1. Background
Neonates born before 37 weeks of gestation are called premature infants (1). The statistics show that approximately 10% of infants (15 million yearly) are born prematurely throughout the world (2). The significant advances in neonatal care have increased the survival rate of premature neonates. However, the deaths from it are still high (3). About one-quarter of the premature neonates with 22 - 28 weeks of gestation die (4). Preterm labor was responsible for the death of 1 million neonates in 2015 (3). Preterm neonates comprise 70% of dead neonates (5). poverty, maternal age, obesity, nutritional status, maternal vitamin D deficiency and African-American race in USA are among the risk factors for early delivery (1). Vitamin D deficiency is common in neonates, children, and pregnant mothers (6). Vitamin D deficiency is defined as the deficiency of 1 and 25-hydroxyvitamin D (25(OH)D) in amounts of less than 30 ng/mL (7). Several studies have reported vitamin D deficiency in 40% - 94% of premature infants (8, 9). Vitamin D is a fat-soluble vitamin essential for the absorption of calcium from the intestine, thus playing an important role in the musculoskeletal function (10). Vitamin D deficiency during pregnancy is associated with an increased risk of developing maternal gestational diabetes, preeclampsia, recurrent abortions, as well as low birth weight (LBW), and intrauterine growth restriction (IUGR) of the fetus (1, 6), which can lead to preterm delivery (11). Vitamin D deficiency is common in premature neonates (12). which can be due to maternal vitamin deficiency and causes serious problems in premature neonates, such as increased risk of respiratory problems at birth, osteopenia of prematurity, bronchopulmonary dysplasia, increased risk of infectious diseases, reduced brain growth, seizures, growth disturbances, retinopathy of immaturity, brain hemorrhage, and death (13-15). Studies report the effect of vitamin D deficiency on the regulation of immune responses by generating an antimicrobial peptide pattern in epithelial cells, neutrophils, and macrophages and the lack of lung maturation by examining the specific vitamin D receptor (VDR), which is expressed in most tissues of the body, in terms of regulation, diagnosis, and differentiation of the cell in immature died premature neonates (15-20). Therefore, deficiency of this vitamin is one of the main challenges in the care of neonates (13).
In a study of 44 infants born before the 29th week of gestation, the average vitamin D level of the umbilical cord blood was 33.8 ng/mL in 41 survived neonates and 30.4 ng/mL in 3 dead neonates, and there was a significant difference between the two groups in the vitamin D level (14). Several studies have shown that respiratory distress, intraventricular hemorrhage, retinopathy of prematurity, and infections are more common in newborns with vitamin D deficiency (12, 13). On the other hand, the problems regarding neonatal morbidity and mortality have important effects. Therefore, vitamin D may be decreased directly or indirectly by increasing the mentioned problems or directly affect the prognosis of these neonates.
2. Objectives
Considering the results of various studies and the importance of different roles of vitamin D in neonates, this study aimed to compare the level of vitamin D in cord blood of the preterm neonates that survived and those that did not.
3. Methods
This is an analytical - cross-sectional study. The population under study consisted of 400 premature infants less than 34 weeks gestational age or of a birthweight less than 1800 grams admitted to the neonatal department of Ghaem Hospital in Mashhad during 2014 and 2018. Neonates with major anomalies and newborns of mothers taking anticonvulsants were excluded. The study was approved by the Ethics Committee of Mashhad University of Medical Sciences. Signed written informed consent was obtained from the parents of the neonates enrolled in the study.
A sample of 1.5 mL of complete blood was collected from each preterm infant’s umbilical cord, to assess serum vitamin D. The specimens were centrifuged and serum kept at -20°C until processed in laboratory. The serum vitamin D level was measured by ELISA method using an Elisa Reader model RT2100c (Germany) and Elisa washing machine. Vitamin D values < 30 nmol/L were considered as vitamin D deficiency. Vitamin D deficiencies were divided into severe deficiency (25-hydroxyvitamin D < 10 ng/mL), moderate deficiency (10 - 20 ng/mL), and mild (suboptimal) deficiency (20.10 - 30 ng/mL) (12).
Demographic characteristics of the newborns (age, birth weight, duration of oxygen therapy, the first-minute Apgar score, the fifth-minute Apgar score, and mechanical ventilation duration), neonatal laboratory findings (sodium, calcium, pH, Be, vitamin D, urea, and Cr), and the maternal information (age and gestational age) were recorded.
3.1. Statistical Analysis
To analyze and examine the relationship between the variables after normality control, independent t-test and for analyzing the relationship between variables with nominal scale chi-square test was applied. Analysis of covariance was used to control the variables gestational age, first minute and fifth minute Apgar score. The significance level was set at P < 0.05. Statistical analyses were performed with SPSS V. 21.0.
