1. Background
Cerebral palsy (CP) is the most common cause of childhood disability (1). CP is the result of damage to growing central nervous system during fetal development, during delivery, or in the first 2 years of life (2). CP can manifest motor and cognitive symptoms and epilepsy. According to its motor effects, it is divided into pyramidal and extra-pyramidal groups. Pyramidal or spastic type, being the most common type, is associated with muscle stiffness (3).
Spasticity causes the children to lose flexibility, range of motion (ROM) and muscle strength with increasing age (2). Decreased ROM is a common secondary problem caused by abnormal muscle tone and longtime static position of CP children. This is one of the concerns in the treatment; therefore, ROM monitoring in upper and lower extremities of CP children becomes essential (4).
Muscle stretching can alter muscle characteristics such as structure, irritability, and visco-elastic properties. The purpose of spastic muscle stretching in CP children is tone normalization, pain reduction, increasing function, maintaining and increasing the soft tissue flexibility (5) as well as maintaining and increasing the existing ROM (6).
In addition to passive stretching exercise, there are currently several treatments to reduce spasticity including oral pharmacologic agents, physical modalities, Botox injection, intrathecal agents, and surgery. One of the new ways to reduce spasticity in children with CP is whole body vibration (WBV) (2).
Although the use of WBV has gained popularity in rehabilitation, but its short-term and long-term effects are still under investigation. Many researchers reported that muscle spindle and alpha motor neurons are stimulated by vibrations leading to muscle contraction. The short-term effects of therapeutic vibration include increasing the oxygen consumption, muscle temperature, skin blood flow, muscle strength, and insulin levels (3).
Lee and Chon examined parameters of gait and muscle thickness of lower extremities after 8 weeks of using WBV in 30 CP children and reported that WBV is effective in improving walking speed, increasing step length and angle of ankle, possibly due to the positive effects of WBV on muscles of lower extremities because the thickness and strength of dorsiflexor and plantarflexor muscles had increased (7). El-Shamy explored the effect of WBV to improve balance and muscle strength of 30 CP children with spastic diplegia and reported that WBV improves muscle strength and balance in children with CP diplegia (8). Duquette et al. in a systematic review reported that WBV has the potential to improve coordination, muscle strength and reduce spasticity in CP (3). However, high quality studies in this field are limited.
2. Objectives
The mechanism of improvement caused by WBV as a new treatment for children with CP which affects mobility, balance, function, and gait in these children, is not clear yet. There are few studies that investigated the effect of WBV on ROM. In this study we aimed to evaluate the effectiveness of WBV on the passive range of motion (PROM) and active range of motion (AROM) of lower extremities joints and walking speeds in spastic CP children.
3. Methods
3.1. Participants and Study Design
The data was collected in summer of 2017. Families of CP children referred to the Neuromuscular Rehabilitation Research Center, Semnan, Iran, were invited to participate in the study. Twenty CP children participated. The mean and standard deviation of children’s age in the control group was 8.1 ± 1.93 and in the intervention group was 6.9 ± 2.46. Mean of BMI in the control group was 14.13 ± 3.3 and in the intervention group 14.6 ± 4.02. The two groups did not have a significant difference in BMI (P > 0.05).
The control group consisted of 6 hemiplegic and 4 diplegic children and the experimental group of 6 diplegic, 3 hemiplegic and 1 quadriplegic children. In both groups there were two children with GMFCS level 1, five children with GMFCS level 2 and three children with GMFCS level 3.
Participants in this single-blind randomized clinical trial study, were selected by convenient sampling. Inclusion criteria were: CP diagnosis of children, age between 4 to 12 years, ability to walk without falling or without walking aids, ability to follow orders and to be at the level of 1, 2 and 3 of The Gross Motor Function Classification System (GMFCS). Exclusion criteria included: any severe or progressive disease, presence of musculoskeletal contracture in lower extremity joints, history of lower extremity surgery in the last 6 months, having a history of rhizotomy or tendon-release, nonunion fracture, uncontrolled seizure, botulinum toxin injections in the last 3 months, and limitation in knee ROM more than 10 degrees.
Ethical approval was obtained from the Semnan University of Medical Sciences, (IR. SEMUMS.REC.1395.6). The trial was registered with www.http://fa.irct.ir/: IRCT20160405 21686 N2.
3.2. Instruments
3.2.1. Modified Ashworth Scale (MAS)
This easy practical scale can be used manually to determine resistance of muscle to passive stretch in spasticity evaluation in knee joint (9). Clopton et al reported the validity of this scale good in hyperton flexor muscles of elbow in CP children in 2005. Intera-rate and inter-rate reliability of this test was reported moderate to good in 38 spastic CP children in 2008 (10).
