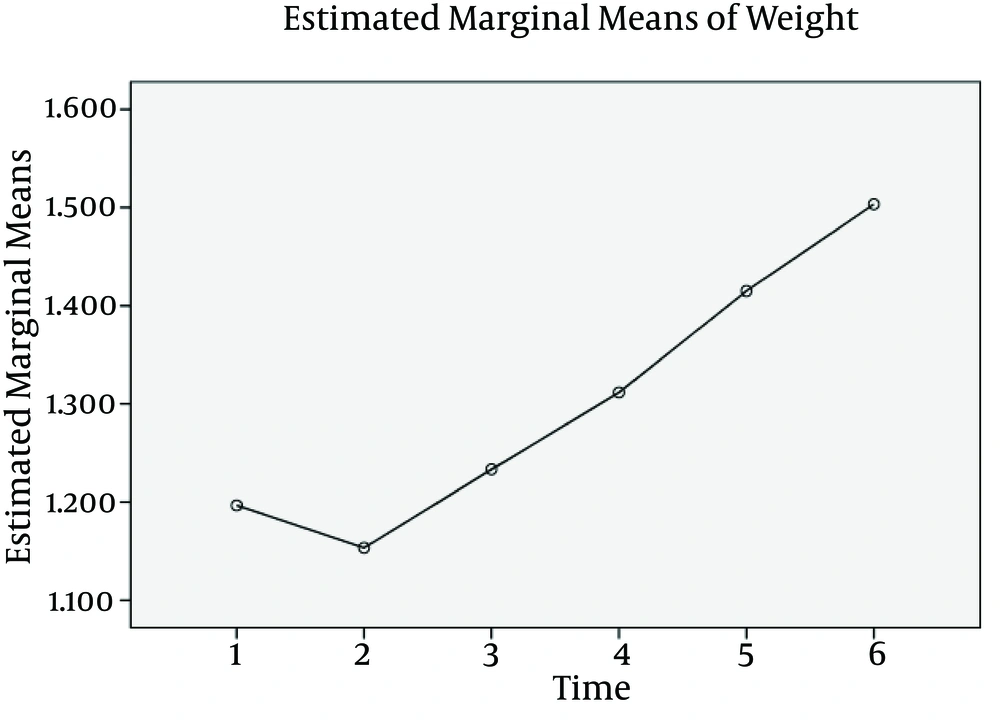
Using a repeated measures ANOVA with a Greenhouse-Geisser correction, the mean scores for weight changes in NNS group were statistically significantly different (F (1.984, 7.934) = 28.086, P < 0.0005). The results of the Bonferroni post hoc test revealed that the difference between the times 1 and 6 (1182 ± 50.73 gr. Vs 1556 ± 24.00 gr.), 2 and 3 (1162 ± 50.23 gr. Vs 1261 ± 52.78 gr.), 2 and 4 (1162 ± 50.23 gr. Vs 1334 ± 46.00 gr.), 2 and 5 (1162 ± 50.23 gr. Vs 1424 ± 37.36 gr.), 2 and 6 (1162 ± 50.23 gr. Vs 1556 ± 24.00 gr.) were significantly different (P < 0.05) (Figure 3). For pre-feeding oral stimulation group a repeated measures ANOVA with a Greenhouse-Geisser correction, revealed that the mean scores for weight changes were statistically significantly different (F (1.321, 6.604) = 22.568, P < 0.001). The results of the Bonferroni post hoc test revealed that the difference between the times 2 and 3 (1153 ± 34.22 gr. Vs 1233 ± 37.47 gr.), 2 and 4 (1153 ± 34.22 gr. Vs 1312 ± 45.12 gr.), 2 and 5 (1153 ± 34.22 gr. Vs 1415 ± 50.38 gr.), 2 and 6 (1153 ± 34.22 gr. Vs 1503 ± 45.94 gr.), 3 and 5 (1233 ± 37.47 gr. Vs 1415 ± 50.38 gr.), 3 and 6 (1233 ± 37.47 gr. Vs1503 ± 45.94 gr.), 4 and 6 (1312 ± 45.12 gr. Vs1503 ± 45.94 gr.) were significantly different (P < 0.05) (Figure 4).