4. Results
Of 400 premature infants 17 neonates not meeting the criteria, were excluded. A total of 335 premature neonates survived and 48 infants died. Using the independent t-test, the results showed that there was a significant difference between the two groups in the first and fifth minutes Apgar scores, duration of oxygen therapy, and gestational age (Table 1).
| Variable | Groups | P Value | |
|---|---|---|---|
| Survived (N = 335) | Died (N = 48) | ||
| 1st min Apgar score | 6.1 ± 16.90 | 5.2 ± 53.24 | < 0.01b |
| 4th min Apgar score | 8.08 ± 1.40 | 7.18 ± 1.86 | < 0.01b |
| Gestational age, week | 31.2 ± 51.12 | 28.1 ± 61.87 | < 0.01b |
| Birth weight, g | 1320.314 ± 10.50 | 1034.297 ± 23.85 | 0.365 |
| Duration of oxygen therapy, day | 6.6 ± 52.55 | 11.90 ± 8 | < 0.01b |
| Vitamin D, ng/mL | 14.87 ± 10.94 | 9.4 ± 6.52 | < 0.01b |
| Na, mEq/L | 140.4 ± 21 | 139.2 ± 4 | 0.350 |
| K, mEq/L | 4.84 ± 0.74 | 4.77 ± 0.8 | 0.805 |
| Ca, mg/dL | 8.86 ± 1.1 | 8.72 ± 1.34 | 0.652 |
| Urea, mg/dL | 38.35 ± 18.52 | 56.30 ± 22.93 | < 0.01b |
| Cr, mg/dL | 0.75 ± 0.20 | 0.82 ± 0.22 | 0.221 |
| PT | 18.62 ± 8.26 | 19.49 ± 5.82 | 0.773 |
| PTT | 49.94 ± 22.96 | 86.90 ± 30.97 | < 0.01b |
| pH | 7.28 ± 0.12 | 7.28 ± 0.19 | 0.953 |
| HCO3 | 20.85 ± 4.31 | 20.6 ± 6.24 | 0.419 |
| BE | -100 ± 7.13 | 3.52 ± 9.14 | < 0.05a |
Mean and Standard Deviation of the Variables Studied in Two Groups of Premature Neonates Using the Independent t-test
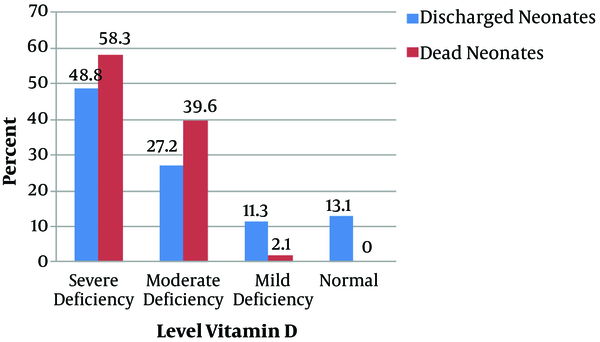
It was found that 339 (88.5%) of the premature neonates had vitamin D deficiency, of which 190 (49.6%), 110 (28.7%), 39 (10.2%) of cases had severe, moderate and mild deficiencies, respectively, and only 44 (11.5%) had normal levels of Vitamin D (Figure 1).
Fisher’s exact test showed that there was a significant relationship between the type of delivery and its outcome (P = 0.008) and Cramer’s test confirmed this relationship (P = 0.005), so that 21.3% of neonates born via normal vaginal delivery and 7.3% of neonates born via cesarean section, have died.
According to the chi-square test, there was a significant relationship between the levels of vitamin D and death and survival of neonates (P = 0.005). A total of 14.7%, 17.3%, and 2.6% of neonates who had respectively severe, moderate, and mild deficiencies of vitamin D died (Table 2).
| Variable | Groups | P Value | |
|---|---|---|---|
| Survived | Not Survived | ||
| Vitamin D | 0.005* | ||
| Severe deficiency | 162 (38.33) | 28 (58.33) | |
| Moderate deficiency | 91 (27.16) | 19 (39.58) | |
| Mild deficiency | 38 (11.34) | 1 (2.01) | |
| Natural | 44 (13.13) | 0 (0) | |
| Gender | 0.500 | ||
| Girl | 160(88.4) | 21(11.6) | |
| Boy | 159 (87.7) | 22 (12.2) | |
| Type of delivery | 0.008* | ||
| Normal vaginal delivery | 151 (45.07) | 33 (68.75) | |
| Cesarean section | 184 (54.93) | 15 (31.25) | |
The Frequency of Severity of Vitamin D, Gender, and Type of Delivery in the Survived and Not Survived Premature Neonatesa
Using covariance analysis with elimination of factors affecting the Gestational age, first minute Apgar score and fifth minute Apgar score, there still was a significant difference between the two groups of survived and not survived neonates in the serum level of vitamin D (P = 0.000). Therefore, vitamin D can be taken as a factor in prediction of neonatal survival rate.