3.2.2. Goniometry
For measurements, children`s lower extremities were exposed to allow access to bony landmarks. PROM was measured 30 to 60 seconds after a slow static stretch and in this measurement the limb was hold with low force at the end of ROM [6]. AROM was assessed after 3 seconds holding the limb in the end of ROM (11). Each measurement was performed 3 times and the mean of 3 measurements was recorded as ROM. A 180 degrees goniometer and a 360 degrees goniometer were used to assess the PROM and AROM of the hip, knee and ankle joints movements. In order to assess abduction and flexion of hip joint, the child lay in supine position. In assessment of knee extension ROM and plantarflexion and dorsiflexion ROM, children were placed in sitting position (12).
3.2.3. Six-Minute Walk Test
This test is used to assess children’s walking speed. That way, the distance that a person walks within 6 minutes is measured. In this test, a distance of 7 meters is determined for walking and the subject is asked to walk on it without interruption and turn back at the end of it and keep walking until 6 minutes and the therapist says standard words of encouragement (1). Standard words including “very good” and “continue” were repeated every 30 seconds (13). The reliability of this test has been reported in CP children aged 3 to 18 years, from good to excellent (ICC = 0.98).
3.3. Data Collection
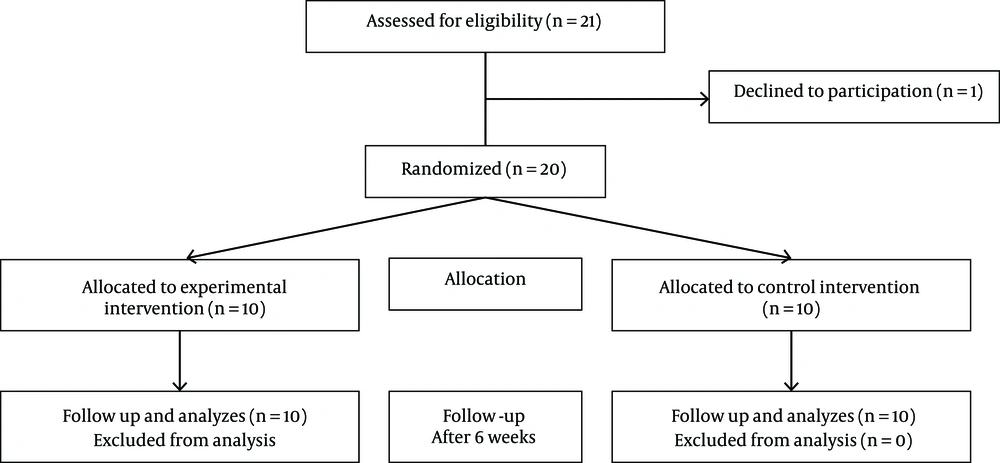
Twenty-one CP children from the age group of 4 to 12 years having inclusion criteria entered the study. One child was excluded due to parent`s reluctance to continue intervention. These children were divided into intervention and control groups in terms of GMFCS by stratified random sampling method. The intervention group received passive static stretching with standing on the power on WBV while the control group received passive static stretching with standing on the power off WBV. WBV device used in this study was the USA Plate Power. The exercises were performed 3 times a week and lasted for 6 weeks. Exercises in two groups were conducted by a graduated occupational therapist. In this single blind study, the assessor was an expert occupational therapist who was not aware of participants’ grouping in order to reduce the potential for bias.
The study was conducted after approval by the Ethics Committee of Semnan University of Medical Sciences. The ethical number is IR.SEMUMS.REC.1395.6 and the registration number in Iranian randomized clinical trial center is IRCT2016040521686N2. Initially, researchers explained the goals and method of the research to parents of CP children, then consent forms were signed by parents and the assessments were started (Figure 1).
Stretching exercises for both groups of children consisted of 2 minuses passive stretching of hip flexor, hip adductor, hamstring muscles and plantar flexor muscles for 40 seconds repeated for 3 times (6). Hamstring muscle stretching: The child was placed in supine position, one leg was kept while the hip and knee were extended and the other hip joint was in flexion position with extended knee. Cuff muscle stretching: The child was in a supine position, knees were extended and the ankles were in dorsiflexion position. Iliopsoas muscle stretching: The child lay in supine position. One leg was kept while the hip and knee were extended and the other knee and hip joints were flexed toward the abdomen. Hip adductor muscle stretching: The child was in supine position with extended knees. Then the therapist kept one leg along the hip joint and abducted the other leg (14).