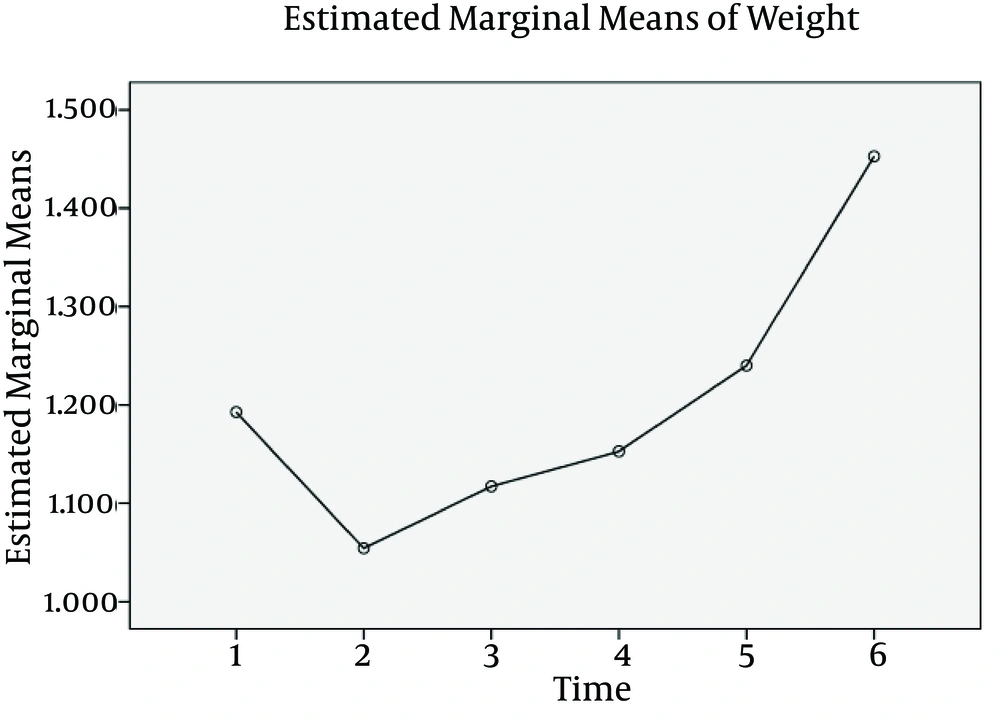
A repeated measures ANOVA with a Greenhouse-Geisser correction, showed that the mean scores for weight changes in control group were statistically significantly different (F (2.488, 14.927) = 26.021, P < 0.0005). The results of the Bonferroni post hoc test revealed that the difference between the times 1 and 6 (1193 ± 45.55 gr. Vs 1453 ± 28.59 gr.), 2 and 5 (1054 ± 23.38 gr. Vs 1240 ± 39.03 gr.), 2 and 6 (1054 ± 23.38 gr. Vs 1453 ± 28.59 gr.), 3 and 6 (1117 ± 25.51 gr. Vs 1453 ± 28.59 gr.), 4 and 5 (1153 ± 29.09 gr. Vs 1240 ± 39.03 gr.), 4 and 6 (1153 ± 29.09 gr.Vs1453 ± 28.59 gr.) were significantly different (P < 0.05) (Figure 5).
The MANOVA test revealed no significant difference in weekly weight gain between three groups (F (12, 20) = 0.904, P > 0.05; Wilk’s lambda = 0.420, partial Eta squared = 0.325).
5. Discussion
NNS and pre-feeding oral stimulation strategies are widely used to accelerate the independent oral feeding of preterm infants. However, which the intervention is most effective, is not yet understood. This study continued to confirm the benefits of oral stimuli techniques applied to preterm infants and to determine which of them is most effective. The results of our study indicated that the NNS and pre-feeding oral stimulation program had a beneficial effect on the time needed to attainment to different stage of oral feeding and independent oral feeding. The preterm infants in NNS and pre-feeding oral stimulation groups reached 7.55 and 6.07 days sooner than control group to these criteria. Therefore in term of performance in oral feeding, NNS program seemed to be more beneficial than pre-feeding oral stimulation and pre-feeding oral stimulation was more fruitful than shame intervention. Although statistically not significant, our results were similar to Lessen et al. (14), Fucile et al. (13), Rocha et al. (15), who confirmed the beneficial effects of two interventions in attainment to oral feeding (a result which is of great clinical and economic importance). Also several studies did not find any improvement in independent oral feeding (10, 16). These differences may result from different administrations of stimulation protocol or small sample size that affected the achievement of statistical significance. Our finding suggested that NNS program compared to pre-feeding oral stimulation program improved weight gaining at discharge time. These results was in contrast to the study from Lyu et al. (17) and in line with those of Bernbaum et al. (18). This difference may be explained by the different method used by these studies. In general newborns in NNS and pre-feeding oral stimulation groups discharged sooner than control group. This findings (although not statistically significant) agree with Fucile et al. (19) and is in contrast to previous studies, which reported that oral stimulation decreased length of hospital stay (15, 20). Our study had several power and weakness. For example, medical events and lack of exact protocol for discharge may lead prolonged the length of hospital stay. The implementation of specific protocol for discharge may have allowed for better discrimination between groups and reduce these weakness.
Furthermore, another weakness of our study was small sample size. For future studies, we propose to recruit a larger sample size to increase the possibility of an achievement of statistical significance.
In conclusion, although our finding not showed significant differences between groups in independent oral feeding (may be for small sample size) but results emphasized the importance of NNS for improvement of weight gain in preterm infants. Also, we have demonstrated that both NNS and pre-feeding oral stimulation may contribute to the improvement of independent oral feeding. Since these interventions have beneficial effects on preterm infants weight gaining and independent oral feeding, we offer the use of both interventions in NICU. Furthermore, NNS is more effective on weight gain. We may further propose that caregivers and speech language pathologist in NICU primarily use NNS because of its simplicity and safety for using by parents and NICU staff.