5. Discussion
In this study, 88.5% of the premature infants had vitamin D deficiency, with almost half of them in a severe form. In a study published by Boskabadi et al. (13), vitamin D deficiency was reported to be 89%. Park et al. (9) found in 89.9% of preterm neonates a vitamin D deficiency, half of them showing a severe deficiency. Walker and Modlin (20) reported a mild vitamin D deficiency in 86% of neonates. The reason for this discrepancy in the level of vitamin D deficiency can be explained as follows:
The only source of vitamin D for embryo is its transfer from the mother, the amount of which depends on the maternal exposure to sunlight and the intake of a supplementation or foods containing vitamin D (21, 22). The level of 1,25-hydroxyvitamin D increases in the first trimester of pregnancy, reaching its peak in the third trimester (twice the non-pregnancy level). An increase in the serum vitamin D level in the mother leads to an increase in Vitamin D binding protein (23). The transmission of essential nutrients, including vitamin D, occurs in the third trimester of pregnancy; because premature neonates have lost this golden time, it is likely that they will be put at risk of having a vitamin D deficiency (1).
The studies by Vieth Streym et al. and Cadario et al. indicate that vitamin D deficiency is greater in preterm neonates (24, 25). Similarly, in a study by Burris et al., the results showed that the chance of vitamin D deficiency of below 20 ng/mL was doubled in premature infants of below 32 weeks of gestational age compared to neonates of 37 weeks (1). In a study by Choi et al., there was a significant relationship between infants born in the second trimester of pregnancy and severe vitamin D deficiencies compared to third-trimester neonates (26). Studies have shown that most vitamin D from the mother reaches the neonate in the last weeks of pregnancy (13).
The results of the current study indicate that the vitamin D level was about one and a half times higher in survived than in non-survived infants. Even by removing the effect of intervening factors (gestational age, first minute Apgar score and fifth minute Apgar score), vitamin D deficiency could predict the death of infants, which is consistent with the study by Yang et al. (27). In contrast to this, the studies by Joung et al. and Onwuneme et al., showed no relationship between the risk of death among succumbed premature infants and the level of vitamin D [(OH)-D] in the umbilical cord (14, 28). In these studies, all neonates had normal levels of vitamin D, but in our study, four-fifths of newborns had vitamin D deficiency. It is likely that the difference between the results of the current work and those of the two mentioned studies is related to the difference in geographical location, economic level, and gestational age. Searching in the available literature we found no study preoccupied with the association between vitamin D deficiency and mortality of premature infants. Although the main cause of this association was not determined, several studies have shown the role of vitamin D in other problems of premature newborns. Boskabadi et al. found that vitamin D levels were lower in preterm infants with respiratory problems (13). Because respiratory problems are one of the most common causes of hospitalization of premature newborns and their mortality, vitamin D deficiency may be effective in increasing the risk of death in premature newborns.
One of the most important causes of premature infant mortality is infections, accounting for 20% - 30% of the deaths of premature infants (29). Hence, vitamin D deficiency may contribute to increasing the likelihood of death of infants by increasing the susceptibility to infections. Several studies have also shown the impact of vitamin D deficiency on the regulation of immune responses by creating an antimicrobial peptide pattern in epithelial cells, neutrophils, and macrophages. There are also reports of lung non-maturation through examination of the nuclear vitamin D receptor (VDR) expressed in most body tissues, which contributes to cellular regulation, diagnosis, and differentiation in premature infants (15-20).
In this study, the Apgar scores of the first and fifth minute were significantly lower in newborns who died. In the study by Kim et al., the Apgar score of infants who had a mild deficiency level of vitamin D was higher than that of dead infants who had severe levels of vitamin D deficiency (30). It was also found that infants with severe vitamin D deficiency needed longer oxygen therapy (30). Vitamin D affects the relationship between endodermal and mesodermal cells that results in alveolar structure and lung maturation. Deficiency of this vitamin, followed by lung non-maturation, may cause the more need for oxygen therapy (14, 31).
One of the limitations of the current study was the lack of follow-up of surviving infants and its relationship with the amount of vitamin D at birth. In addition, we did not investigate the exact causes of death in these infants. Therefore, more studies are recommended in this regard with the consideration of multiple factors.
5.1. Conclusions
The results of this study showed that most premature infants had a severe vitamin D deficiency, and this deficiency was more pronounced in newborns who did not survive. It could be taken as a tool to predict the risk of non-surveillance in premature infants. Vitamin D deficiency may increase the likelihood of death of these infants by increasing respiratory problems and infections.