In the intervention group, after stretching exercise, children were placed on the WBV device using frequency of 20 to 24 Hz and amplitude of 2 mm, with a 30 degrees flexed knee, and asked to take the supporting bars of the device. The feet were placed in an equal distance from the center line of the device when standing (15). Children stayed in WBV for 3 minutes and then had a 3 minutes rest and this was repeated for 3 times. The total time of vibration children received was 18 minutes (16). The children in the control group stood on the power off WBV device for 18 minutes at each session after receiving the same stretching exercises.
Primary assessments were conducted in the first session before interventions started and secondary assessments were conducted in a meeting 1 day after the last session of treatment to avoid the immediate effect of intervention in increasing the ROM. In both primary and secondary assessments spasticity evaluation, ROM measurement and six minute walk test were conducted.
3.4. Data Analysis
Data were analyzed using SPSS software version 22. Given that the histogram and the Kolmogrov-Smirnov test indicated that the data had normal distribution, independent t-test was used to examine the difference between the two groups and the paired t-test to examine the differences within the groups before and after the intervention in the two groups. P value of less than 0.05 was considered statistically significant.
4. Results
Results of independent t-test revealed no significant difference between the two groups before the intervention (P > 0.05). As it is shown in Table 1, active hip abduction, knee extension and ankle dorsiflexion significantly increased in the experimental group (P < 0.05). The AROM and PROM of hip extension and flexion increased before and after intervention in both groups (P < 0.05). But there were no significant differences in PROM of ankle dorsiflexion and also in AROM and PROM of hip abduction in the two groups, and in the control group no significant change was found in active dorsiflexion, AROM and PROM of knee extension, and AROM of hip abduction (P > 0.05). As indicated in Table 1, stretching training combined with WBV was effective in increasing the 6-minute walk test significantly (P < 0.05).
| Variable/Group | Mean ± Standard Deviation | Effect Size | P Value | |
|---|---|---|---|---|
| Before | After | |||
| Active hip flexion | ||||
| Experimental | 72 ± 15.71 | 81.6 ± 20.09 | 0.98 | 0.03a |
| Control | 81.1 ± 10.03 | 98.6 ± 14.12 | 0.8 | |
| Passive hip flexion | ||||
| Experimental | 100.5 ± 22.22 | 110.55 ± 23.34 | 1.37 | 0.37 |
| Control | 112.6 ± 15.16 | 118.5 ± 14.49 | 1.39 | |
| Active hip extension | ||||
| Experimental | 10.25 ± 7.72 | 11.25 ± 7.72 | 0.65 | 0.12 |
| Control | 16.06 ± 7.02 | 18.3 ± 8.56 | 1.18 | |
| Passive hip extension | ||||
| Experimental | 21.6 ± 6.07 | 24.05 ± 5.79 | 1.18 | 0.86 |
| Control | 20.8 ± 7.50 | 23.06. ± 6.13 | 0.6 | |
| Active hip abduction | ||||
| Experimental | 25.6 ± 10.7 | 34.85 ± 5.32 | 1.02 | 0.04a |
| Control | 28.3 ± 7.65 | 28.5 ± 7.74 | 0.18 | |
| Passive hip abduction | ||||
| Experimental | 33.3 ± 11.83 | 38.15 ± 12.11 | 0.65 | 0.94 |
| Control | 38 ± 4.21 | 38.4 ± 4.5 | 0.43 | |
| Active knee extension | ||||
| Experimental | 113 ± 14.75 | 115 ± 15.63 | 0.52 | 0.32 |
| Control | 102.3 ± 21.89 | 106.05 ± 22.74 | 0.82 | |
| Passive knee extension | ||||
| Experimental | 133 ± 14.8 | 137.3 ± 14.42 | 0.42 | 0.1 |
| Control | 126 ± 10.74 | 128 ± 9.77 | 1.19 | |
| Active ankle dorsiflexion | ||||
| Experimental | 5.15 ± 3.71 | 18.45 ± 5.55 | 0.79 | 0.02a |
| Control | 7.2 ± 5.09 | 10.2 ± 8.57 | 0.7 | |
| Passive ankle dorsiflexion | ||||
| Experimental | 12.2 ± 4.49 | 20.65 ± 10.68 | 0.77 | 0.31 |
| Control | 14.6 ± 7.79 | 15 ± 9.28 | 0.17 | |
| 6 min walks | ||||
| Experimental | 158.8 ± 100.24 | 189.45 ± 115.47 | 0.9 | 0.04a |
| Control | 194 ± 78.82 | 271.5 ± 60.81 | 0.71 | |
aStatistically significant (P < 0.05)
Our study did not lead to any changes in the level of GMFCS and the severity of spasticity of knee muscles before and after the intervention (P < 0.05).
5. Discussion
The results of this study revealed that the use of WBV with stretching exercise could be effective in increasing the AROM of hip flexion, abduction, dorsiflexion of ankle, as well as increasing walking speed in CP children.
5.1. Hip Joint
WBV combined with stretching exercises for 6 weeks, can improve AROM in hip flexion and abduction. With this method, although AROM increased in hip flexion and abduction, PROM did not change significantly. The reason for increased AROM could be the improved strength of flexor and abductor muscles. Despite the importance of mobility in hip joint in gait and balance, there are few studies on the effect of WBV on hip ROM.
In line with this study, Krause et al. showed that WBV training increases maximal voluntary muscle activation in lower limb muscles (17). Lee and Chon used WBV with physical therapy for 8 weeks in CP children and concluded that WBV had no effect on the improvement of the hip joint flexion strength (7). In a similar study Tupimai et al. used stretching along with WBV training in 20 CP children and found that WBV had no significant effect on hip joint ROM (18).
Ahlborg et al. examined the effectiveness of two WBV methods and the resistance training on spasticity, strength, and gate parameters in fourteen 21 - 41 years old CP adults. After 8 weeks of intervention, they found that WBV had more effect on reduction of hip abductor spasticity than resistance training. They also reported that the muscles strength of lower extremities had increased in both groups (19), which is consistent with the results of our study.
5.2. Knee Joint
In this study AROM and PROM of knee extension did not significantly change. Along with this study, Dickin et al. (2) and Lee and Chon (7) found that WBV does not increase knee joint PROM and AROM of CP children. Song et al. reported that spasticity in knee flexion and extension did not decrease after WBV training followed by conventional physiotherapy (50 min per day, 12 days per month) (20). But El-Shamy reported that WBV in CP children leads to an increase in the strength of knee extensor muscles (8). Cheng et al. (11), Krause et al. (17), and Tupimai et al. (18) also reported an increase in knee ROM by using WBV. One reason for such finding in our study is that the spasticity did not significantly change in quadriceps and hamstring muscles. However, considering different results of studies on the effect of WBV in the knee joint, further investigation is needed.
5.3. Ankle Joint
In this joint, only AROM of dorsiflextion in the intervention group increased significantly. Therefore, it seems that WBV has led to an increase in strength or activation of dorsiflexor muscles. The results of our study were in line with the study of Tupimai et al. who reported that passive muscle stretching combined with WBV could increase ankle dorsiflexion ROM (18). Dickin et al. also reported the effect of WBV on improvement in dynamic ROM due to decrease in muscle tone of triceps surae. By decreasing of this muscle tone, tibialis anterior can increase ankle ROM (2). Lee and Chon also reported that using WBV is effective in improving muscle strength of ankle joint. Song et al. found that WBV training improves tibialis anterior muscle activity and decreases spasticity in plantar flexor muscles (20).
5.4. Walking Speed
Our study showed that stretching training with WBV leads to increased walking speed in CP children. Other studies too have indicated that WBV is effective in improving the strength and coordination of muscles (3). In our study, AROM of hip flexion and abduction increased in the intervention group which can be the result of increased flexor and abductor muscles strength which effects on the swing phase of gait and leads to improved balance and increased walking speed. In this regard, some studies have also reported that WBV can result in increased muscle strength (8).
Lee and Chon found similar results in their study and found WBV effective in improving walking speed, step length, and cycle time (7). Several studies have reported that the use of WBV device increased the speed of walking in CP children effectively (18, 20, 21). Saquetto et al., in a systematic review on the effects of WBV, reported that this device increased the speed of walking and improved functional standing in CP children (22). Duquette et al. (3) and Sa-Caputo et al. (23) in their systematic reviews also found that WBV increased walking speed and muscle strength. After 12 weeks of intervention, Ibrahim reported that the WBV resulted in increased walking speed, muscle strength and gross motor skills in CP children (24).
5.5. Spasticity
Our study results indicate that six weeks of stretching exercises alone and in combination with WBV would not change the severity of spasticity in knee muscles in CP children. Also Sa-Caputo et al. in their systematic review, did not find this method an effective way of reducing spasticity (23). Park et al. examined the effect of one session WBV on spasticity on 17 CP children and reported that spasticity in the ankle plantar flexors had decreased using Ashworth and Tardieu scale and this reduction in spasticity maintained up to two hours after using WBV (25). One explanation for this finding can be the length of assessment time. In our study we investigated the short term effect of WBV on spasticity whereas Park et al. assessed its immediate effect.
5.6. Conclusion
According to the results of this study WBV can be considered as an effective treatment for increasing the range of motion and walking speed in cerebral palsy children.
5.7. Limitations
Our intervention lasted 6 weeks. In order to assess long lasting effect of intervention, future studies with larger sample size and longer follow-up periods are needed.